Type I vs Type II Respiratory Failure
Type I respiratory failure is a failure to oxygenate
- Air may be moving in and out of the lungs appropriately, but the oxygen can't get across into the blood for whatever reason
- This causes hypoxia
- CO2 is super-soluble in water and usually has no trouble diffusing across into the lungs, so the CO2 is usually normal or even low, because the patient is hyperventilating to try and get as much oxygen into their blood as possible
- This is what we classically see in pneumonia and pulmonary oedema
- Type I respiratory failure can easily progress to type II failure, if left untreated and the patient becomes progressively more exhausted
Type II respiratory failure is a failure to ventilate
- This means you're not getting the air into the lungs appropriately
- As a result, there is hypercapnoea (too much CO2 in the blood) because it isn't being expired effectively
- The knock on effect is there is also hypoxia, because you're also not breathing enough oxygen in
- The primary problem to fix is the moving gas in and out of the lungs, rather than just giving more oxygen
Why does it matter?
If you are in type I respiratory failure, you need help with oxygenation, but if you are in type II respiratory failure, you need help with ventilation.
Just supplying more oxygen isn't going to help, if the problem is inadequate breathing. Sure, it'll improve the oxygen saturations temporarily, but the CO2 will continue to rise and the patient will become progressively more drowsy until they go unconscious and stop breathing altogether.
Check out this blood gas
- pH = 7.48 (7.35 - 7.45)
- PaO2 = 7.2 kPa (8 - 11 kPa)
- PaCO2 = 3.6 kPa (4 - 6 kPa)
Here you can see the oxygen levels in the blood are very low - there's an oxygenation problem, but the CO2 levels are also low.
This suggests that the patient is able to breathe the CO2 out, and is even hyperventilating in order to try and get more oxygen in, and as a result, the CO2 is lower than normal, causing a slight respiratory alkalosis.
For now this patient needs more oxygen, and doesn't require any extra help ventilating, but if this person gets tired, you'll start to see their ventilation get worse, their CO2 rise, and this will progress to type II respiratory failure.
Now look at this one
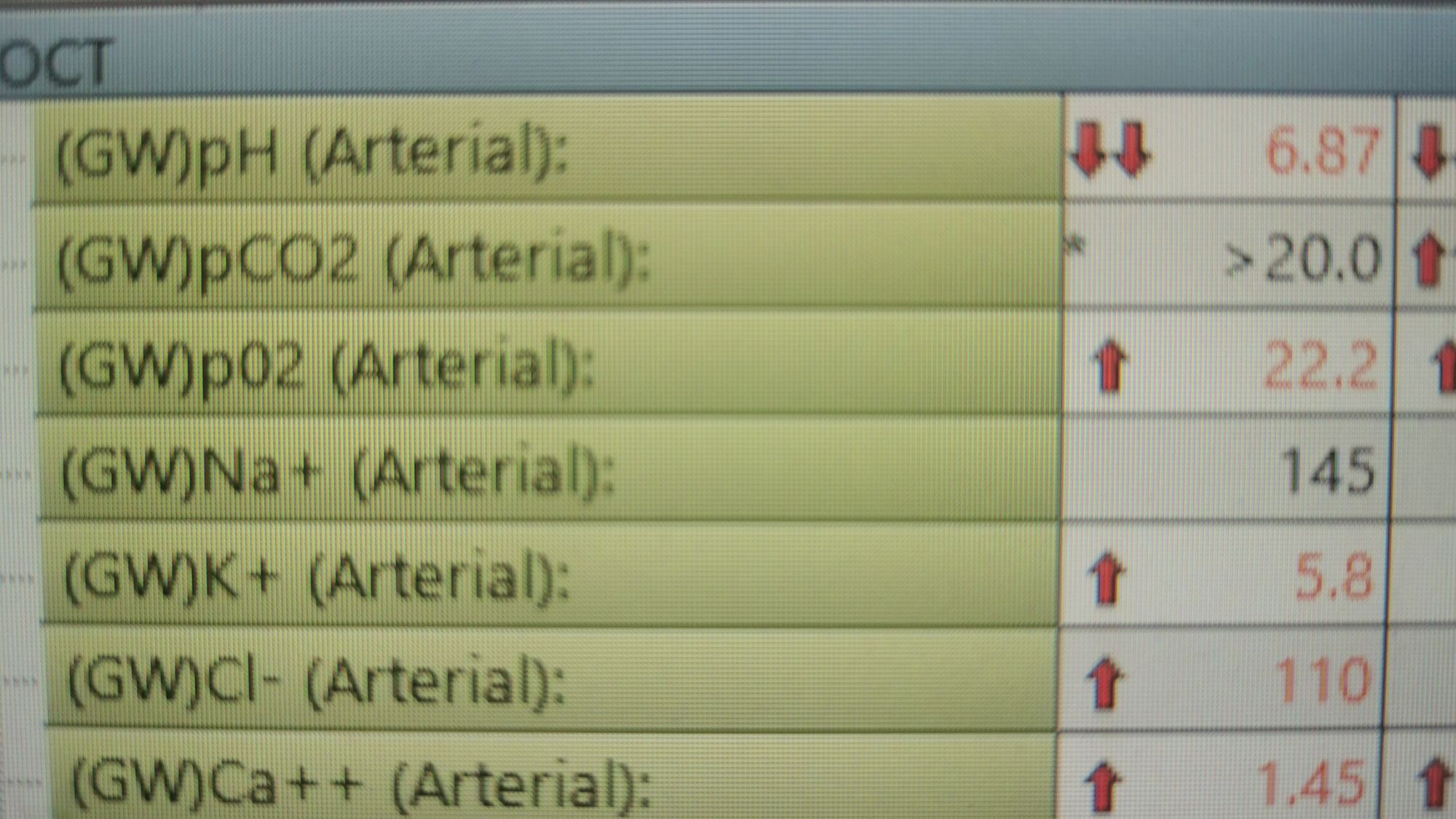
The patient is ridiculously acidotic - why? - because the CO2 is insanely high giving a respiratory acidosis, because they're not ventilating properly.
