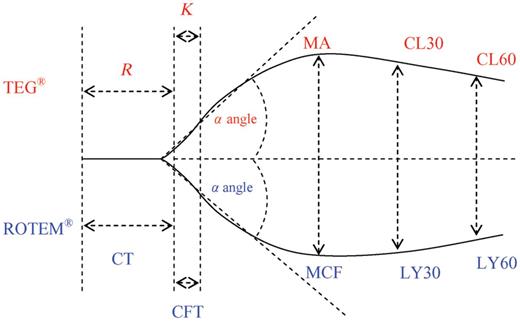
TEG and ROTEM
Take home messages:
- TEG (thromboelastography) and ROTEM (Rotational thromboelastometry) are slightly different variations of the same thing
- Both are rapid point-of-care tests of the viscoelastic properties of clot formation of whole blood
- They can be used guide immediate management of bleeding disorders and haemorrhage
- They can't detect hypothermia or hypocalcaemia as causes of coagulopathy
- They're pretty cool, and becoming increasingly commonplace
- It gets examined a lot in the FRCA Final exam
How does it work?
A small amount (like - 300 microlitres small) of whole blood is put in a little cup, warmed to 37°C, and a pin is suspended into the blood.
Then either the cup or the pin rotates, depending on whether you're using TEG or ROTEM, and the blood starts to clot.
As the blood clots, it starts to exert a twisting force on the pin.
Clearly, the stronger the clot, the larger the forces, and the quicker the clot forms, the sooner these forces will start to act on the pin.
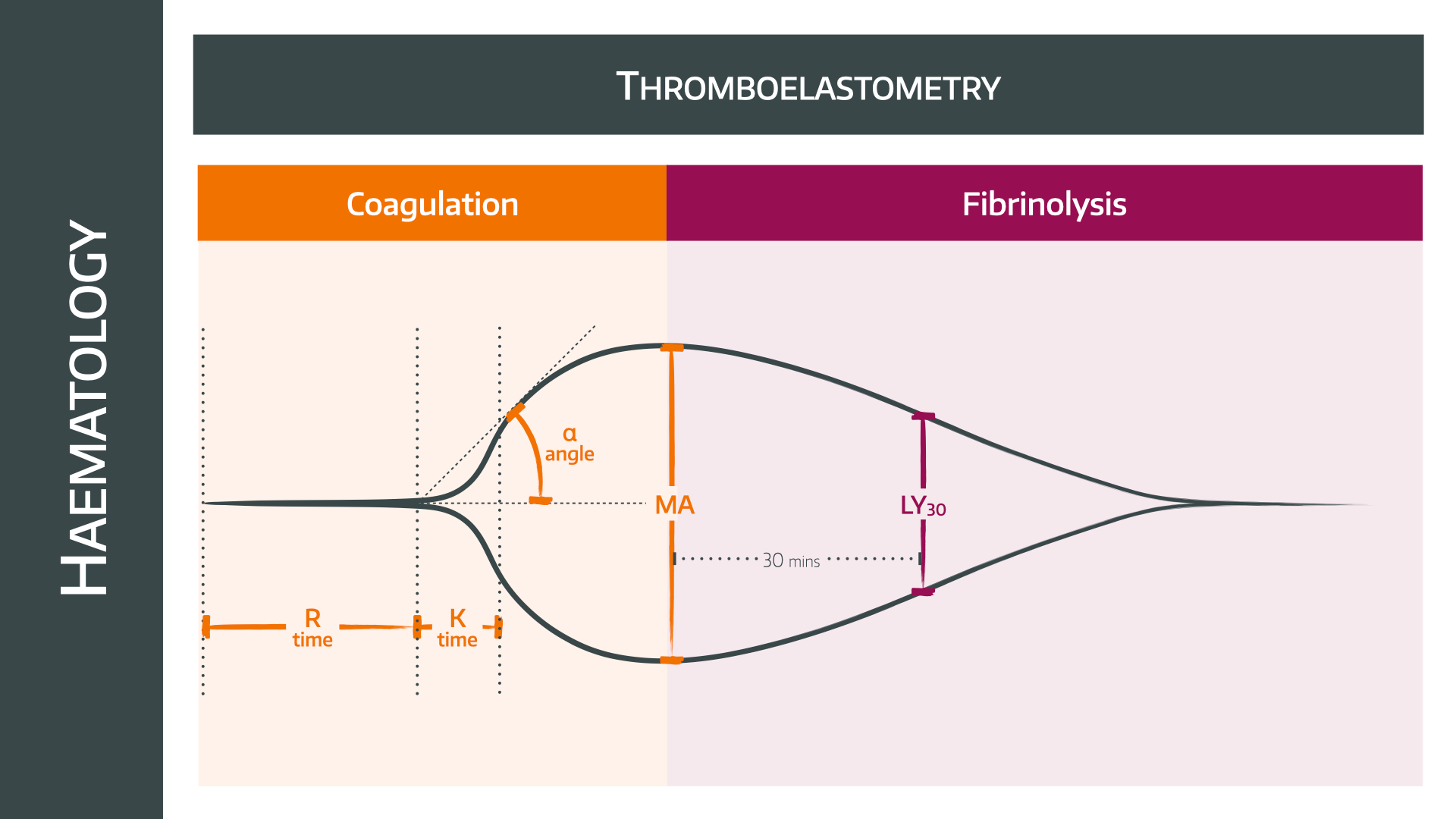
If you then transduce these forces into an electrical signal and chart it as a graph, you get a trace like this
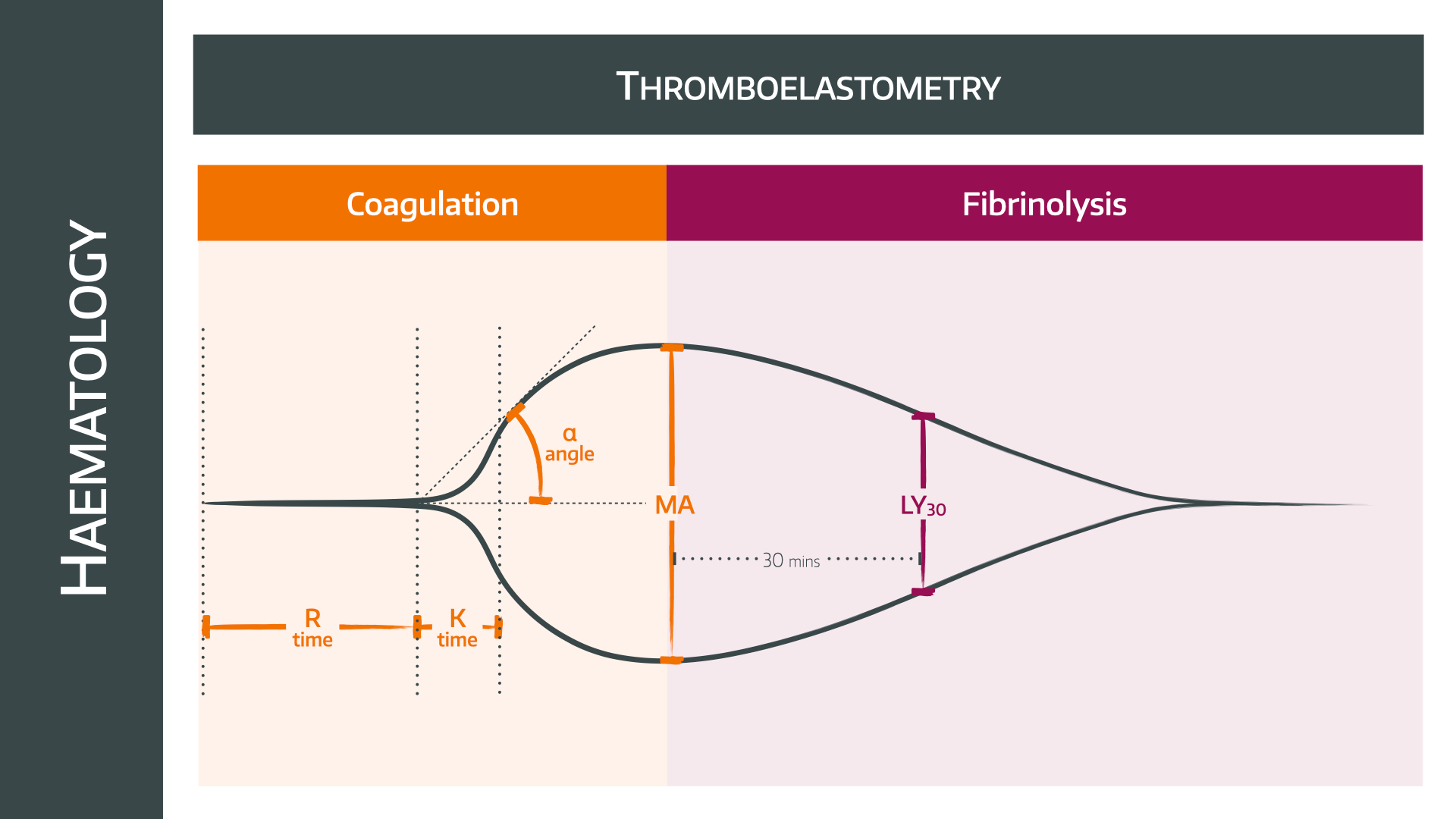
Technically it takes upwards of 30 minutes to get a complete graph to form, but in reality you get some very useful information to guide your management within a few minutes, making it a very handy piece of kit in a major haemorrhage emergency scenario.

