Aortic Stenosis
Take home messages
- Aortic stenosis is bad news, causing increased perioperative mortality and morbidity
- Patients may benefit from aortic valve replacement prior to major elective surgery
- The aim of the game, as usual, is maintaining stable cardiac output
Podcast episode
We like flow
We anaesthetists are simple beings, and if there's one thing we want more than anything else, it's for our patients to have a solid flow of oxygen to the brain.
Clearly then, any obstruction to that flow is going to present problems, and these problems are generally amplified during an operation, just to keep the anaesthetist on their toes.
As you'll immediately remember from medical school, the three cardinal symptoms are:
- Angina
- Syncope
- Dypsnoea
And some other words you learned at medical school:
- Slow rising pulse
- Carotid thrill
Aortic stenosis doesn't generally come on all of a sudden, it builds gradually over many years.
The body is generally very good at compensating for slow-onset badness, and aortic stenosis is no different. So classically patients tend to have long periods of asymptomatic valve disease, followed by a rapid deterioration and development of symptoms.
Once symptoms do develop, the average life expectancy is then around two to three years, and that drops to 18 months if significant heart failure is present.
It's also more common in men.
Causes of stenosis
Rheumatic
Let's get this one out the way first. Yes, it's an important cause, but despite its popularity in textbooks, the cause is rarely rheumatic nowadays in the UK.
Do keep it in mind however if you're working in areas with diverse populations from a variety of backgrounds.
Degenerative
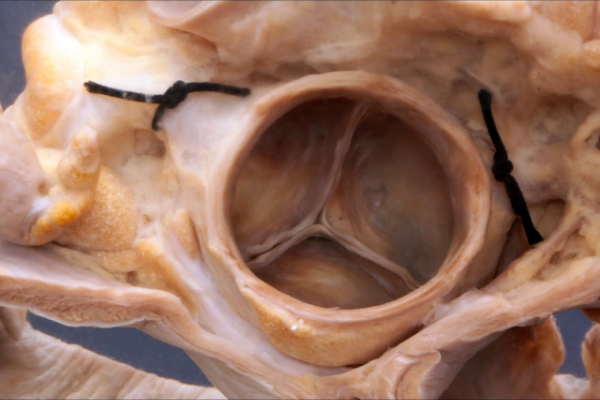
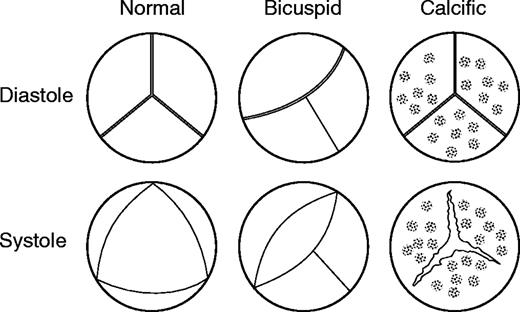
Degenerative calcific aortic stenosis of a previously normal tricuspid valve is the most common cause in UK, and usually occurs towards the age of 70. It will generally start as sclerosis, where the valve leaflets become thickened without any significant effect on heart function, and then progress to stenosis where blood flow is substantially affected.
What are the risk factors for degenerative calcific aortic stenosis?
- Diabetes
- Hypercholesterolaemia
- Smoking
- Hypertension
- Chronic haemodialysis
Congenital
Congenital bicuspid aortic valve is the most common congenital heart malformation, with around 2% of the population affected.
Two leaflets result in turbulent blood flow, which over a long time leads to thickening and fibrosis of the valve leaflets, usually showing up with symptoms between 30 - 50 years of age.
About half of patients under the age of 70 needing aortic valve surgery have a bicuspid valve.
Drugs
Drug induced valve disease was first associated with ergot alkaloids in the 1960s, and has since been linked to Parkinson's medications such as cabergoline, and recreational drugs including MDMA, however these are not specific to aortic stenosis.
Radiotherapy can also cause fibrosis of the valve leaflets and subsequent stenosis.
Others
As with anything in medicine, there's a group of rare other causes including Paget's disease, hypercholesterolaemia in children and ochronosis which are good to have up your sleeve for an exam question.
Why is it bad news?