But look at the oxygen - it's high!
This patient has been given lots of oxygen, so their oxygen levels are pretty reasonable, but clearly the CO2 is a huge problem.
This patient was having a near fatal asthma attack, unable to breathe effectively due to bronchospasm and getting progressively more exhausted.
They managed to breathe in, and drag some oxygen into their lungs, but then when they tried to exhale, their small airways would obstruct and prevent any gas flow.
They could get the extra oxygen in, but couldn't get the CO2 out.
After having a nebuliser with 100% oxygen, they had trapped a whole load of pure oxygen in their lungs that they then couldn't exhale due to the severity of the bronchospasm.
The problem here is the patient cannot ventilate properly.
We intubated the patient and gave salbutamol, ketamine, magnesium, rocuronium and aminophylline and gradually the bronchospasm resolved. We supported the patient's ventilation for 24 hours and gradually the numbers on the blood gas all normalised.

Note the gradually improving carbon dioxide levels, and the accompanying improvement in pH
- The patient has more than enough oxygen throughout while on the ventilator, and as you can see we reduced how much oxygen we were giving to bring his PaO2 down to a more normal 16 kPa.
- Note also the potassium - salbutamol activates beta 2 adrenoreceptors in the lungs to cause bronchospasm, but this also activates the sodium potassium pump, which drives potassium from the blood into the cells, causing the potassium level in the blood to decrease.
- The glucose has also increased, most likely because we gave hydrocortisone, but potentially also because of a septic inflammatory response, and some of the medications are often given in dextrose rather than saline.
- The ionised calcium also appears to have dropped at the end - this might be due to the change in pH. At higher (more alkaline) pH, albumin is better at binding calcium, so the amount of free calcium in the blood drops. (This is why you get tingly fingers when you hyperventilate).
- The high lactate is most likely due to the large amounts of beta 2 receptor agonists that we were giving him at the start, as the levels normalised very quickly after that.
So how can I help with ventilation?
It's easy to give someone more oxygen, you just stick a facemask or nasal cannulae on and plug them in, but how can you help them to ventilate more effectively?
Simple stuff first
- Open the airway
This may sound silly but it's so important. Even something as simple as snoring can make ventilation ineffective, especially in patients with a low GCS due to trauma or overdose.
If you do a chin lift, a jaw thrust, or pop an airway adjunct in (oro- or nasopharyngeal airway) then you can open the soft tissues of the mouth and pharynx and allow much smoother air flow.
Often this is all that is required.
Stuff you can do on the ward
- Optiflow
This is just really fast, warmed and humidified oxygen and air via large nasal cannulae. The enormous rate (up to 60 litres per minute) helps to hold the nasopharynx open and help shove gas down into the patient's lungs, making it easier for them to draw in each breath.
- CPAP
Stands for continuous positive airway pressure
This is a tight fitting mask that just holds the upper airways open and helps prevent the alveoli from collapsing. It's very helpful in snoring patients with sleep apnoea.
Just note that it doesn't actively ventilate the patient - it doesn't drive air into their lungs - it just maintains a steady pressure for them to breathe against.
- BIPAP
Stands for bi-level positive airway pressure.
This is exactly the same as CPAP, but when the patient starts taking a breath in, the machine generates extra pressure to help drive the gas into their lungs, meaning it is a form of assisted ventilation.
Because it's via a facemask, rather than a tracheal tube, it is called non-invasive ventilation.
Stuff that needs ITU
- Intubation and ventilation
This is the last stop option, and requires the patient to be anaesthetised in order to tolerate having a tube between the very sensitive vocal cords.
The airway is secured with a cuffed endotracheal tube (the definition of a definitive airway) and connected to a ventilator.
The ventilator then drives gas in and out of the lungs, giving the patient's respiratory muscles a rest and allowing the oxygen to be used to recover from the original pathology.