SVT and Tachyarrhythmias
Take home messages
- Shock needs a shock
- Be vary cautious with your sedation
- Don't get sucked into ownership of the cardiovascular management
ABC
In our line of work we usually see a tachycardia in the context of an emergency, during an operation or when another medical professional has asked us to come and help out.
So we'll start with the resuscitation approach for a patient where the only thing you know is:
"Help, they've got a really fast heart rate."
I'm going to be completely honest here, my approach to a weird heart rhythm looks a bit like this:
- Give oxygen if they need it
- Check the blood pressure and wheel out the defib if it's crashing
- Give some fluid (assuming no heart failure)
- Check a blood gas and replace whatever is low
- Give some empirical magnesium
Very rarely has this not worked, so I'm sticking to it, but for the exam you need to be able to explain your actions, hence we've written this post.
I spent far too long on this https://t.co/Fqs4v6US9t pic.twitter.com/jVGFa87gvM
— Edd B (@edd_broad) November 20, 2020
The algorithm
Start as you always do - ABC and fix as you go.
If the heart rate is fast because of anaphylaxis, life-threatening asthma or tension pneumothorax, hopefully this will become apparent before you start reaching for adenosine or syringes to blow in.
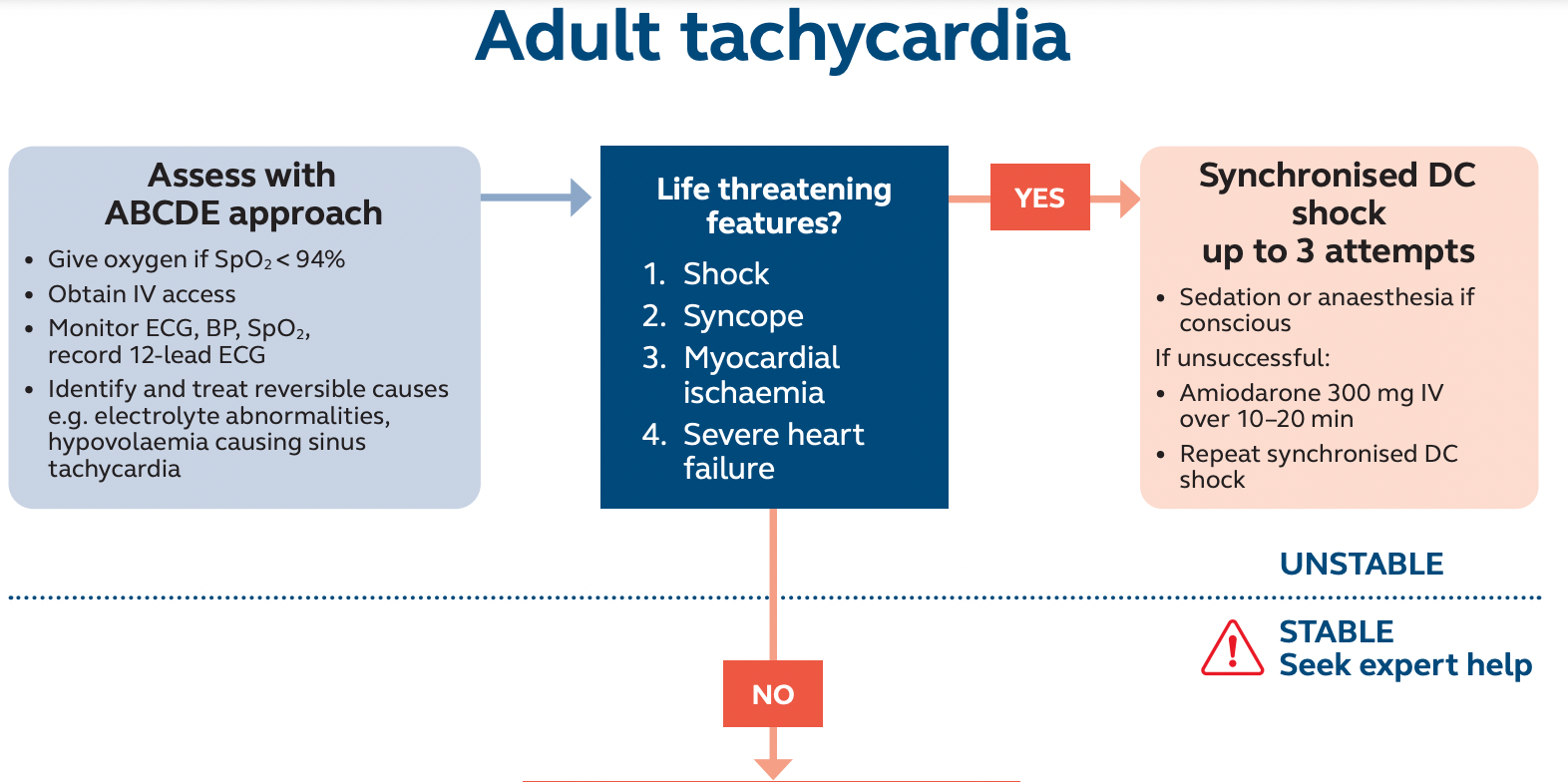
Please can you come and sedate this patient...
