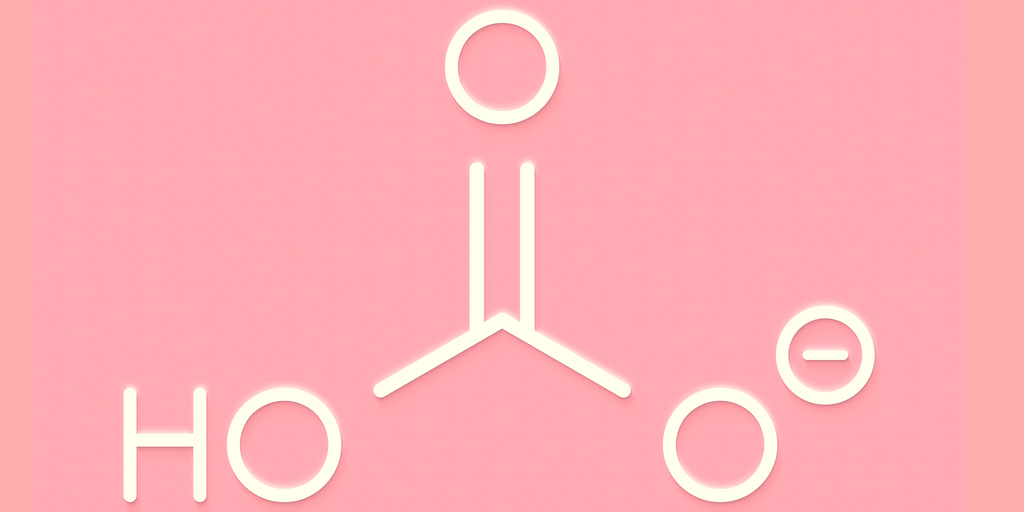
When should I use bicarb?

Every so often, when faced with a particularly unwell patient, one may find oneself tempted to inject baking soda into their vasculature.
Because if it makes cakes rise, maybe it'll do the same to a human.
Take home messages
- Salicylate and TCA toxicity - yes please
- Hyperkalaemia with risk of arrhythmia - yes please
- Severe normal anion gap acidosis - probably
- Super severe DKA or lactic acidosis - probably not
- Cardiac arrest - no thank you
The theory
It is a natural buffer that the body uses to counter a metabolic acidosis by mopping up pesky hydrogen ions and converting them to CO2 which can be easily and conveniently exhaled.
The reality
It's usually an accountancy trick - it fudges the numbers to make things look better than they really are.
Now I know what you're thinking - our entire job is just making numbers on a screen look better - and we're not disagreeing. We're just saying that sometimes, the numbers can be misleading.
When it's useful
- Hyperkalaemia with significant ECG changes
- Bicarb helps shove the potassium into the cells
- The sodium load helps stabilise cardiac membranes
- This temporises against impending fatal arrhythmias
You're not really fixing anything - you're just buying time while your actual treatment gets the job done.
- Severe normal anion gap metabolic acidosis (pH <7.1) with haemodynamic instability
- For example caused by fistulae or renal tubular acidosis
- There is a genuine deficiency of bicarb, which you can replace
- Normal kidneys will gradually replace it themselves, but it takes time
- You're also increasing the pH for a while to allow the struggling cardiac muscle tissue to function while you fix the underlying pathology.
- Specific toxidromes
- TCA overdose
- Salicylate poisoning
Here you're actually doing something meaningful.
By increasing the pH of the blood, you increase the affinity of albumin to bind the drug - so you increase protein binding and reduce the free fraction available to cause problems.
By alkalinising the urine, you 'trap' the drug molecules in the tubules and prevent them being reabsorbed.
When it's not useful
Cardiac arrest
- It doesn't improve survival
- It doesn't improve neurological outcomes
- It worsens intracellular acidosis
- It increases CO2 which you're probably already struggling to get rid of
Mild or moderate metabolic acidosis
- If the pH is above 7.2 then stop faffing about and just treat the underlying cause
- For lactic acidosis the problem is tissue hypoxia, which is usually better fixed with oxygen and more blood pressure
DKA
- Bicarb will distract you from actually treating the ketoacidosis
- Bicarb will increase the pH, and increase ketone production by reducing the inhibition on beta oxidation that occurs at low pH
- You'll make the patient even more hypokalaemic
So let's not.
Why it's bad
To start with, if you give loads you'll end up with
- Hypernatraemia
- Metabolic alkalosis
- Hypokalaemia
- Arrhythmias
- Volume overload
- Worsening intracellular acidosis
- Hypercapnoea*
*You have to be able to get rid of the extra CO2 that you generate, otherwise you've not achieved anything.
