Serotonin Syndrome
Take home messages
- Serotonin does lots of different things, in the CNS, gut and platelets
- If you have too much of it, you get a triad of autonomic hyperactivity, neuromuscular abnormalities and mental status change
- It's a clinical diagnosis, and there has to be a trigger
- Treatment is mainly supportive and it usually resolves in 24 hours
Serotonin
- Monoamine neurotransmitter made from L-tryptophan
- Plays a role in bronchospasm, platelet aggregation, pain, nausea and vomiting
- Metabolised by monoamine oxidase (MAO)
- Primary metabolite is 5-hydroxyindole acetic acid (5-HIAA), excreted in urine
In what three locations is serotonin made?
- Serotoninergic neurons in the CNS
- Enterochromaffin cells in the GI tract
- Platelets
Serotonin receptors
- 7 classes 5HT1–7 with different subtypes e.g. 5-HT2a
- All act via G-Proteins and cAMP, apart from 5HT-3, which acts via a ligand-gated ion channel
- 5HT-3 receptors act in GI tract and CNS to generate emetic response, hence inhibitors of 5HT-3 receptors (like ondansetron) are effective antiemetics
Serotonin Specific Reuptake Inhibitors
- Commonly used medications to boost synaptic serotonin levels
- Best not to stop in perioperative period, but a few missed doses not significant
- Anaesthesia can trigger hypotension, arrhythmias, shivering, and postoperative confusion, albeit rarely
- Probably decrease platelet aggregation but not thought to be clinically significant in perioperative setting
Serotonin syndrome
- Mixture of mental status change, neuromuscular abnormalities, and autonomic hyperactivity
- Occurs within 24 - 48 hours of trigger, usually a change in medications
- Thought to be from hyperstimulation of 5-HT1a and 5-HT2 receptors in medulla and central grey nuclei