This is a classic call, often from CCU or Resus
- Patient in SVT or other tachyarrhythmia
- Signs of shock or ischaemia
- Needs electrical medicine
It's much nicer to undergo DC cardioversion with some sedation on board, but this is possibly the hardest sedation to get right.
Sedating a patient with life-threatening cardiovascular compromise that already has an arrhythmia is real tiger country, so you need your wits about you.
If you feel like you're giving a ridiculously small dose of midazolam/ketamine/propofol then you're doing it right - these patients need very little indeed.
Remember they're not having a joint manipulated or anything incised - they just need to not be fully aware.
The most important thing is that they don't really remember their millisecond jolt of chest-lightning.
- 0.5 mg midazolam is often more than enough
- Make sure you have all your airway kit ready
- Be ready to manage as a VF arrest
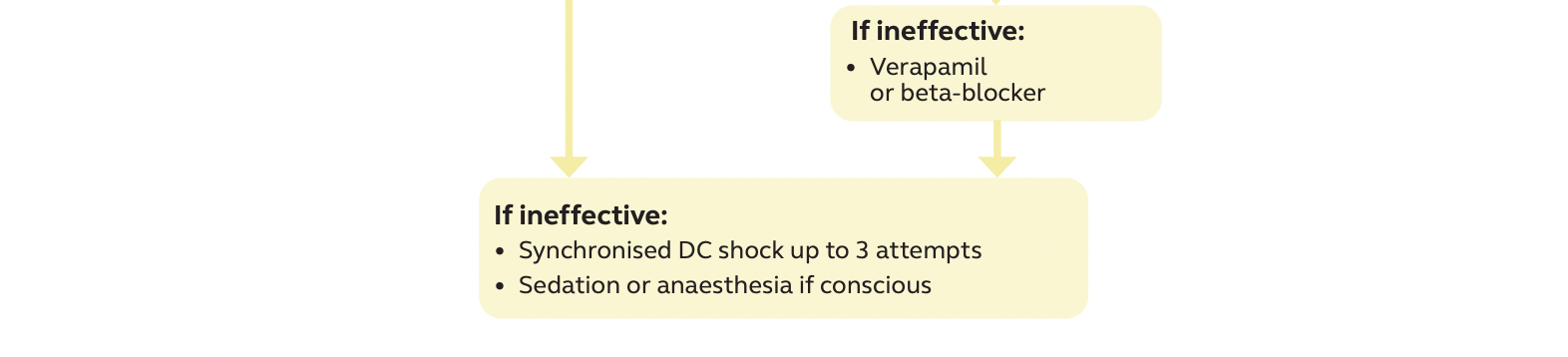
Managing a stable tachycardia
We tend to do less of this as anaesthetists, largely because by definition there generally isn't any requirement for ABC support.
This might crop up as an intra-operative scenario with a tachycardia in an anaesthetised patient.