What do the numbers mean?
It is important to know that TEG and ROTEM have different labels for the same things, because why make it easy for us?
Here we're using the TEG parameters, which are most commonly examined.
The R Time
- Time from when test starts, to when clot starts to form
- Normal is 5-10mins
- Determined by clotting factors
- If prolonged, give FFP
For ROTEM this is clotting time
The K time
- The time from the beginning of the clot forming, until the width or deviation of the graph is 20mm on the screen
- Normal is 3-5mins
- Determined by fibrinogen
- If prolonged, give cryoprecipitate
For ROTEM this is clot formation time
The alpha angle
- This tells you the rate at which the clot is forming
- Normal is around 50-70 degrees
- Determined again by fibrinogen
- If lower then give cryoprecipitate
This is the same in ROTEM
The maximum amplitude (MA)
- A measure of how big the clot gets
- Normal is 50-70mm
- Determined largely by platelets
- Unsurprisingly - Give platelets if low
For ROTEM this is Maximum Clot Firmness
CL30 or LY30 (lysis at 30 mins)
- A measure of how rapidly the clot is breaking down
- Should be less than 8% by 30 minutes after maximum amplitude
- If more than this, give tranexamic acid
TEG is CL30, ROTEM is LY30
Is it any good?
Yes.
In short, it provides rapid useful advice that you can use to tailor your management of a major haemorrhage in a more scientific way than guessing which products you haven't given enough of yet.
Of course it has limitations and equipment can always fail or need re-calibrating, and a single test result should never be used in isolation to guide your clinical management.
But in essence - it's a seriously cool bit of kit
Useful Youtube video
Useful Tweets
If you don't already follow @OnePagerICU on twitter, do. It's unbelievably high value information beautifully presented. Onepagericu.com
Today's ICU #OnePager is #thromboelastography (TEG) a rapid, useful way to assess coagulation & clotting to guide therapy in the ICU:
— ICU OnePager (@OnePagerICU) May 13, 2022
Prolonged R --> FFP
Decreased α angle --> cryo
Decreased MA --> Plt transfusion or enhance Plt fxn (ddAVP)
Increased LY30 --> TXA or amicar pic.twitter.com/ECim8I791N
And here's a cool tweet about using TEG in cirrhosis.
PulmCrit Minute- Using thromboelastography (TEG) to guide product transfusion in cirrhotic coagulopathy
— 𝙟𝙤𝙨𝙝 𝙛𝙖𝙧𝙠𝙖𝙨 (he/him) 💊 (@PulmCrit) June 17, 2019
(full post here: https://t.co/YSxAj1WNa4) pic.twitter.com/hXDa2G56AF
This is useful too
https://www.bsuh.nhs.uk/library/wp-content/uploads/sites/8/2021/12/ROTEM-interpretation.pdf
References and Further reading: