Renal Autoregulation and GFR

Take home messages
- Renal metabolic demand is determined by blood flow
- Autoregulation occurs via the myogenic reponse and tubuloglomerular feedback, plus some other bits and bobs we don't really understand
- The units on the graph don't matter, as long as there's a plateau from around 75mmHg to 160mmHg ish
Podcast episode
The blood supply to the kidney
The kidneys receive a quarter of the cardiac output, which is approximately:
- 1.25 litres per minute or
- 400 - 500ml/100g/minute
Over 90% of this supply is to the cortex, with only around 5% reaching the medulla, hence the medulla's profound sensitivity to hypoperfusion in shock states (why all really sick people get an AKI).
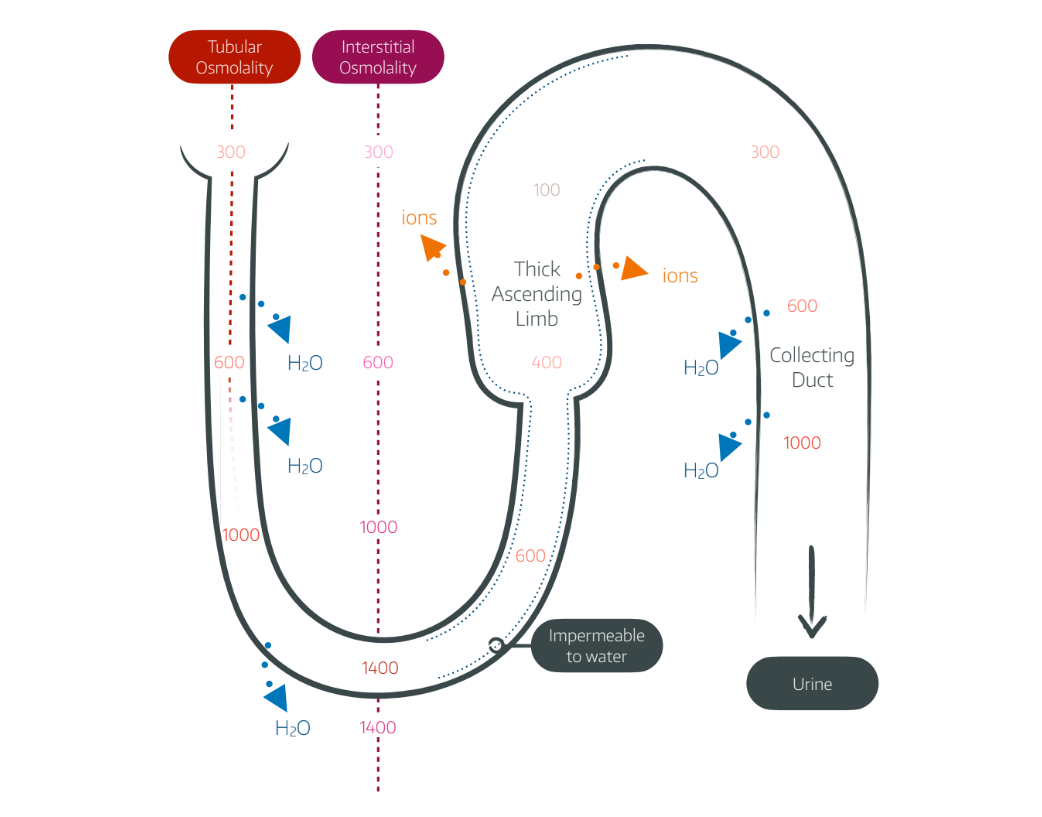
Why such low flow to the medulla?
- To maintain a steady urea concentration gradient, which drives all of the water-reabsorbing machinery in the Loop of Henle and Collecting duct
- If the blood flow were any higher, simple biophysics determines it would wash away all of that hard-earned urea
Weirdly, the hardest working bit of the kidney needs to be in a constant state of near-hypoxia in order for its machinery to actually work.
The kidneys are special
We knew that already, but tell us again why?
Because unlike any other organ, the metabolic demand of the kidney is determined in large part by the blood flow that it receives - not the other way around.
This may sound completely nonsensical, but if you think about it, the kidney's job is mostly maintaining concentration gradients and reabsorbing ions such as sodium, and these ions only need absorbing if they're being supplied and filtered by the glomerulus in the first place.