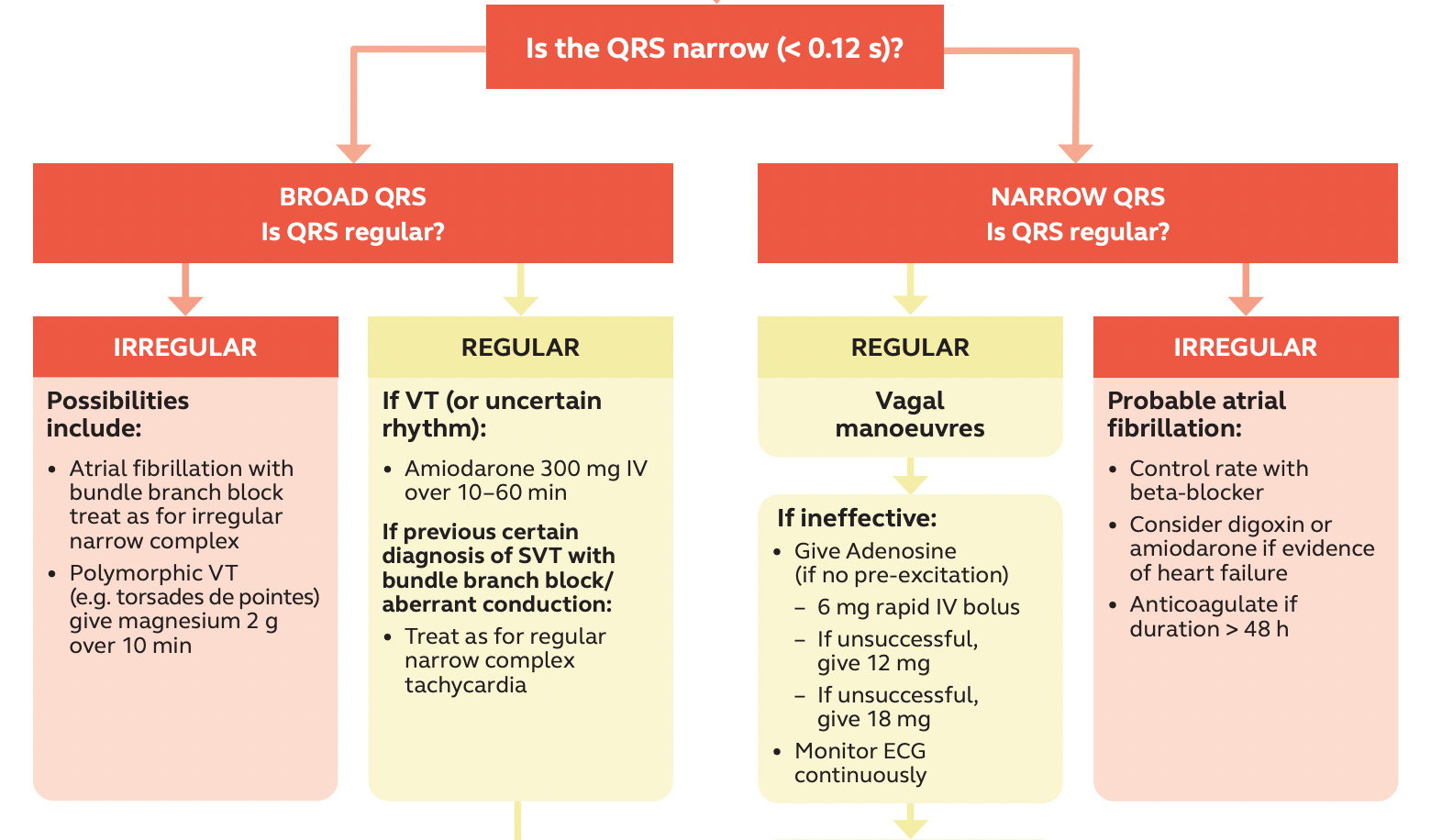
Vagal manoeuvres
- I have seen ice work, but it usually doesn't
- I have seen blowing into a syringe work, but it usually doesn't
- Adenosine rarely fails if the problem is a legitimate AV node issue
If you're using adenosine, be ready to use a laryngoscope and a defibrillator.
And if that doesn't work
By this point you're either not involved as an anaesthetist or you're being called to come and sedate a patient for a DC cardioversion as described previously.
Again - easy on the sleepy meds.
What is SVT?
Any fast heart rhythm that is dependent on nodal tissue to keep it going.
So things like AF and multi-focal atrial tachycardia aren't technically SVT as the AV node isn't the causative issue.
Other atrial tachyarrhythmias
The Regulars
Sinus tachycardia
- This is a normal autonomic response to some stressor on the cardiovascular system
It is fixed by fixing the cause:
- Hypovolaemia
- Sepsis
- Pain
- Anxiety
The usuals.
Atrial flutter
- Pathological narrow complex organised rhythm
- Usually from a re-entrant circuit around the tricuspid valve
- The atria depolarise at around 300 bpm
- Variable AV node conduction - usually around 2:1 - gives a heart rate at around 150 bpm
- Often hard to spot because of the speed and overlap between T and P waves
- The conduction ratio can also change between 2:1, 3:1 etc, making it look irregular
AV re-entrant tachycardia
- Has an accessory pathway that congenitally abnormal
- Bypasses the AV node and can conduct forwards or backwards
There are three types of AVRT:
- Orthodromic - regular narrow complex tachycardia anterograde via the AV node and back up the accessory pathway
- Antidromic - regular broad complex tachycardia anterograde via the accessory pathway and back up the AV node
- AF with rapid anterograde conduction via accessory pathway
See below for WPW.