- Classic triggers are a combination of drugs that boost serotonin levels, including SSRIs, tricyclic antidepressants, MAO inhibitors, and St. John's Wort
- Previously diagnosed according to the Sternbach criteria, either four major or three major plus two minor features must be present
Sternbach Criteria - Major symptoms
- Confusion
- Elevated mood
- Coma
- Fever
- Sweating
- Clonus
- Hyperreflexia
- Tremor
- Rigidity
- Shivering
Sternbach Criteria - Minor symptoms
- Hyperactivity
- Agitation
- Restlessness
- Insomnia
- Tachycardia
- Tachypnoea
- Labile blood pressure
- Flushing
- Incoordination
- Mydriasis
- Akathisia
- Ataxia
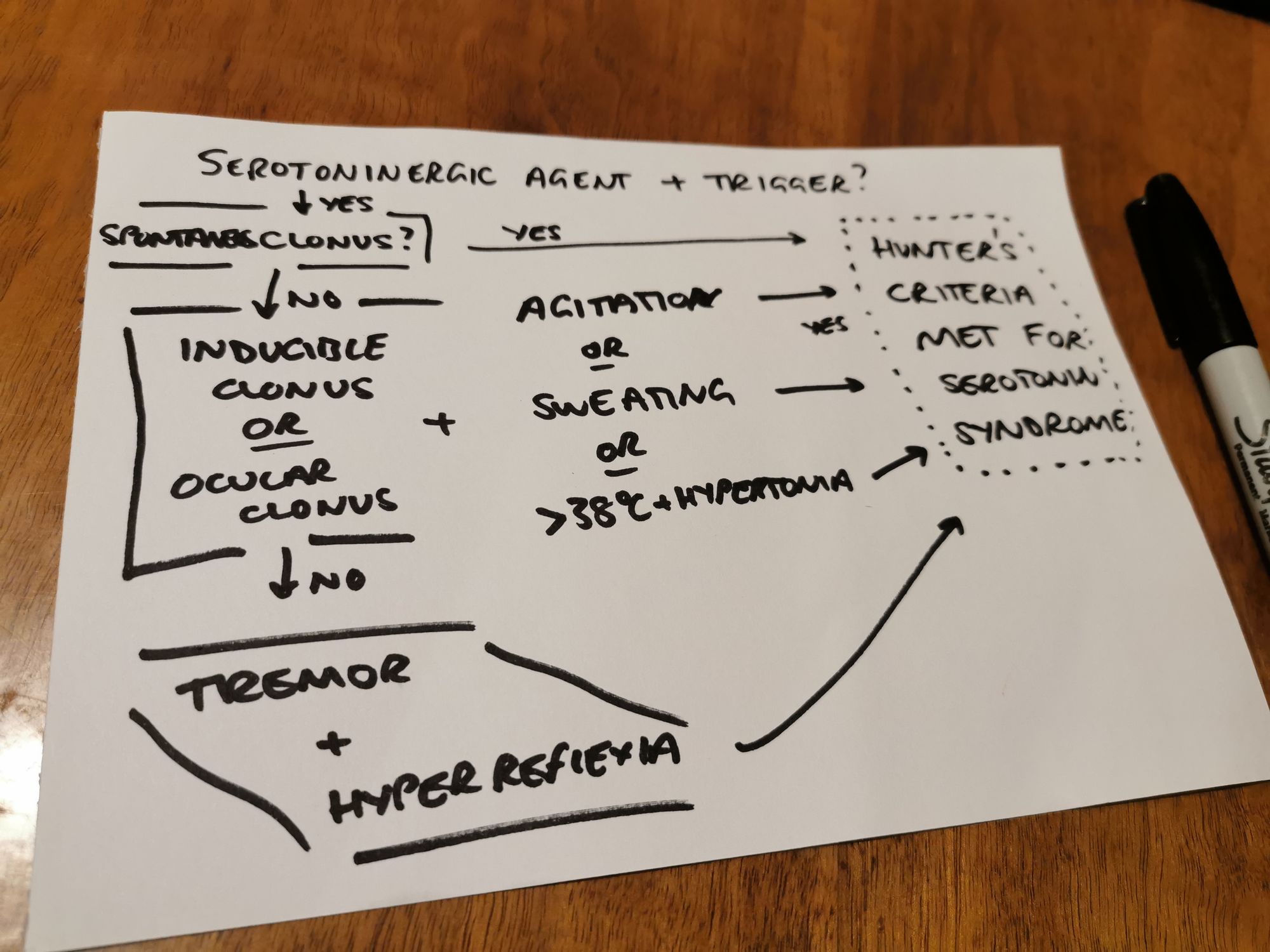
- But Hunter criteria probably better, and so are used more frequently nowadays:
Treatment
- Stop any drugs that increase serotonin
- Supportive therapy
- Self-resolves within 24 hours - rarely fatal - usually good prognosis if spotted early
- Benzodiazepines for anxiolysis and seizures
- Noradrenaline if severely hypotensive
- Cyproheptadine has also been used (antihistamine that also has anti-serotonin activity)
1/2
— Pharmacopalliation (@pharmacopallia) December 27, 2022
Serotonin Syndrome, the classical triad of clinical features pic.twitter.com/SasGT6WyIr
References and Further Reading:
- Sadasivan Chinniah, FRCA, James L.H. French, FRCA, David M. Levy, FRCA, Serotonin and anaesthesia, Continuing Education in Anaesthesia Critical Care & Pain, Volume 8, Issue 2, April 2008, Pages 43–45, https://doi.org/10.1093/bjaceaccp/mkn006
- Bartakke A, Corredor C, van Rensburg A. Serotonin syndrome in the perioperative period. BJA Educ. 2020 Jan;20(1):10-17. doi: 10.1016/j.bjae.2019.10.003. Epub 2019 Dec 4. Erratum in: BJA Educ. 2020 Apr;20(4):139. PMID: 33456910; PMCID: PMC7807833.