Subarachnoid Haemorrhage
Take home messages
- 5% of strokes are due to SAH
- 85% of SAH are due to an aneurysm
- Nimodipine is good
What happens?
If there's one clinical presentation that literally every medical student remembers without even trying, it's subarachnoid haemorrhage.
"Er...thunderclap headache...?"
Signs and symptoms
- Sudden onset severe headache
- Nausea
- Vomiting
- Neck stiffness
- Photophobia
- Low GCS
- May also have focal neurology
- Can also cause cardiac arrest
Ah yes, but what else could it be?
- Meningitis
- Migraine
- Pituitary apoplexy
- Postcoital cephalgia*
*You can also have postcoital subarachnoid haemorrhage.
A classic ED presentation
"54 year old female, known smoker and moderate alcohol intake. Reported a sudden onset severe headache to her partner around seven o'clock this morning. Ten minutes later she started acting strangely and became confused before collapsing, at which point her partner called us..."
Ideally blood is meant to stay within the vasculature where it belongs, but if said vasculature becomes compromised for any reason, then it can leak out and explore its surroundings a little.
This isn't always terrible - if the hole is small and the pressure inside the vessel is low (because it's a vein) - then you get a bit of a bruise and that's that.
What is terrible however is when the bleeding is:
- High pressure
- Out of a big hole
- Into a delicate structure that is highly irritated by blood and thus very painful (meninges/peritoneum)
- Into a confined space with a solid organ that's desperately sensitive to changes in pressure but can't escape (the head)
So a ruptured aneurysm into the subarachnoid space is rarely a good thing.
Describe the pathophysiology of subarachnoid haemorrhage
- Aneurysm ruptures
- High pressure blood leaks out into intracranial space
- Meninges are irritated and ICP rises (causing horrendous headache)
- Pressure on the brain has mass effect and impairs blood flow
- This produces neurological symptoms
- Clots develop in ventricles, impairing CSF drainage
- This produces hydrocephalus
- Blood in the subarachnoid space is irritant and contributes to vasospasm and cerebral ischaemia
Confirm the diagnosis
The first line imaging after your convincing history is a non-contrast CT head.
It is also helpful for ruling out oedema, hydrocephalus and big space occupying lesions.
If you see blood on the plain CT head, you then think about a CT angio to locate the source of the bleed, which is usually an aneurysm.
The gold standard answer is digital subtraction angiography.
Why not just do a CT angio first, and save the patient from having two scans?
Because for each person presenting with a headache who would have had a negative plain CT head, a very small number will have a non-ruptured aneurysm show up on CT angio, just as an incidental finding.
They would not know about this aneurysm without the angio, and it may never have caused them any problem.
A small number of these will be deemed to require surgery, and a not-so-small number of these will develop significant neurological complications as a result of said surgery.
Of those that don't undergo surgery, they will have anxiety for the rest of their life whenever they get a headache, they'll struggle to get a mortgage, house insurance, travel insurance, health insurance...
You get the idea.
If the CT is negative, but you're convinced it's likely to be SAH, then a lumbar puncture should be done at 12 hours post symptom onset.
You're testing for
- RBC
- Bilirubin
- Xanthochromia
Causes of subarachnoid haemorrhage
Remember to classify, and here we can say traumatic and non-traumatic.
Within non-traumatic, we than have congenital* and acquired.
The most common three causes are:
- Aneurysm (85%)
- Arterio-venous malformation
- Trauma
*weird stuff like Moyamoya disease.
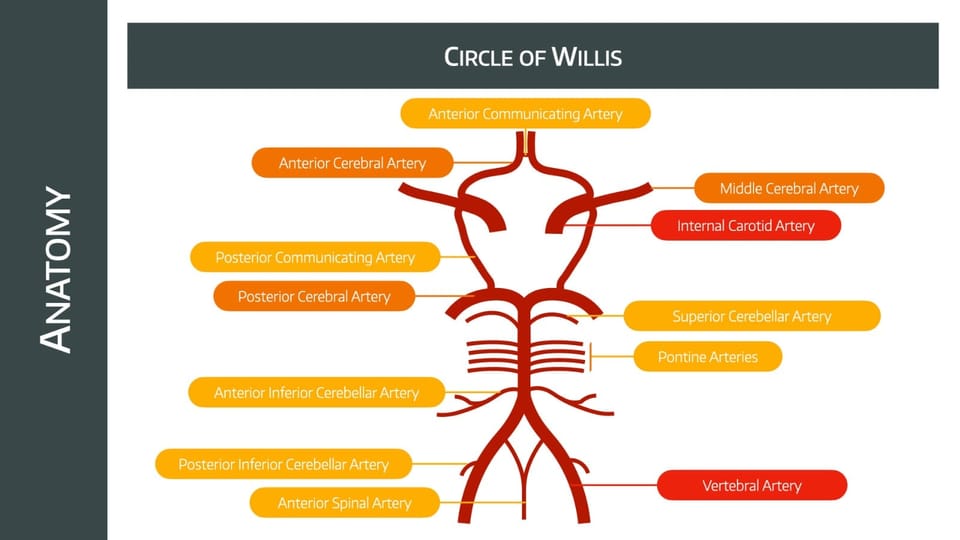
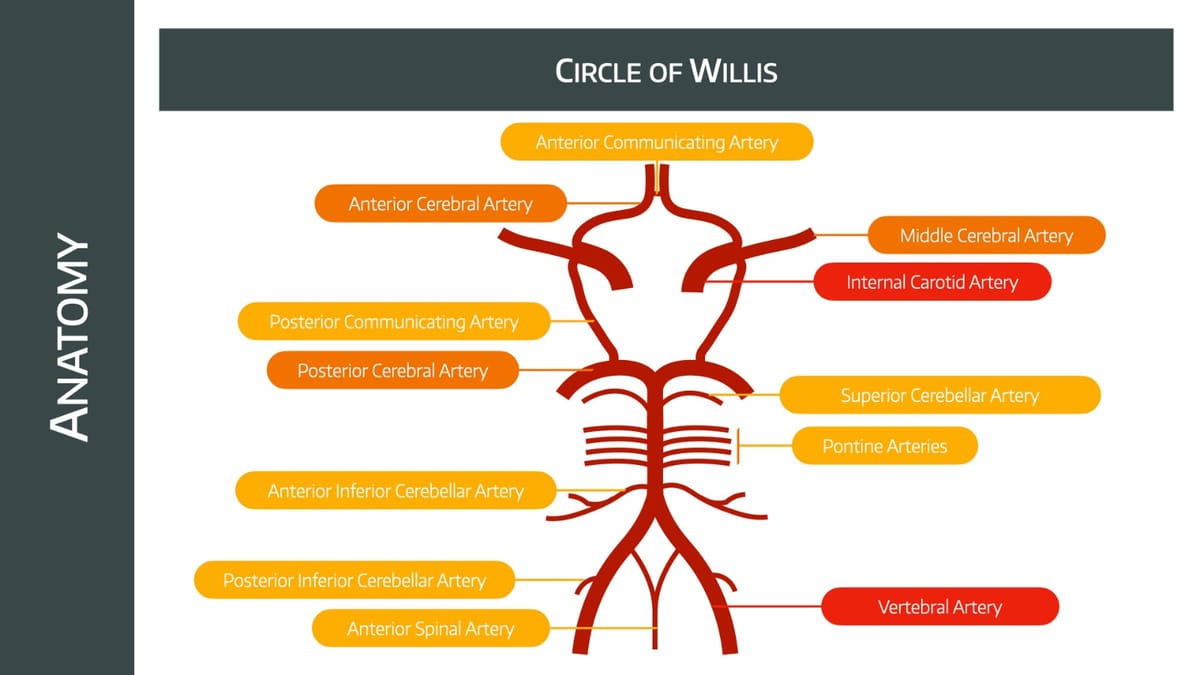
Which are the most common sites of aneurysm rupture?
- Posterior communicating artery*
- Anterior cerebral artery
*Specifically where it splits with the internal carotid
So how bad is it?
- Incidence up to 12/100 000 in the UK per year
- 50% mortality, 25% never reach hospital
- 30% of survivors will have substantial care requirements
Who gets it?
- The highest incidence is in 40-60 year olds
- 3:2 Female to male ratio
- Smokers and drinkers
- Family history of aneurysms
- Polycystic kidney disease
Lots of people have decided to make up scoring systems for subarachnoid haemorrhage - to allow us to determine how bad the one in front of us is - but the two we generally use are the Hunt and Hess and the World Federation of Neurosurgeons Scale.
These are both clinical scales. The Fischer scale is another but it uses CT information as well.
Hunt and Hess Scale
- Grade 1 - asymptomatic or mild headache and slight neck stiffness
- Grade 2 - Moderate to severe headache or neck stiffness, possible cranial nerve palsy
- Grade 3 - Drowsy, confused, mild focal deficit
- Grade 4 - Moderate to severe hemiparesis, stupor
- Grade 5 - Comatose, decerebrate posturing, moribund
World Federation of Neurosurgeons Scale
- Grade 1 - GCS 15 with no motor deficit
- Grade 2 - GCS 14-13 with no motor deficit
- Grade 3 - GCS 14-13 with motor deficit
- Grade 4 - GCS 12-7
- Grade 5 - GCS 6-3
Fischer Scale
Requires a CT head first.
- No blood
- Diffuse deposition, or thin layer, no clots >3mm or layers >1mm
- Dense collection of blood >1mm thick
- Intracerebral or intraventricular clots
What are the three main predictors of morbidity and mortality in subarachnoid haemorrhage?
- Low GCS on admission
- Age
- Volume of blood on CT scan
So what do I do?
There are four main priorities in the management of a subarachnoid haemorrhage:
- Resuscitation and haemodynamic stabilisation
- Fixing the ruptured aneurysm
- Reducing secondary brain injury
- Avoiding the avoidable complications
You as the anaesthetist are likely going to be heavily involved in the first two, and possibly involved in the latter two if you're also working on ICU.
Resuscitation
Airway (as always) for low GCS airway protection and ventilatory control, aiming for:
- PaO2 of >13 kPa
- Normocapnia (4.5–5.0 kPa)
Cardiovascular management is about maintaining stable perfusion of the brain and avoiding triggering another bleed.
- Aim for a systolic 100 - 160 mmHg
- MAP 90 - 110 mmHg
- Avoid lots of laryngeal traction please and thank you
Neuro stuff:
- Monitor pupils before and after tubing, both size and speed of reaction
- Avoid fever
- Keep glucose level steady between 4.5 and 11 mmol/litre
- Sedation and pain relief
- Give nimodipine 60mg every six hours for 21 days (reduces vasospasm and improves overall outcomes)
Then for most anaesthetists it's time to prescribe a stat dose of diesel - or kerosene if you're lucky - and get to a neurosurgical centre.
What are the non-neurological complications after subarachnoid haemorrhage?
- Hyperglycaemia
- Fever
- Myocardial infarction
- Heart failure
- Aspiration
- Pulmonary oedema (neurogenic or cardiogenic)
- Hospital acquired pneumonia
- ARDS
- Hyponatraemia (SIADH, cerebral salt wasting or IV fluids)
Clip or coil?
The question as to whether or not you put someone through a procedure to try and fix the aneurysm is determined by:
- Age
- WFNS scale
- Comorbidities
- How long the bleed has been there
- What the aneurysm looks like
Now you can open the skull and clip the aneurysm, or you can tunnel your way radiologically through the vasculature and deploy embolising stents to block the artery off.