AV nodal re-entrant tachycardia
- No accessory pathway
- The re-entrant circuit is via the posterior and anterior pathways to the AV note, where one is conducting significantly faster than the other
- An atrial ectopic starts during the refractory period of the fast pathway
- This then tracks down the slower pathway, then back up the fast pathway once it's ready to go again
- As a result the P wave is buried in the QRS complex
- Usually in young adults
- Rarely causes major haemodynamic compromise unless there's other cardiac badness underneath
Wolff-Parkinson-White
- WPW is a particular type of AVRT
- Can be orthodromic or antidromic
- There has to be 'pre-excitation' on the ECG as well as them having symptomatic tachyarrhythmias
- Aberrant conduction between atria and ventricles via Bundle of Kent
Major ECG features:
- Short PR (because the accessory node bypasses the AV node)
- Broad QRS with delta wave due to fusion of early depolarisation down accessory pathway, and late depolarisation through the AV node
The reason WPW is so dangerous is because the patient loses the natural rate-limiter of the AV node.
The accessory pathway can conduct ridiculously rapidly to the ventricles, so if the atria go too fast, the ventricles will do the same, and end up in VF.
Avoid verapamil.
Focal atrial tachycardia
- Regular atrial tachycardia
- Starts somewhere in the atria but not in the SA node
- P wave looks slightly different
- Usually quicker onset than sinus tachycardia
The Irregulars
Atrial fibrillation
- Multiple little electrial triggers throughout the atria
- Irregular conduction to ventricles
- No P waves
- Irregular R-R interval
- Narrow complexes (assuming no bundle branch block as well)
Multifocal atrial tachycardia (MAT)
- Usually only in really unwell elderly patients
- Sometimes seen in theophylline toxicity
- Usually progresses to AF
- Characterised by irregular atrial impulses with at least three different-looking P waves
This is usually best managed by treating the cause rather than the arrhythmia itself.
Look at the P waves
- I can't see them, irregular - AF
- I can't see them, regular, really fast - try adenosine
- The P waves are all weird - MAT
- Sawtooth P waves 250-300 per minute - Flutter
- Normal P waves - AVRT or AVNRT
- Weird P waves with long PR - FAT
- Definitely no P waves, regular - junctional tachycardia
Tell me about adenosine
Do not tell the patient they're about to feel an impending sense of doom.
Tell them they're going to feel strange, like they're skipping a beat, for a few seconds.
Adenosine induces a hopefully transient AV node block, for a few seconds.
- Adenosine hits the A1 receptor
- Inhibits adenylyl cyclase
- Reduces cAMP
- Allows potassium out of the cell
- Hyperpolarises the cell
Needs to be injected through a large, proximal cannula and flushed very quickly, as it gets metabolised rapidly in the blood.
Contraindications
- Known accessory pathway (WPW) - can induce AF, VT, VF
- Asthma or severe COPD - can induce bronchospasm
- Broad complex tachycardia
- Sick sinus syndrome
Other drugs
By this point you're usually involving some sort of cardiological person, but you need to be able to list the second and third line options for SVT
- Verapamil
- Beta blockers
- Flecainide
- Procainamide
Perioperative AF
Some patients either have AF anyway, and just flick in and out throughout their perioperative stay, and others develop new AF for the first time.
- Follow the algorithm above
- Focus on treating the underlying trigger
- Rate control is the priority, as this increases duration of diastole and therefore oxygen delivery to the myocardium
- Esmolol is fast-acting and easy to titrate, but is a negative inotrope
- Amiodarone is always there, waiting for you
- If a patient is on a beta blocker, verapamil or diltiazem then generally speaking these should be continued perioperatively
Remember to consider the thromboembolic risk of post-operative AF, which needs a CHADS2 score and a decision regarding anticoagulation.
What if it's broad?
It is safer to treat a broad complex tachycardia as VT and be wrong than it is to treat it as SVT with bundle branch block and be wrong.
Useful Tweets
If you’re looking for an AMAZING supraventricular tachycardia (SVT) primer, look no further ⬇️#MedTwitterpic.twitter.com/52RWVcE3uY
— Avraham Z. Cooper, MD 🩺 (@AvrahamCooperMD) September 25, 2022
This video shows a modified Valsalva maneuver being used in the emergency treatment of stable SVT (supraventricular tachycardia)! This awesome ER team was able to temporarily convert a stable paroxysmal SVT back into sinus rhythm!
— Paul Wischmeyer MD (@Paul_Wischmeyer) October 1, 2024
This is a beautiful example of how manipulating… pic.twitter.com/gE6IF1P8U7
References and Further Reading
Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.