- Muscle tissue's job is to move as much as it is told to do so, and it just has to hope it receives enough fuel and oxygen to facilitate this
- The kidneys however are like factory workers on a production line, told to clean up whatever comes along the conveyor belt - if there's less blood supplied, there's less work to do
The very high renal blood flow that we see is actually to allow efficient filtration in the glomerulus, rather than being due to the kidneys having a particularly high metabolic demand (the renal oxygen extraction is pretty low at around 10-15% on a good day).
This means that renal oxygen extraction remains amazingly constant over a wide range of renal blood flow values
The blood is supplied via the renal artery which supplies two capillary networks
- A high pressure glomerular network
- A low pressure peritubular network
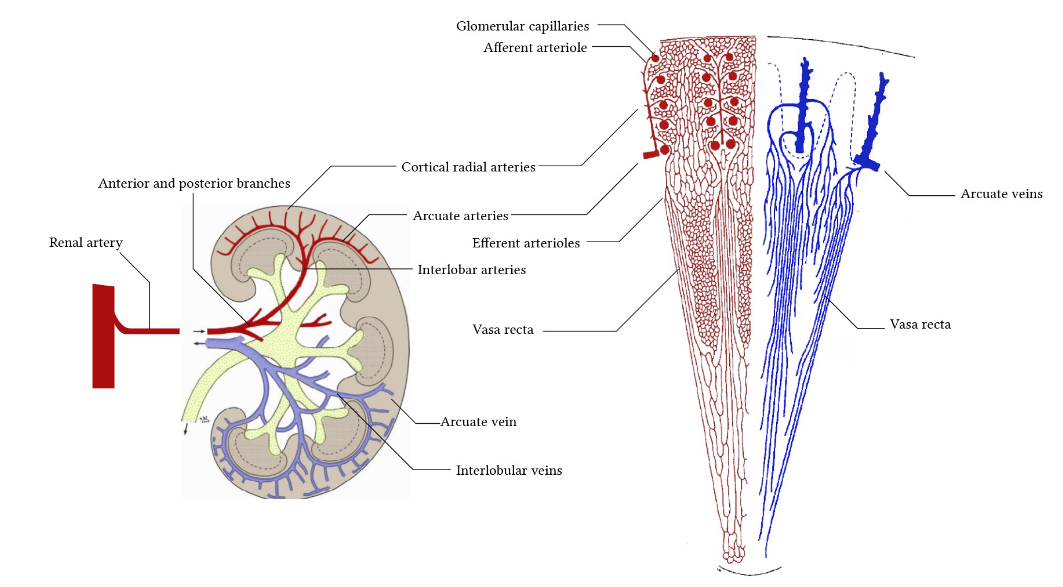
What is the course of blood vessels through the kidneys?
- Aorta
- Renal artery
- Segmental artery
- Interlobar artery
- Arcuate artery
- Cortical radial artery
- Afferent arteriole
- Glomerulus
- Efferent arteriole
- Peritubular capillary
- Vasa recta
- Veins
- Renal vein
- IVC
Around 30 vasa recta branch off from each efferent arteriole
Autoregulation
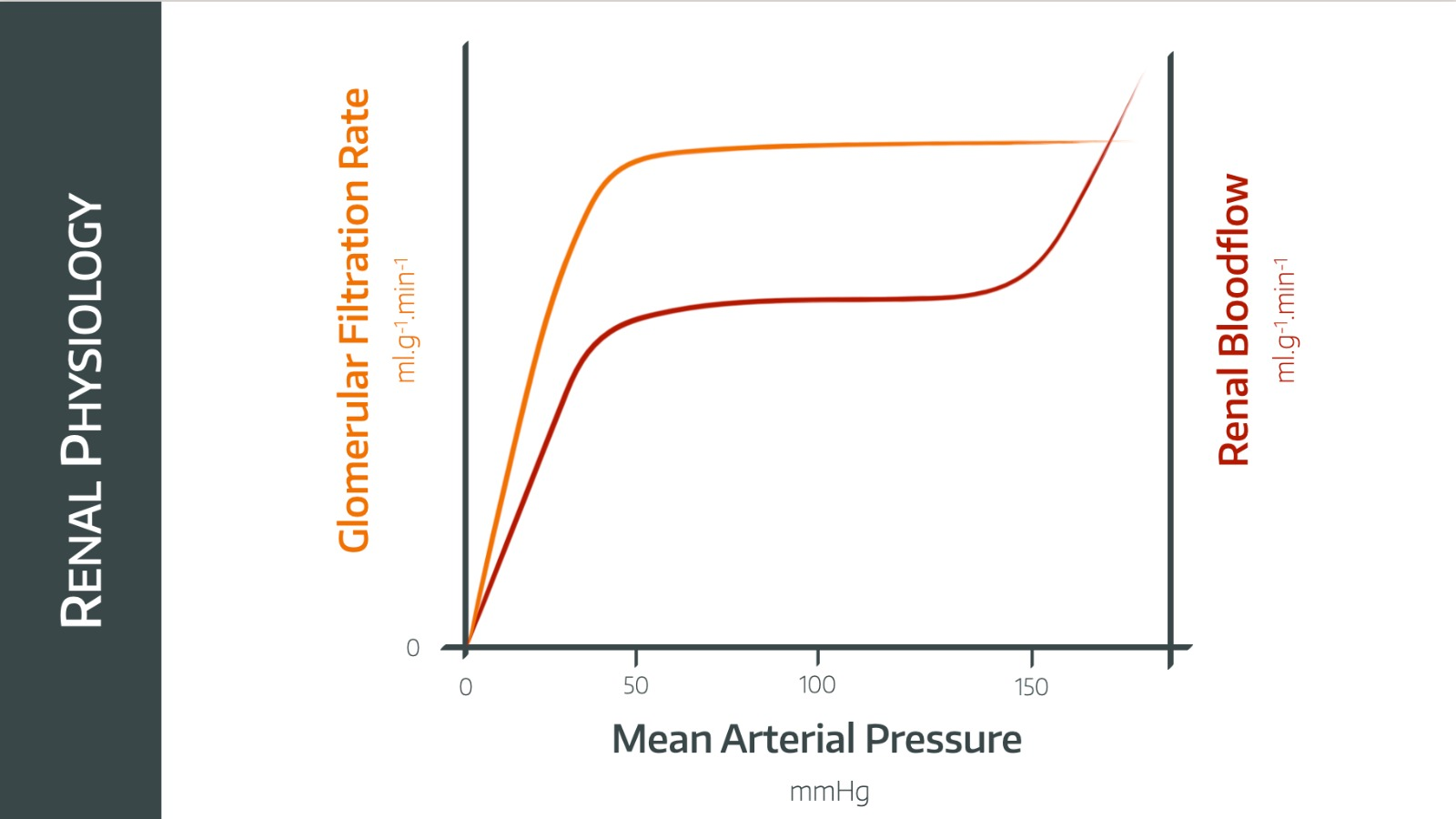