The basic principle is very simple - there's a narrowing in the piping causing obstruction to flow.
In the same way an orange cannula is better for resuscitation than a pink, a narrow tube will limit the maximum flow rate of fluid, according to the Hagen–Poiseuille equation:
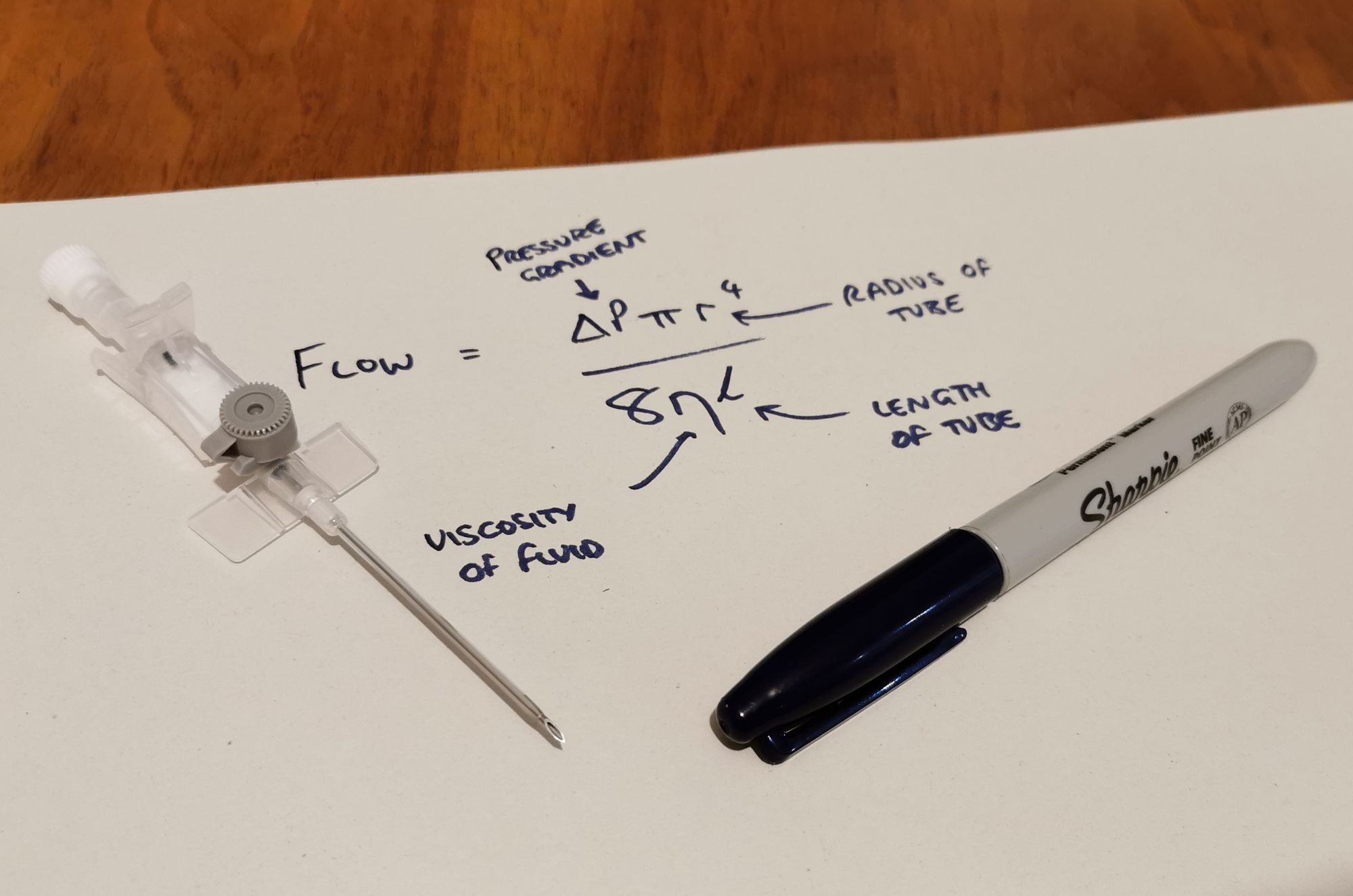
To begin with, the left ventricle just works harder to increase the flow, by driving a larger pressure gradient, and so it hypertrophies. However eventually it reaches a point where, even if the heart tries to pump even harder, the cardiac output is limited by the flow rate limit of the aortic opening.
