Trigeminal Neuralgia
Take home messages
- Trigeminal neuralgia is the most common facial neuralgia
- Make sure nothing else is going on
- The first line treatment is carbamazepine
Podcast episode
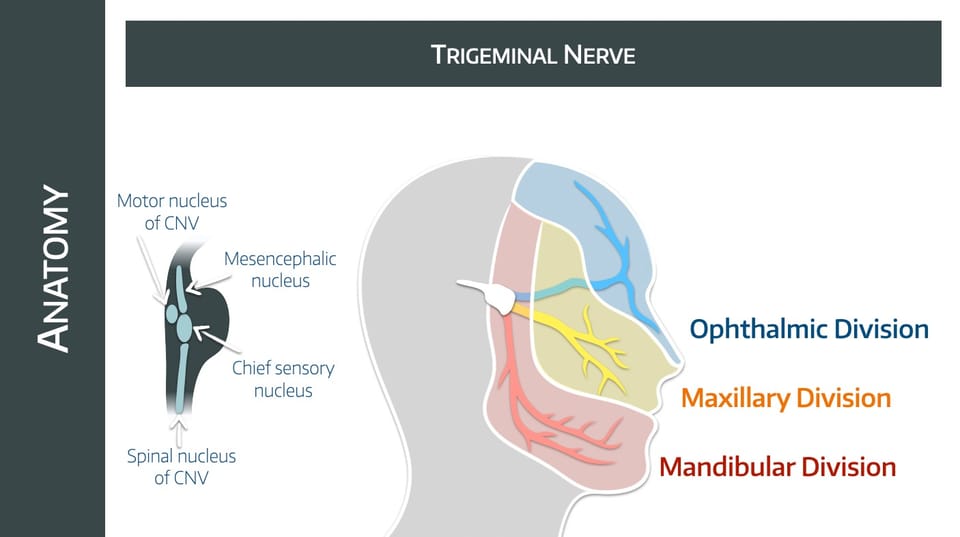
Some brief anatomy
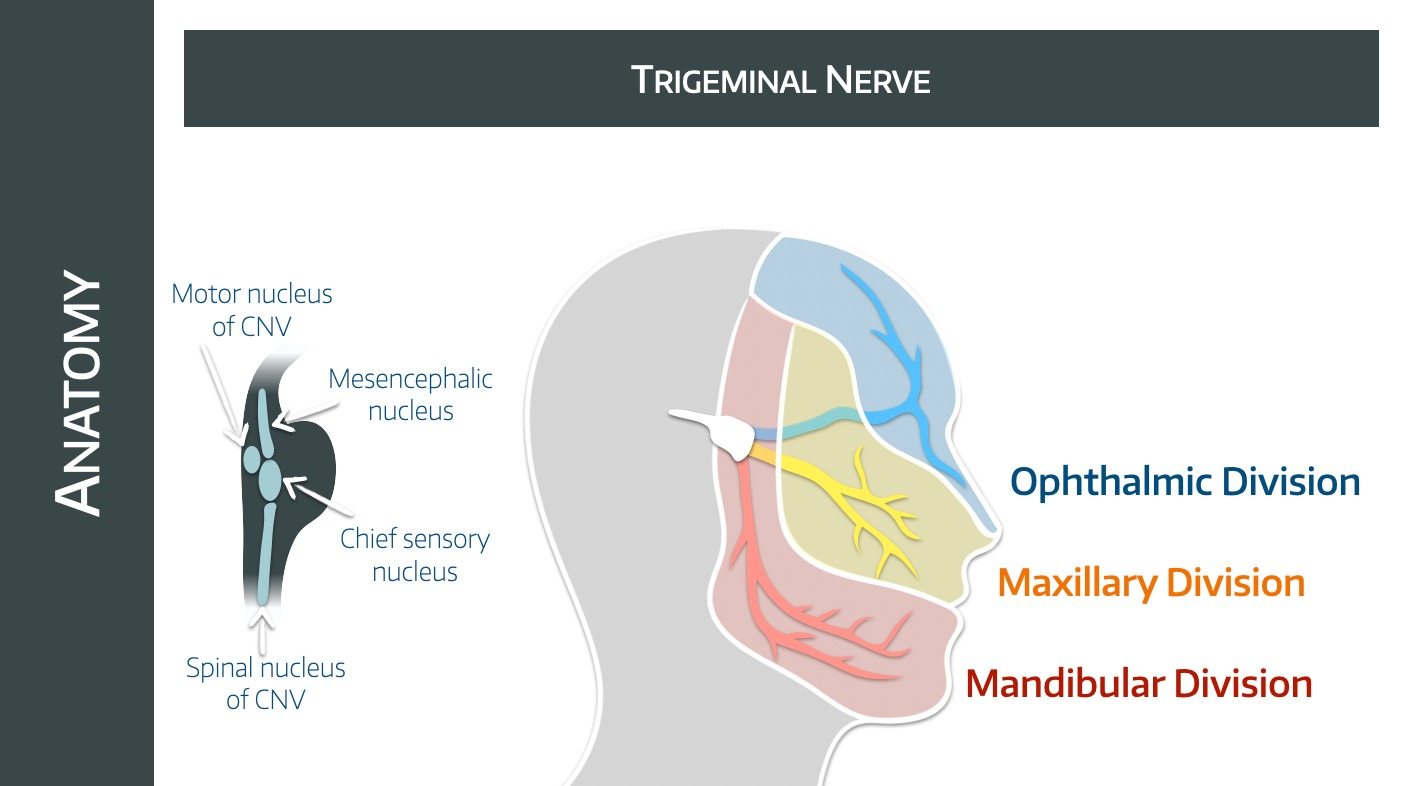
Tell me about the trigeminal nerve
- Cranial nerve number 5
- Largest cranial nerve
- Sensory and motor
- Paired nerve
- Starts at the lateral surface of the pons
- Sensory and motor roots are initially separate
- Sensory root forms the Gasserian or trigeminal ganglion in Meckel's cave in the middle fossa
- This divides into V1, V2 and V3
- V1 leaves through the superior orbital fissure
- V2 leaves through the foramen rotundum
- V3 leaves through the foramen ovale
- The motor root passes with V3
What are the functions of the trigeminal nerve?
The fifth cranial nerve does:
- Corneal reflex
- Sensation to the face over three divisions - forehead, cheek and chin
- Motor to masseter and temporalis muscles
- Autonomic supply to lacrimal, nasal, submandibular, sublingual and parotid glands, as well as the pupil
What we think happens
Nerves generally work very well indeed, as long as you don't hit them, burn them, cut them, marinade them in sugar or let them get infected.
If a pain nerve gets injured, it often gets hyperexcitable, meaning it will fire off pain signals inappropriately.
Fortunately you also have a central pain desensitisation system, which acts as a volume dial for these pain signals and can help make them less inappropriate.
But if you lose this central system as well, you're in trouble.
The trigeminal nerve has a vulnerable spot at the root entry zone, where the peripheral myelin provided by Schwann cells hands over to that provided by the central astrocytes.
Compression or damage at this point can cause aberrant pain signals to fire in response to even very light touch of the face.
Ephaptic coupling (if you care) is when nerves in very close proximity can actually induce and coordiate action potentials with each other, and we think it's this coupling of Aβ, A-δ and C fibres that gives you the pain response to a light touch.
What are the common triggers of trigeminal neuralgia?
- Chewing
- Talking
- Light touch
- Shaving
- Tooth brushing or washing the face
Sudden extreme pain can cause spasm of the facial muscles called 'tic douloureux'.
