Thyroid and Parathyroid Surgery
Take home messages
- You can use either but TIVA is probably better
- Make sure you're really assessing their airway before you begin
- Be ready for the endocrine emergencies
Podcast episode
Respect the Thyroid
Unlike the -ologists, we anaesthetists don't really have an organ of our own, however the trachea is close to our hearts.
It's also rather close to the thyroid.
Depending on the surgery, this may be an issue for us, because whilst lopping off a little thyroid nodule might not cause us to look up from our crossword, removal of a large hormonally active retrosternal goitre causing tracheal compression does bother us a tad more.
Especially if they have to split the sternum to get to it.
We might even stand up.
‘Can the thyroid in the state of enlargement be removed? Emphatically experience answers no…every stroke of the knife will be followed by a torrent of blood and lucky…if his victims lived long enough for him to finish his horrid butchery. No honest and sensible surgeon would ever engage in it’
These are the words of Samual Gross in 1848, some four and a half thousand years after goitres were first described for the first time in China.
We've come rather a long way since then.
It gets examined
Anaesthesia for thyroid surgery has come up multiple times in the CRQ paper:
- September 2015
- September 2018
- March 2020
- September 2022
Probably because it's got interesting anatomy, endocrine physiology and airway management all crammed into one.
So of all the topics to revise, it's probably a good one to devote some attention to.
Some Primary Revision
This can come up in the Final, so we'll run through it briefly.
A very brief summary of the thyroid
- Endocrine organ weighing 25g
- Situated in the anterior triangle of the neck bilaterally
- Two lobes and one isthmus overlying the third tracheal ring
- Occasionally has a central pyramidal lobe as well
- Produces thyroid hormones and calcitonin
- Follicular cells secrete T3 and T4
Can you describe its blood supply and innervation?
Blood supply
- Superior thyroid artery from external carotid
- Inferior thyroid artery from subclavian
- Superior, middle and inferior thyroid veins
Innervation
- Recurrent laryngeal nerve
- External laryngeal nerve
How does it make thyroid hormones?
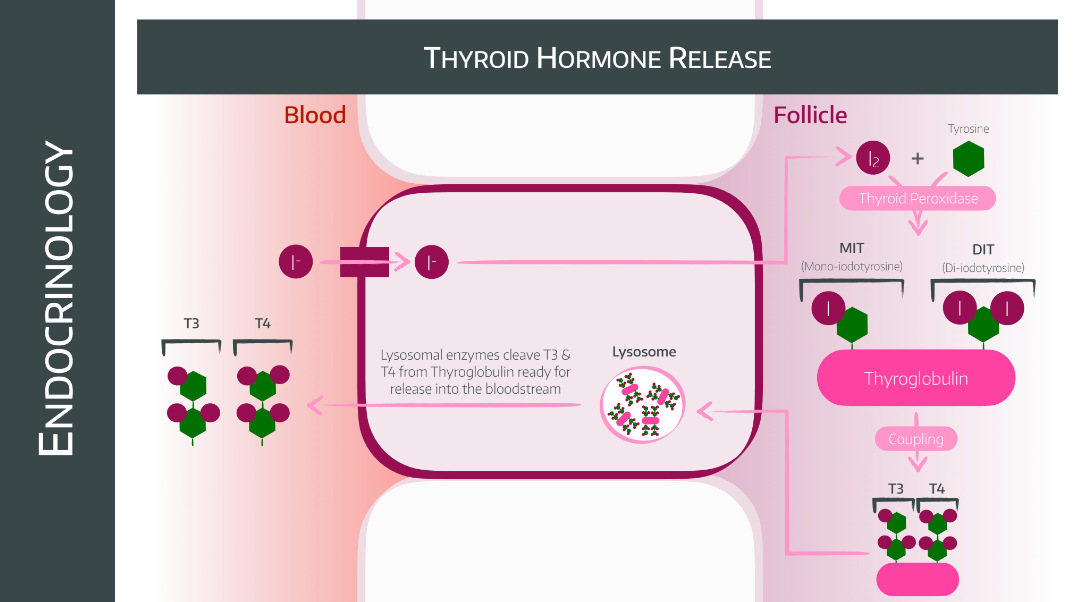
- Step 1 - Iodide uptake - Active transport into follicular cells via sodium/iodide cotransporter, stimulated by TSH
- Step 2 - Iodide oxidation - Oxidised by hydrogen peroxide to iodine, stimulated by TSH
- Step 3 - Iodine reaction with tyrosine - Tyrosine from thyroglobulin reacts with iodine to produce monoiodotyrosine (MIT) or diiodotyrosine (DIT)
- Step 4 - Oxidative coupling - Two DIT molecules produce T4, and MIT couples to DIT to form T3 - also stimulated by TSH
What do the thyroid hormones do?