- Both work
- Coiling isn't always possible
- Coiling seems to give a slightly lower incidence of bad outcomes (in certain circumstances)
- This is hotly debated between different centres
It'll largely be determined by the hospital you're working at deciding which technique is 'what we do round 'ere'.
How to anaesthetise the patient
Unlike sphenopalatine ganglioneuralgia, anaesthetising for aneurysm rupture is easier said than done, as you've got a potentially highly unstable patient with a time-critical condition needing deep, delicate anaesthesia.
The main priorities when anaesthetisting for aneurysm surgery
- Make sure the patient isn't awake and doesn't move
- Maintain cardiovascular and respiratory stability
- Maintain cerebral perfusion pressure
- Maintain a stable ICP
- Prevent brain swelling
- Avoid cerebral vasospasm
- Get the surgeon to fix it carefully and quickly
Two ways to anaesthetise for SAH surgery
- Avoid too much induction agent to avoid hypotension, and then give lots of stuff to prevent excessive response to laryngoscopy (opioids, esmolol, lidocaine)
- Get them seriously deep with lots of induction agent, and use a vasopressor infusion from the start to avoid hypotension
What anaesthetic should I use?
The one you're told to use.
It doesn't matter as long as your technique keeps the patient asleep and stationary, and also maintains cerebral perfusion pressure.
- Sevoflurane has minimal effect on cerebral blood flow or ICP, but massively drops cerebral oxygen demand
- Isoflurane and desflurane increase blood flow and ICP, but drop oxygen demand
- Propofol and thiopentone hugely drop all three
- Nitrous increases ICP, oxygen demand and blood flow
- Opioids do very little to any of them
The reality is you're going to walk into the neuro theatre and the consultant is going to tell you what to use.
So use that.
What monitoring do I need?
You need your standard AAGBI (AoA) set up of:
- Pulse oximeter
- Blood pressure
- ECG
- ETCO2
Plus:
- Invasive blood pressure monitoring
- Urine output
- Neuromuscular block monitoring
- Temperature
- Central venous pressure
And maybe even:
- Evoked potentials
- Precardial Doppler
- Transoesophageal Echo
- Pulmonary artery catheter
- ICP monitoring
- Jugular venous bulb monitoring*
*You put a catheter the wrong way into the jugular so it sits in the jugular bulb, and monitor the oxygen saturations.
It gives a global measure of oxygen delivery to the brain.
Other interesting bits
- Hypothermia doesn't appear to help
- Bypass and circulatory arrest with cooling to <22°C might be needed in the case of clipping a giant aneurysm (more than 2cm diameter)
- Don't routinely hyperventilate, and avoid excessive PEEP to reduce CVP
This is seriously cool
If the surgical field is full of blood, and the surgeon can't get a good view to fix the aneurysm, the logical thing to do is definitely to completely stop cardiac output while they clip it... right?
This is a case performed by Dr Hunt Batjer which launched our interest In adenosine for aneurysm clipping. Special credit goes to Neuroanesthesiology pioneer Dr Tony Koht. Film credits go to medical student @evturcotte. pic.twitter.com/GCIQgAEPjU
— Bernard Bendok, MD (@BernardBendokMD) August 29, 2022
CPP and TMPG
These are your two most important numbers during aneurysm surgery or coiling.
- CPP = Cerebral perfusion pressure
- TMPG = Transmural pressure gradient
The first one tells you how much blood you're delivering to the brain tissue, and the second tells you how likely you are to blow the aneurysm even wider open.
- CPP = MAP - ICP
- TMPG = MAP - ICP
Oh look they're exactly the same.
But you want a high CPP and a low TMPG...
So if the ICP increases because of swelling or bleeding, you don't want to bring it back down again too quickly, because you'll rapidly increase the TMPG and potentially worsen the bleeding.
But if you don't bring it down enough, and they open the dura with a high intracranial pressure, that's bad too.
Yup, neuroanaesthesia is hard.