Then you're left with a fixed cardiac output that is largely dependent on the rate of contraction, and you also have all the knock on detrimental effects of a substantially hypertrophied ventricle:
- Stiff myocardium with diastolic dysfunction
- Increased myocardial oxygen demand
- Reduced oxygen supply, as the reduced cardiac output provides a lower diastolic blood pressure, and therefore reduced coronary perfusion pressure
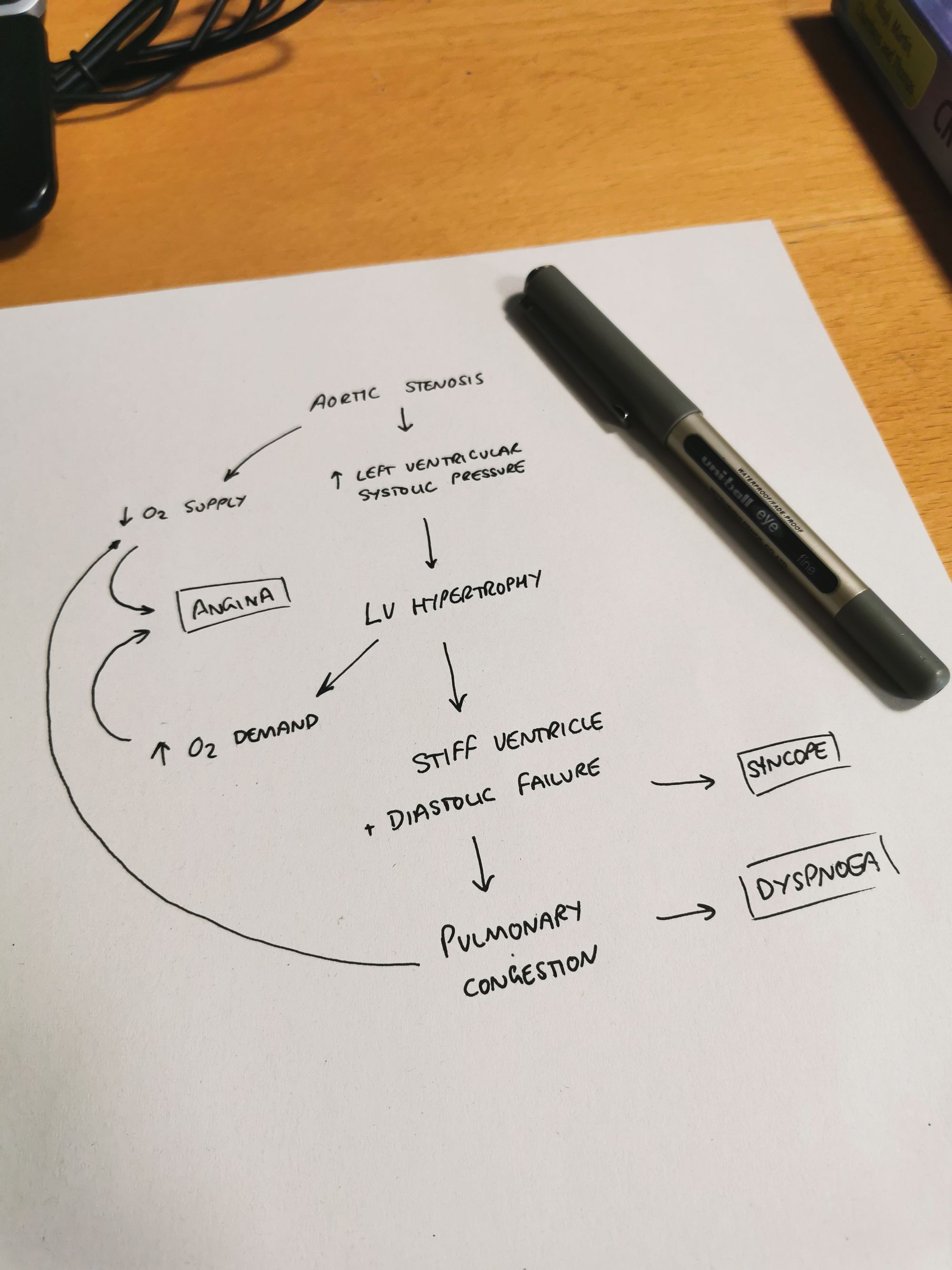
Aortic stenosis will therefore cause obstructive shock if it leads to inadequate perfusion of tissues.