The kidneys are not unique in their ability to regulate their own blood flow, but they have their own special graph that you need to be able to draw in the exam.
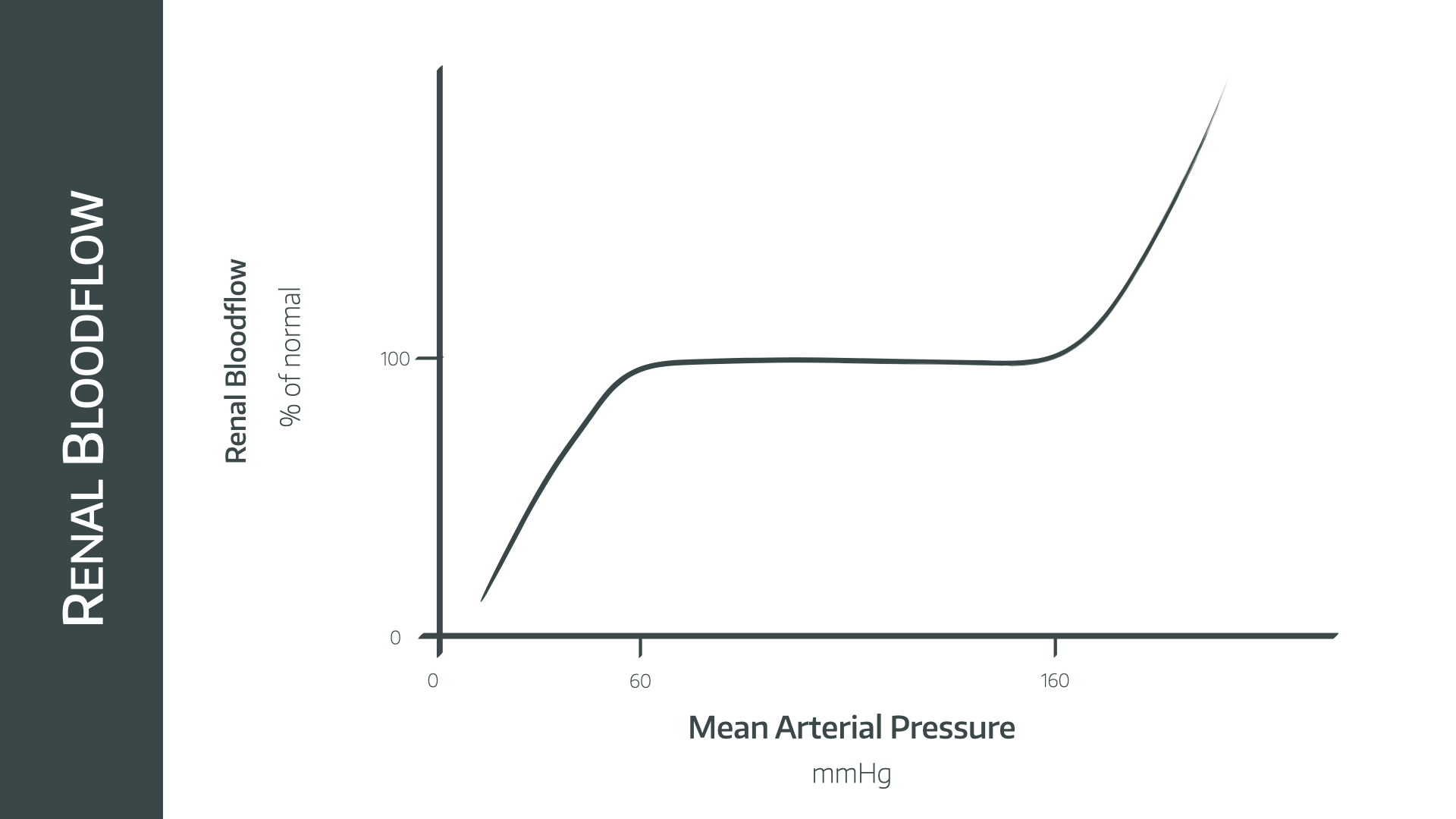
When drawing this graph, the most important part is a relatively flat line between pressures of around 75mmHg and 160mmHg
How does it work?
As with many magical aspects of physiology, we don't fully understand, however we suspect it may involve three mechanisms.
Myogenic response
- The afferent arteriole has stretch receptors embedded within the muscle of the vessel wall
- If it is stretched, magical mechanisms involving things like stretch-sensitive calcium channels make it contract, reducing the diameter of the lumen and increasing the resistance of the vessel
- Ohm's law dictates that flow will therefore be adjusted nicely
This is responsible for around 50% of the autoregulatory power of the kidney and is clearly not unique to renal tissue.
Tuboglomerular feedback
- As blood flow to the kidney increases, more blood is filtered and more sodium passes along the tubule to the macula densa
- Increased sodium detected at the macula densa causes afferent arteriolar constriction
- Probably using adenosine and ATP
- This reduces flow and completes the negative feedback loop
This is unique to the kidney.
Humoral and autonomic influence
- Vasoconstrictors such as angiotensin II and endothelin constrict the efferent arteriole, reducing renal blood flow but maintaining GFR
- Vasodilators such as prostaglandins, bradykinin and other amino acids do the opposite
- Sympathetic tone contributes to arteriole contraction - with slightly more afferent than efferent contraction - meaning sympathetic stimulation reduces renal blood flow slightly
This box exists largely to explain the fact that if you take away tubuloglomerular feedback and myogenic response, you still somehow get some autoregulation of blood flow.
In the exam they're looking for knowledge about the previous two mechanisms, so don't worry too much about this bit.
Tell me about GFR
Glomerular filtration rate is a process of ultrafiltration and occurs at around 125ml/min
This works out at around 180 litres per day, and the main determining factor is particle size
- Molecules over 70 000 daltons are not filtered
- Molecules below 7000 daltons are freely filtered
- Negatively charged molecules are repelled by the basement membrane and therefore have a reduced filtration fraction
Glomerular filtration and tubular reabsorption of fluid and solutes can be altered by the kidneys to maintain homeostasis and remove waste products and drugs.