Long story short, try and keep blood pressure near the preoperative level until the aneurysm is fixed, and don't change anything too quickly.
Preventing cerebral vasospasm
If they're going to spasm, it'll usually be before 12 days after the initial rupture, so you need to monitor for longer if you're operating on day 2 post rupture than if you're operating after 11 days.
IV fluids
- If they didn't have signs of cerebral vasospasm before surgery, then maintain normovolaemia
- Consider bringing the MAP up a little after clipping
- If they had symptomatic spasm beforehand then they need careful volume loading and maintenance of moderate hypertension after clipping
Either way, avoid hypotension intraoperatively.
Papaverine
- You can stick papaverine intracisternally after clipping, but before closing the dura
- The idea is to reduce or prevent cerebral vasospasm
- Side effects include facial nerve palsy, mydriasis, hypotension and hyperthermia
What is DCI?
Delayed cerebral ischaemia, and it's important to know about as it occurs in over 60% of cases.
- The highest risk time is 4-10 days after the initial bleed
- It worsens overall outcome
- DCI often occurs with vasospasm, but can occur alone
The definition of DCI
- Neurological deterioration related to ischaemia that persists for over an hour with no other cause identified, such as seizure or hydrocephalus
*Vasospasm on the other hand is angiographically-proven arterial constriction that causes clinically relevant signs and symptoms.
Unsurprisingly DCI is more common in those with a worse bleed, and smokers who are already prone to vasospasm.
How to manage delayed cerebral ischaemia
DCI is reversible, and you need to hit it early with
- Nimodipine
- Triple H therapy
- Magnesium
- Statins
Tell me about nimodipine
- Dihydropyridine calcium channel blocker
- Blocks L-type calcium channels
- Not exactly clear what it does in SAH but it seems to reduce incidence of delayed cerebral ischaemia (presumably prevents vasospasm)
- It's a cheap way to improve outcomes in SAH
- Give 60mg 4 hourly PO/NG ideally or IV if needed
- Give 30mg 2 hourly if worries about dropping blood pressure too much
- Give for 21 days
Tell me about triple H therapy
- Hypertension
- Hypervolaemia
- Haemodilution
The aim is to improve cerebral perfusion pressure and oxygen delivery. There's no super-solid evidence that Triple H therapy actually does all that much, but avoiding hypotension definitely is important.
Hypervolaemia also carries cardiac and pulmonary risk, so we aim for euvolaemia.
Oh and haemodilution impairs oxygen supply and anaemia is associated with poorer outcomes, so a haemoglobin of 80-100 g/l is recommended.
So basically ignore the idea of triple H and just keep cerebral perfusion pressure above 70mmHg.
Tell me about magnesium
- It's awesome and all anaesthetists love it
- It's neuroprotective
- It's vasodilatatory
- Avoid hypomagnesaemia
- Don't target hypermagnesaemia
Tell me about statins
- Reduce glutamate-mediated excitotoxicity
- Reduce ROS production
- Increase e-NOS production
- Reduce inflammation
If a patient is on a statin before they bleed into their head, continue the statin.
If they weren't, then only start a new statin if you think they're at very high risk of DCI and vasospasm.
What other treatment options for DCI are there?
- Endovascular treatment
- Antiplatelets (only if a stent was used)
Useful Tweets and Resources
Here's the Neurocritical care society 2011 guideline if you're interested
🔐The possibility of an intracranial haemorrhage after spinal anaesthesia should always be considered when spinal subarachnoid haemorrhage is identified, even in uncomplicated procedures in patients without coagulopathy.
— 𝘈𝘯𝘢𝘦𝘴𝘵𝘩𝘦𝘴𝘪𝘢 𝘙𝘦𝘱𝘰𝘳𝘵𝘴 (@Anaes_Reports) June 16, 2020
🔗https://t.co/fSVJY6sXqW pic.twitter.com/ok60KNX25y
References and Further Reading
Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