What is normal aortic valve surface area?
- 2.6–3.5 cm2
At what valve surface area are haemodynamic effects seen?
- Approximately 1.0 cm2
Left ventricular dilatation is a very late, and therefore very bad sign, in aortic stenosis.
How does this affect my anaesthetic?
In lots of ways.
Sorry.
Preoperative priorities
- Get an echocardiogram beforehand, to establish the severity of the stenosis
- If you can't get an echo, and can't delay surgery, then assume it's at least moderate severity
- They might benefit from aortic valve replacement before any other surgery so it's worth discussing with their GP, the surgeon, and of course, the patient.
Intraoperative priorities
Lots of monitoring
- As always, start with the AAGBI required monitoring basics
- If the aortic valve area is less than 1cm2 or the gradient more than 30mmHg then invasive blood pressure monitoring is heavily advised
- Consider CVC for vasopressors/inotropes
- Consider trans-oesophageal echo
Note that pulmonary artery catheters are somewhat contraindicated as they can trigger arrhythmias
Maintain sinus rhythm
- The ventricular filling provided by atrial contraction is much more important in aortic stenosis, as it provides up to 40% of the stroke volume, compared to 20% normally
- Hence avoiding atrial fibrillation is very important, which is easier said than done, because the left atrium will hypertrophy over time in its efforts to fill a stiff left ventricle, and the physical distortion of the atrium can predispose to AF
Maintain a normal heart rate
Too fast
- You don't give the ventricle enough time to fill
- Huge increase in myocardial oxygen demand
- You don't have enough time in diastole to perfuse the myocardium
Too slow
- Cardiac output is largely rate dependent, so bradycardia leads to hypotension
- This reduces coronary perfusion pressure
Maintain blood pressure
- Early use of vasopressors to maintain systemic vascular resistance
- Think very carefully before using neuraxial blockade - vasodilatation due to spinal anaesthesia is tolerated very poorly
- Inotropes may be required but often contractility remains good due to left ventricular hypertrophy, as long as there's adequate preload and SVR
While this may seem obvious in any patient, it is particularly important to maintain a coronary perfusing pressure in aortic stenosis, as they are in a delicate balance between oxygen supply and demand, and can decompensate very quickly
Maintain preload
- Maintaining adequate filling pressure is essential to maintaining sufficient cardiac output
Also your ECG might be weird
Anatomically, your aortic valve is right next to your AV node, so it's fairly logical that substantial valve disease can have arrhythmogenic effects, and distort a normal ECG.
Findings include:
- Heart block
- Left axis deviation
- P wave enlargement
- ST depression and T wave inversion
- Features of left ventricular hypertrophy
How to fix aortic stenosis
Usually it ends up being a surgical problem.
What are the three surgical options for aortic stenosis?
- Surgical aortic valve replacement
- TAVI (transcatheter aortic valve implantation)
- Balloon valvuloplasty of the aortic valve (BAV)
Who might benefit from TAVI?
- Severe symptomatic aortic stenosis plus high risk for AVR
- or a contraindication to surgery*
*Including:
- Porcelain aorta
- Severe kyphoscoliosis
- Cirrhosis
- Mediastinal radiotherapy.
Useful Tweets
70 y/o 🧒🏻 lady, symptomatic aortic stenosis, initial mean gte 94 mmHg, ➡️ TAVR, pre and post dilations ✅ Final mean echo gte 5 mmHg, no PVL. #Structuralheart pic.twitter.com/Ggg4A2cCn2
— Oscar Millan-Iturbe (@ozkr_millan) February 12, 2023
References and Further Reading

Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