What happens in trigeminal neuralgia
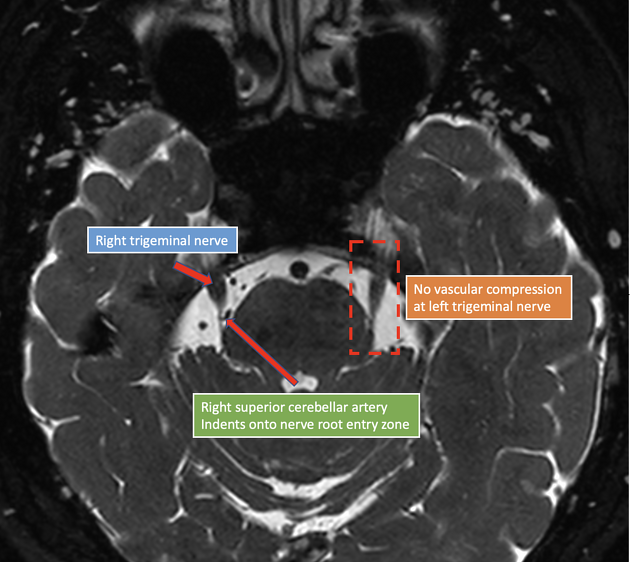
You get neurovascular compression of the root of the trigeminal nerve.
This happens at the root entry zone, usually by the superior cerebellar artery.
You need to see this compression on MRI to confirm the diagnosis.
You can also get the same thing with the glossopharyngeal nerve - glossopharyngeal neuralgia pain is generally felt in the ear.
Who gets it?
- 50-60 years old
- 3x more women than men
- Usually on the right hand side
- Usually V2 or V3 or both
What else could it be?
- Tumour - posterior fossa tumours, cavernous sinus masses
- Multiple sclerosis
- Epidermoid, dermoid, or arachnoid cysts.
- Aneurysm, or arteriovenous malformation
- Temporomandibular disorder
- Dental pain or abscess
- Cluster headache
- Salivary gland or sinus disease
Other -algias
- Trigeminal autonomic cephalgia
- Occipital neuralgia
- Glossopharyngeal neuralgia
- Post-herpetic neuralgia
Diagnosis
How is trigeminal neuralgia diagnosed?
- Paroxysmal attacks
- Severe pain
- Lasting seconds to minutes
- Affecting one or more divisions of the trigeminal nerve
Plus:
- Superficial, sharp or stabbing quality
- Triggered by specific areas or factors
- Always the same pattern for the individual (stereotyped)
- Not caused by anything else
- No neurological deficit
What are the red flag symptoms for a sinister underlying pathology?
- Sensory changes
- Deafness or other ear problems
- History of skin or oral lesions that could spread perineurally
- Pain only in the ophthalmic division of the trigeminal nerve (eye socket, forehead, and nose), or bilaterally
- Optic neuritis
- Family history of multiple sclerosis
- Age of onset before 40 years
What are you looking for on examination?
- Evidence of neurological deficit*
- Allodynia
- Hyperalgesia
- Hypoalgesia
*Trigeminal neuralgia very rarely gives you any motor symptoms, so weakness in the masseter or temporalis is suggestive of something else going on.
Which vessels are most commonly the cause of trigeminal neuralgia?
- Anterior inferior cerebellar artery
- Superior cerebellar artery
- Basilar artery
What investigations are indicated in suspected trigeminal neuralgia?
- Clinical examination including corneal blink reflex*
- MRI
*Blink reflex should be normal in trigeminal neuralgia
Tell me about carbamazepine
It's the first line treatment, and the only one that really properly works.
- It's a sodium channel blocker
- It works in a frequency-dependent manner
- It stabilises overexcited neural membranes
- It inhibits repetitive firing
- You give 200-1200 mg per day
Oxcarbazepine is an alternative - 300-1800 mg per day
What's not to love?
Well the number needed to harm is also quite high, around 3.5 for minor badness and 25 for major badness.
Badness includes:
- Dizziness
- Rash
- Ataxia
- Drowsiness
- Liver damage
But if it takes away the only pain ever considered worse than childbirth, one might decide it's worth putting up with these.
The other key things to monitor for are:
- Hyponatraemia
- Blood dyscrasias
So they need fairly regular blood tests.
Any other drugs?
Lamotrigine
400mg per day seems moderately helpful, usually given in combination with carbamazepine, presumably if carbamazepine can't manage on its own or increases in dose have been intolerable.