- Modulate the body’s metabolic rate
- Increased metabolic rate
- Increased oxygen consumption
- Increased carbohydrate absorption from the GI tract
- Increased lipolysis
- Increased production and sensitisation of β adrenoceptors, causing increased sensitivity to adrenaline and noradrenaline
Tell me a bit about calcitonin
- Polypeptide hormone
- Produced by Parafollicular or C-cells in thyroid
- Released in response to hypercalcaemia
- Acts to reduce plasma calcium concentration
- Inhibits GI absoption of calcium
- Inhibits renal calcium and phosphate reabsorption
- Inhibits osteoclasts
- Hence it is used to treat osteoporosis and Paget’s disease
Preoperative considerations
Your main question - as usual - is 'how hard is this tube going to be'?
But you're also going to have to think about a few other issues that are a little different from your standard general anaesthetic for something like a laparotomy
Preoperative considerations
- You need to ask about positional dyspnoea
- You need to assess for recurrent laryngeal nerve palsy
- You need to assess for tracheomalacia if there's a long history of goitre
- You need to ask about their other comorbidities
- You need to know their thyroid function test results and ensure they're as euthyroid as possible before you start
Let's be honest, you probably need a CT scan too.
What are the symptoms of a large goitre?
- Positional dyspnoea
- Dysphagia
- Stridor
- Hoarseness or change in voice
What examination features are of relevance?
- Pulse - tachycardia, atrial fibrillation
- Mallampati
- Patil's test (thyromental distance)
- Jaw protrusion
- Texture of goitre - hard = malignancy
- Tracheal deviation
- Stridor
- Neck movement
- Retrosternal spread (can you palpate below the goitre)
- SVC obstruction (Pemberton's sign)
What investigations should be performed for thyroid surgery?
- FBC
- Electrolytes
- Corrected calcium level
- Thyroid function tests
Imaging
- Chest xray - tracheal deviation/narrowing
- Lateral thoracic inlet views - (to view retrosternal extension, but largely replaced by CT now)
- CT - retrosternal extension, airway compromise
What the thyroid might throw at you
Thyrotoxicosis
- First of all, use a calculator like this one to work out whether you're looking at thyroid storm or not.
- In an emergency you can use plasmapheresis to normalise thyroid hormone levels
Hyperthyroidism
- Patients should ideally be controlled and euthyroid prior to surgery
Hypothyroidism
- Emergency surgery for severe hypothyroidism requires a loading dose of levothyroxine 200-500 microgram IV
- Then they need 50-100 microgram daily
- Liothyronine can be used in myxoedema coma
- Remember steroids if there is adrenal insufficiency as well
Imaging
If someone is having thyroid surgery they definitely need a chest xray for starters. This will allow for an initial assessment of tracheal position, lung expansion as well as highlighting any other chesty pathologies that might be lurking beneath the distraction of a big thyroid.
Fibreoptic nasendoscopy can also be done to have a dress-rehearsal look at the larynx before attempting to intubate for real.