8.4% Bicarb contains 1mEq/ml, which is the same as 84mg/ml, or 0.05 mol in a 50 ml vial.
If administered to the patient, this then produces just over a litre of CO2 - more than you would exhale at rest in 5 minutes.
If you give bicarb to a patient on the ventilator, you'll see their end tidal CO2 jump substantially.
One last thing.
Note that 8.4% bicarb contains 1000 mmol of sodium per litre, and is as osmotically spicy as 6% saline at 2000 mOsm/kg so if you do insist on giving it, don't be doing it neat through a blue cannula on the hand please.
What the hell is a mEq?
- Milliequivalent
- It's a unit of measure often used for electrolytes
- It indicates the chemical activity, or combining power, of an element relative to the activity of 1 mg of hydrogen
- It's the number of mg of the molecule, divided by the molecular weight, then multiplied by the valence
- So 1 mEq of sodium contains 23 mg sodium ions because the atomic weight is 23 and the valence is one - 23 mg sodium ions has equivalent activity to 1mg hydrogen ions
1mg of hydrogen ions contains the same number of + as 23mg of sodium ions, because sodium ions weigh 23 times as much.
- However 1 mEq of magnesium would be 12 mg, because while the atomic weight is 24, magnesium has double the charge.
- Hence 1mEq of sodium bicarbonate - NaHCO3 - is 84 mg
Bicarbonate in overdose
This is the only time you definitely need to use it.
The two most useful cases that you need to know about are:
- Salicylate poisoning
- TCA overdose (and other sodium channel blockers)
Salicylate toxicity
Salicylate toxicity is complex and beyond the scope of a wee chat about bicarb, but know this - bicarb is really useful.
- Enhances urinary elimination of salicylate
- Reduces concentrations of salicylate in the target tissues
Salicylate is a weak acid, meaning it will ionise more in higher pH environments.
If you increase the pH of the blood, more free drug molecules ionise, and fewer can cross into the tissues to cause harm, particularly in the CNS.
Hooray.
When to give it
- Salicylate overdose with CNS or pulmonary symptoms
- Overdose plus substantial metabolic acidosis
- Some reckon you should just give it if their blood salicylate level is >300mg/L even if they're asymptomatic
Sodium channel blockers
Examples
- TCAs
- Type IA and IC antiarrhythmic agents (quinidine, procainamide, flecainide)
- Quinine
- Carbamazepine
- Cocaine
Sodium bicarbonate helps by doing two things as we mentioned before:
- Increases protein binding and reduces available free fraction of drug
- Provides a bolus of sodium ions to move through the sodium channels and out-compete the drug molecules
When to give it
- QRS > 0.10 seconds
- Ventricular dysrhythmias
- Significant hypotension
Bicarb in metabolic acidosis
When your patient is very poorly with a normal anion gap metabolic acidosis caused by their:
- Pancreatic fistula
- Renal failure
- GI losses
- Exorbitant volumes of intravenous NaCl
Then clearly you want to treat the underlying cause, and not just plaster over the cracks by making the blood gas printout look nicer.
However.
In a patient - with a normal anion gap metabolic acidosis - who is so critically unwell that their lactate is increasing and the pH is drifting south of 7.1 despite your best medical management, your focus needs to shift a little.
The priority is now improving the pH
Why?
You're already treating the cause, hopefully, but their body is still decompensating, most probably due to tissue hypoxia.
- This is because the cardiac output is rubbish
- And because the body's response to catecholamines is becoming more sluggish
- This is all because the pH is so low
So by fixing the pH, you improve myocyte function, vasopressor response and tissue oxygen delivery, and hopefully they start getting better.
They may also have just run out of buffer
A normal anion gap metabolic acidosis is literally a deficiency of bicarbonate, which the body then has to replace from the liver and kidneys - and this takes time.
So it's not a ridiculous suggestion to replace it with a top up.
I want to know about strong ion difference
Good, because then you can explain why normal saline makes you acidotic.
- Your blood does not want to be positive or negatively charged
- So all the + ions and all the - ions need to cancel out
- We don't measure all of them, just the sodium, potassium, calcium, magnesium, bicarb and the chloride
- Because we don't measure all of them, there is a difference between the measured positives and negatives
- Kind of like the anion gap - in fact the anion gap is literally the subset of the strong ion difference that ignores bicarb
- The vast majority of the strong ions (the ones that fully dissociate) are made up by sodium and chloride
- So the simple way to measure the strong ion difference is to compare the number of sodiums and chlorides
- So we should have approximately 40 more sodiums than chloride in the blood in a normal healthy patient
If we then whack in 154 sodiums and 154 chlorides to a patient who has 135 sodiums and 95 chlorides already, we have given proportionately way more chloride.