- Voltage gated sodium channel blocker
- Stabilises membranes
- Prevents release of excitatory neurotransmitters
- Can cause weird CNS stuff, rashes and SJS
Gabapentin
- 300-3600 mg per day
- Voltage gated calcium channel blocker
- Second line for trigeminal neuralgia
- Low quality evidence
Pregabalin
- 150-600 mg per day
- Not really very well tested
Baclofen
- GABA B agonist
- Used as an adjunct
Keppra
- a.k.a. Levetiracetam
- 3-4 g per day
- Binds synaptic vesicle glycoprotein SV2
- Modulates synaptic neurotransmitter release (which means we have no idea what it does)
Cannabinoids
The gift that keeps on giving - cannabinoids are becoming increasingly popular as a treatment for, well everything including trigeminal neuralgia
Any interventions?
You can inject botox, which can help for a few months, but can unsurprisingly give you motor side effects.
Otherwise there are four classes of surgical intervention, (which definitely do come up in the CRQ):
Microvascular decompression
- Most invasive but works the best
- Posterior fossa craniotomy
- Physically untangling artery from the nerves at the cerebellopontine angle
- Requires general anaesthesia and hospital admission
90% feel better and 80% will still feel better after a year
Stereotactic radiosurgery
- Also known as the awesome-sounding gamma knife
- Fires radiation at the trigeminal nerve root
- Can take up to 2 months before any relief felt
Over 50% have good relief at one year
Ganglion ablation
- The trigeminal ganglion is also called the Gasserian ganglion
- Can be ablated with radiofrequency or thermocoagulation
- Can also be injected with glycerol (chemical ablation)
- Can also squish it with a balloon
Clutching at straws here a bit - only really indicated if all the preceding options have failed.
Peripheral neurolysis
- Blast the distal nerves and hope the pain goes away
- Laser therapy
- Alcohol neurolysis
- Neurectomy
Long story short - if you're not coping on meds, and you are fit to do so, have the microvascular decompression.
What on earth is secondary trigeminal neuralgia?
It's the symptoms without the neurovascular compression, caused by something else - usually multiple sclerosis, in which case you'd see demyelination in the root entry zone.
Or at least the neuroradiologist would.
What are the other causes of secondary trigeminal neuralgia?
- Tumours (particularly at cerebellopontine angle, such as acoustic neuromas and meningiomas)
- Arteriovenous malformations
- Other space occupying lesions
The key to differentiating trigeminal neuralgia caused by MS from the classical type is abnormal reflexes.
- Blink reflex
- Evoked potentials
Both very useful for spotting MS as the underlying cause.
Unsurprisingly this doesn't respond nearly as well to carbamazepine etc but Gasserian ganglion blocks can still work, and if an AVM is causing the issue, microvascular decompression is an option.
So what is painful trigeminal neuropathy?
Good question.
A continuous facial pain... in the distribution of one or more branches of the trigeminal nerve... caused by something else
So it's basically exactly the same, but something else is causing it other than anything we've already listed above.
We're as confused as you are.
- It's generally a continuous burning pain rather than a stabbing intermittent attack
- There are sensory deficits including allodynia and cold hyperalgesia
- There are also three types
What are the three types?
- Trigeminal neuropathic pain due to herpes zoster infection
- Post herpetic neuralgia
- Post traumatic neuralgia (anaesthesia dolorosa)
There's more
Facial pain is an enormous subject, and we've consciously chosen to focus on what tends to be useful for the exam here, rather than a comprehensive review of the topic.
(You can answer the whole CRQ below using the information above.)
If you're keen to dive deeper into the weeds then check out the references below, and the FRCA questions in the members area at the bottom.
A free CRQ from revise FRCA
Our wonderful colleagues over at FRCA revision have kindly let us share some of their hand-crafted CRQs which you should definitely ensure you've seen before the exam.
Tap the image below for the trigeminal neuralgia question
Useful Tweets and Resources
Atypical facial pain in a Rheumatoid arthritis pt. Severe lancinating pain in the left V2 region. Rx as Trigeminal neuralgia without relief. MRI normal. Left TM joint crepitus O/e. CT -showed Flattening & destruction of the left mandibular condyle & erosion of the glenoid fossa. pic.twitter.com/qwxfXKrIoG
— Neurophilia (@bobvarkey) July 30, 2024

References and Further Reading



Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.