As always, for a predicted difficult airway, you should strongly consider awake fibreoptic intubation
How to anaesthetise them
The answer to this question never changes - general or regional
Regional anaesthesia
- Not really done in the UK
- Deep and superficial cervical plexus blocks
- With or without sedation
There is clearly a relatively narrow cohort of patients who will tolerate this, either psychologically or physiologically.
General anaesthesia
- TIVA or volatile
- TIVA might be better for shared airway surgery with potentially difficult intubation, as it takes the worry about adequate anaesthesia out of the equation
- Remifentanil is pretty perfect as it gives powerful pain relief, blocks laryngeal reflexes and also helps provide the low blood pressure needed by the surgeon
- Halogenated agents seem to affect intraoperative neuromuscular signals more
Induction
- You can do it the conventional way, usually with the patient sat up a little to relieve some of the tracheal compression
- You can do awake fibreoptic using your standard technique
- You can do gas induction to keep them breathing and maintain muscle tone if severe stridor
- You can go straight for tracheostomy under local (by the surgeon please, not you)
If you do intubate in the conventional manner, and are using a NMT tube, then you're more likely to land the electrodes in the right place with a videolaryngoscope.
Paralysis
- Makes intubation easier, but messes with intraoperative nerve monitoring
- Suxamethonium was the classic answer, having worn off by the time you need to monitor the recurrent laryngeal nerves
- Now you can use rocuronium and give sugammadex
- Atracurium seems to give good intubating conditions and doesn't seem to affect nerve monitoring significantly
What are the risk factors for difficult airway management in thyroid patients?
- Male
- BMI >30
- Neck circumference >40cm
- Signs and symptoms of tracheal compression
- Goitre
- Tracheal deviation
- Mallampati 3 or 4
- Interincisor distance <4.4 cm
- Thyromental distance <6.5 cm
- Neck circumference to thyromental distance ratio of >5
Logistics
If you've been in theatre for head and neck cases, then you've probably noticed a few of the following differences when compared to something like a laparotomy:
- The head's at the other end, miles away from the anaesthetist
- The breathing circuit is really long
- The IV lines have extensions
- There's loads of padding on the patient's eyes and face
- The tube is usually reinforced and taped rather than tied
- Often they'll use an NMT tube as well
- There's slight head-up positioning with an extended head in a head ring
- There's a shoulder roll or sandbag behind the scapulae
All of these have scored points in exam questions in the past.
The key points about neuromonitoring
- The tube has electrodes on the side, that sit abutting the vocal cords
- The surgeons then map the activity of the recurrent laryngeal nerves via their action on the vocalis muscles
- It requires good communication between anaesthetic and surgical teams about what muscle relaxant is on board and whether there are any concerns about tube position
Extubation
While extubation is rarely given the same respect, quiet or attention as intubation, it is exceptionally important in neck surgery where the field of play may have changed over the course of the procedure.
- Bleeding
- Swelling
- Nerve damage
- Tracheomalacia and tracheal collapse
All of these can make taking the tube out substantially more tricky than when it went in, but fortunately there are a few things you can do to make it a bit easier.
Extubation considerations
- Dexamethasone at induction to reduce swelling
- Regional and local anaesthesia to reduce the need for IV opioids
- Ensure the patient is wide awake and breathing spontaneously prior to extubation
- Deflate the cuff slowly and ensure a leak is present before removing the tube
It almost certainly won't score you marks on the exam paper but you can also consider intracuff lidocaine
A bit about the parathyroids
There are four of them, and they play with calcium.
- The most frequent indication for parathyroid surgery is primary hyperparathyroidism due to an adenoma
- This causes hypercalcaemia, and all the 'bones, stones, groans etc' symptoms that you remember from third year med school
Most will have a single adenoma with curative resection, and with new technetium-99 sestamibi scanning we are now much better at ensuring we get all the diseased tissue out.
Post op considerations
There are a few things you need to be thinking about once you've extubated your patient:
- Where should this patient go next?