The principle is the same as of Starling’s forces
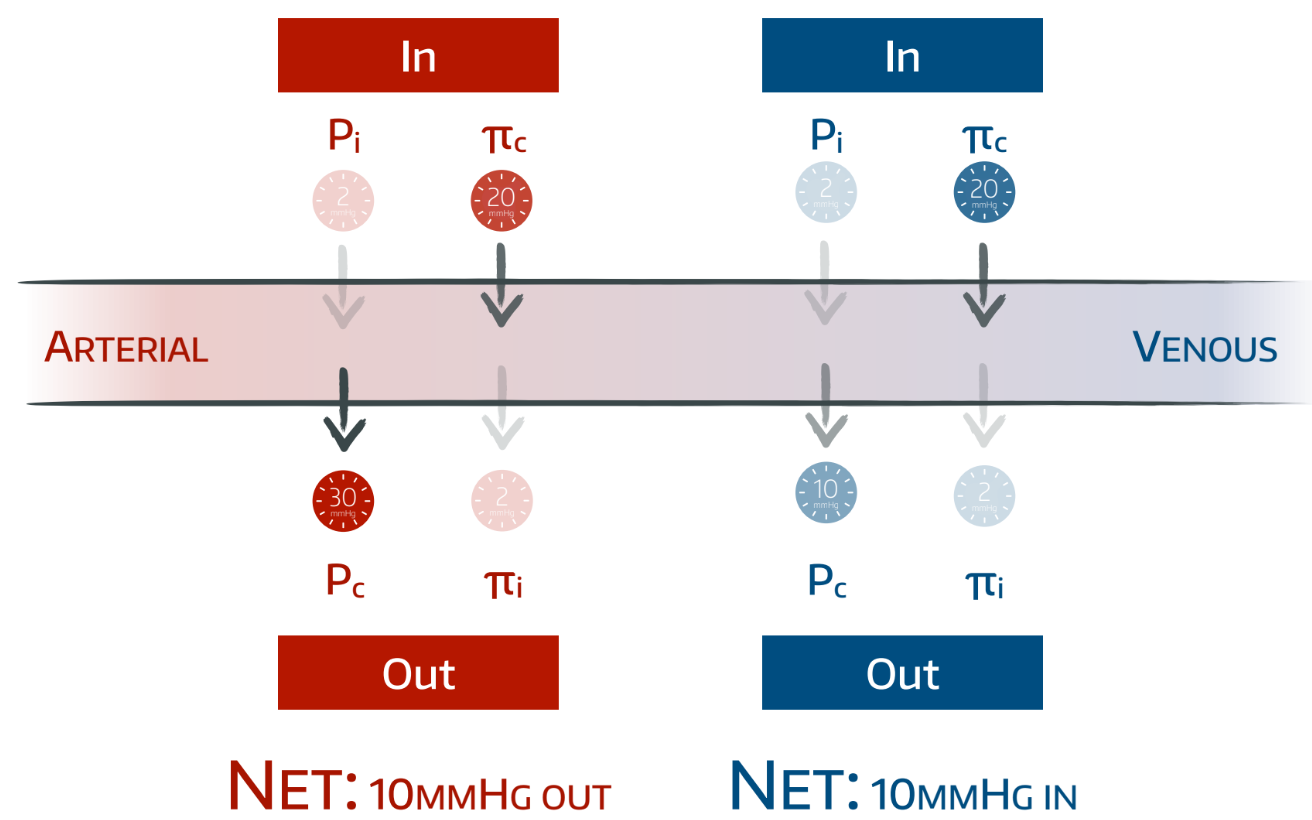
Where:
- Kf = glomerular ultrafiltration coefficient
- PG = Glomerular hydrostatic pressure
- PB = Bowman’s capsule hydrostatic pressure
- πG = Glomerular oncotic pressure
There are other forces at play, such as the viscosity of the fluid, friction to the flow of the fluid and interstitial pressure causing compression of renal tubules, however these are generally ignored.
Syllabus
- PB_BK_49 Structure and function, renal circulation
- PB_BK_50 Blood flow and glomerular filtration, plasma clearance and tubulo-glomerular feedback
- PB_BK_51 Tubular function and urine formation; transport processes
- PB_BK_52 Assessment of renal function
Useful Tweets
Pay attention to this thread:
— Ed (@Rx_Ed) May 18, 2022
Sodium/Glucose Cotransporter *2* (SGLT2) receptors are in the *1st* part of the proximal tubule, where 90% of glucose reabsorption occurs & also where SGLT2 inhibitors like empagliflozin work.
SGLT *1* receptors are in the *2nd* part of the tubule. pic.twitter.com/2UESZb8rqF
References and Further Reading
Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.