This reduces the strong ion difference, threatening to make the blood more negatively charged.
To counter this the body ditches negative bicarbonate ions in favour of positive hydrogen ions and the electroneutrality is maintained.
The pH, however, drops.
This is why you get a hyperchloraemic metabolic acidosis.
The saline isn't 'acidic' in it's nature, rather it's the effect its administration has on the strong ion difference that induces an acidosis.
Giving sodium bicarbonate simply reverses this process.
If you're thinking about giving bicarbonate to help fix a normal anion gap metabolic acidosis, then you can do the following:
- Take the sodium concentration and minus the chlorides
- Then take away another 10 from that number
- If the result is a number that would be a 'low' bicarb, then consider replacing
How should I give it?
We'll start by saying 'don't, until you've chatted with the ICU consultant responsible for answering difficult questions about this patient in court'
If they're happy, then:
- You want 150 mEq in a litre of 5% dextrose
- This is usually three 50ml vials of 8.4%
How much to give
- Take the base deficit (or negative base excess)
- Multiply it by their weight
- Multiply it by 0.3
That much.
You have to realise the implications
You can't just smash in some baking soda and feel terribly pleased with yourself, you need to consider the consequences of what you've just done.
- Their CO2 is going to skyrocket, so they need to hyperventilate a lot
- Their saturations are going to paradoxically improve (see below)
- Their albumin is going to have a renewed affinity for calcium, and they're going to go hypocalcaemic
- Their lactate is going to increase
Why does bicarb make their lactate go up?
- It unlocks more glycolysis
- Lactate is produced by glycolysis, the rate limiting step of which is phosphofructokinase
- This enzyme is inhibited by low pH
- Bicarb removes this inhibition by increasing the pH for a little while, allowing lactate production to ramp back up again
- It reduces oxygen supply to the tissues (see the box below)
I just gave bicarb and my patient's saturations improved!
Congratulations you just made them sicker.
- They probably had a degree of tissue hypoxia, because they're really sick and hence you're giving them bicarb
- Their oxygen dissociation curve was shifted way to the right, to offload as much oxygen to the tissues as possible
- Now you've come along with your fancy-pants bicarb, whacked the pH up a bit and shifted that curve to the left
- The free, mobile oxygen has then been hoovered back into the newly invigorated haemoglobin molecules, rather than being delivered to the dying tissues where it's needed
- So the numbers look better, but the mitochondria aren't happy
Make sure you're giving enough oxygen to compensate for this effect if you're going to use bicarb.
Why shouldn't I give it in DKA?
Because the evidence suggests it isn't justified.
The risks of giving bicarbonate in DKA are:
- Paradoxical CSF acidosis
- Hypokalemia
- Cerebral oedema
- Shifts oxygen-hemoglobin dissociation curve to left, decreasing O2 delivery to tissues
- Distracts you from actually fixing the problem by making you think you've fixed the problem.
Just hammer the patient with fluids, insulin, potassium and treat the infection or whatever is causing it.
If you can't mitigate these sequelae of giving bicarb, then you probably don't want to give it in the first place.
Also the 2018 BICAR-ICU study suggests it doesn't make a significant difference to important outcomes, so don't feel bad if you don't feel comfortable giving it.
Should I take bicarbonate for Wellness?

Here's our post on 'The Deeks'
Cool Tweets and References
Just look at how impossible it is to decide whether to use bicarb or not
Everyone likes to argue about bicarbonate. Looks like the signal is it could really help the response to vasopressor and we may not prescribe it enough by degree acidosis/weight https://t.co/oX9CTB4HoZ
— Joanna Poole 💙 (@jopo_dr@critcare.social) (@Jopo_dr) February 3, 2021
You've probably heard that Bicarbonate has to turn into CO2 to raise the pH. “Don’t give bicarb if you can’t increase ventilation.”
— Nick Mark MD (@nickmmark) May 14, 2023
But how much CO2 is there in an amp of sodium bicarbonate?
A bicarb 🧵
1/ pic.twitter.com/E06TseFU2V
🚨Sodium Bicarbonate in Critically Ill Conditions: From Physiology to Clinical Practice🚨
— SrivatsaNagachandan (@Srivatsa34) August 17, 2024
Part 1: Understanding the Complexities of Sodium Bicarbonate in Critical Care
🩺 Restoring Physiologic Balances
In the ICU, the goal is always to restore a patient’s physiologic balance… pic.twitter.com/0sBS0brDCw