- How do I manage their pain?
- What complications might crop up?
Pain
Digging around in the neck can look rather barbaric however thyroid surgery is apparently less painful than you'd expect.
What are my pain control options?
Preoperative
- Paracetamol 1g
- Ibuprofen 400-800mg or other NSAID*
- Gabapentin 1200 mg
Intraoperative
- Regional anaesthesia (superficial cervical plexus block)
- Remifentanil infusion
- Ketamine 0.25 - 1 mg/kg
- Dexmedetomidine infusion (up to 1.2 mcg/kg/hour)
- Lidocaine (up to 1.5mg/kg IV, but caution if using other local anaesthetics)
Postoperative
- Regular simple analgesia
- NSAIDs*
- Opioids
- PCA
*Avoid in renal failure etc etc....
Bilateral recurrent laryngeal nerve palsy
So this one's fun - you whip the tube out and the patient develops immediate stridor and respiratory distress because both recurrent laryngeal nerves aren't working.
You need to reintubate, and this is difficult.
Err, that's it.
Hypocalcaemia
If for some reason the parathyroids get irritated, impaired or obliterated during the procedure, then calcium is likely to present a bit of an issue, hence we measure it closely after any major neck surgery.
Up to around 20% of patients who've had a large goitre removed will have a transient hypocalcaemia.
What do I do about hypocalcaemia?
Prophylaxis
- 0.5-1.25 mg calcium 2-3 times per day orally
- 0.25-0.5 micrograms calcitriol twice a day
Treatment of mild to moderate hypocalcaemia (<0.85)
- 1-3 g calcium per day orally in divided doses
- 0.25-0.5 micrograms calcitriol twice a day
Treatment of severe hypocalcaemia (<0.7)
- 3-4 g calcium per day orally in divided doses
- 0.25-1 micrograms calcitriol twice a day
- Calcium gluconate 2g IV bolus plus infusion
If it's not getting better quickly, you need to be talking to intensive care.
The dreaded haematoma
You usually get told about these fairly on in an anaesthetic career, but hopefully won't find yourself having to manage one alone for a few years at least.
Thyroids are rather vascular, and can bleed after an operation, especially if the blood pressure was low during the procedure and didn't 'test' the surgeon's haemostatic skills all that thoroughly.
Remember the four benevolent Daleks:
Signs of a haematoma causing impending airway compromise
- Neck swelling
- Respiratory distress
- Stridor
- Desaturation
- Dysphagia
- Distress
What to do about it
Well, you SCOOP it out of course.
- Skin exposure
- Cut the subcuticular stitches
- Open the skin
- Open the strap muscles to expose the trachea
- Pack the wound after scooping out any blood
Which patients are allowed day-case surgery for endocrine neck stuff?
- Low risk of post operative bleeding
- Properly informed consent
- Written and verbal instructions about postoperative bleeding
- Easy and rapid access to hospital if stuff goes wrong
A free CRQ
From our lovely colleagues over at FRCA-revision.com
Useful Tweets and Resources
How to deal with a challenging, potentially life threatening post op (thyroid/parathyroid surgery) haemorrhage:
— British Journal of Anaesthesia (@BJAJournals) August 13, 2024
''OXYGENATE AND EVALUATE, EVACUATE AND INTUBATE''#BJAEd article by Drs Guzzetti, Inversini + @ABacuzzi https://t.co/fg1WY2e95e
Valsalva maneuver
— I USE THIS ACCOUNT FOR SELF STUDY & MY OPINIONS 📚 (@Theo_Alaistaire) February 1, 2023
- topic I always weak at
-4 phases
- changes diabetic autonomic dysfunction , cardiac failure
- consideration intraop for valsalva when surgeon request ( Thyroidectomy)#anaesthesia #anesthesia #intensivecare#physiology
Picture source : Googled Images. pic.twitter.com/LBGChxDyzg
References and Further Reading
Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.