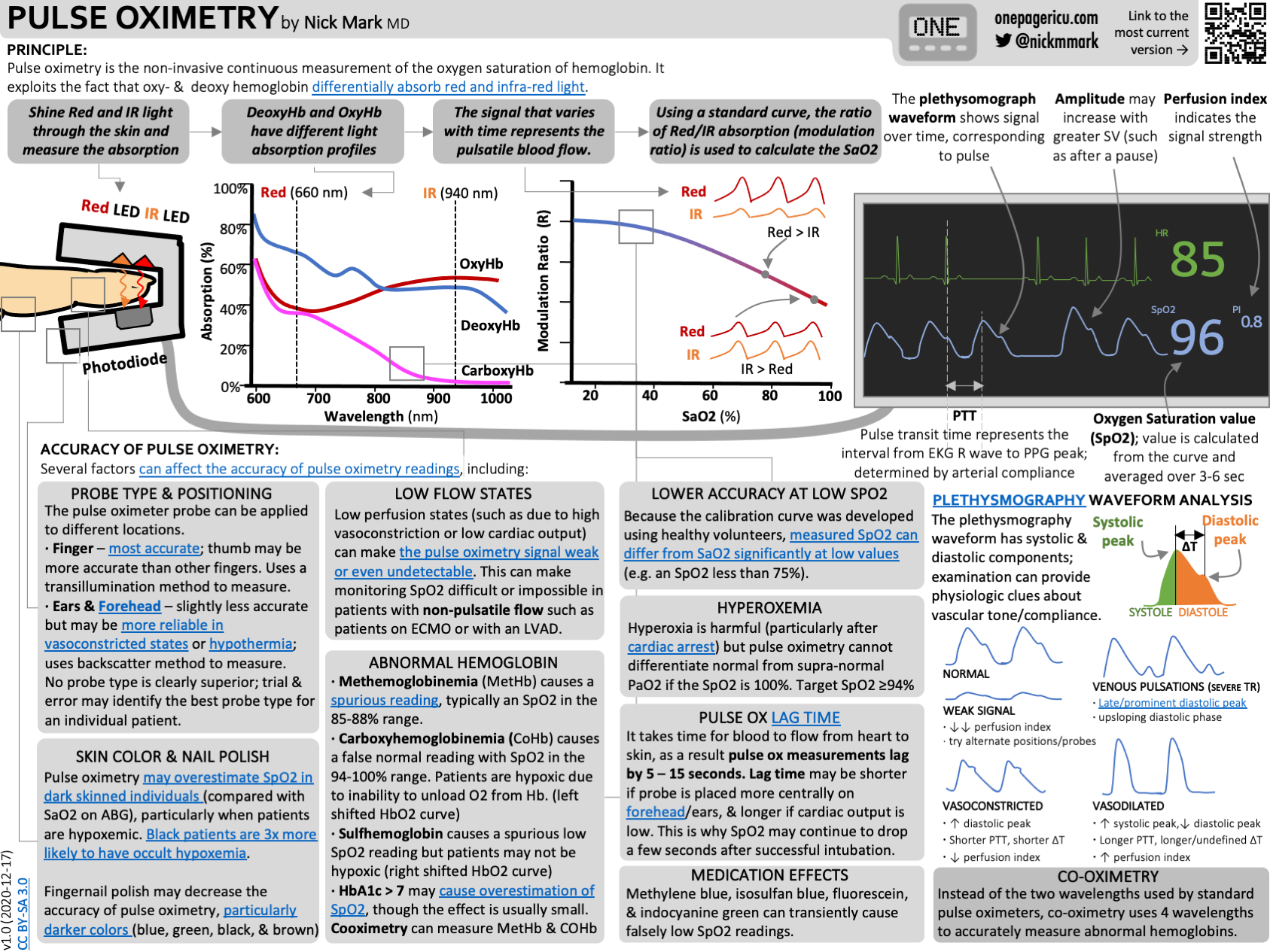
Pulse Oximetry

Take home messages
- Pulse oximetry is a very useful piece of monitoring equipment, but you need to know whether the number it's giving you is reliable and accurate
- By understanding how it works, you can decide whether the number is likely to represent the genuine oxygen level in the patient's blood
Podcast episode
Choose one.
Ask an anaesthetist what they would choose if they had to give an anaesthetic and could only have one piece of monitoring equipment, and usually it's a toss-up between:
- End Tidal CO2
- Pulse Oximetry
They're both incredibly powerful bits of monitoring kit as long as you know how to use them.
End tidal CO2 tells you:
- Patency of the airway
- Efficacy of ventilation
- Evidence of obstruction to air flow
- Cardiac output sufficient to supply CO2 to the lungs
Pulse Oximetry tells you:
- Oxygen level in the patient's blood in their peripheral vasculature
- Heart rate
- Heart rhythm
Personally I'd choose the sats probe, but hey - it just wouldn't be anaesthetics if we all agreed now, would it?
Know your kit.
The key, as with everything involving equipment and machinery, is to know your kit so well that you can accommodate effectively for the times when it goes wrong, and be able to determine whether an unexpected value is due to a patient problem, or a machine problem.
So with that - how does it work?
Pulse Oximetry allows us to non-invasively measure oxygen saturations.
This means the percentage of haemoglobin that is bound to oxygen, and not the total amount of oxygen present in the blood, and it's important to understand this distinction.
The key underlying principle that makes this whole process work is that molecules of different shapes and sizes can absorb light at specific wavelengths.
Oxyhaemoglobin (HbO2) and deoxyhaemoglobin (Hb) have different absorption spectra, meaning they absorb different wavelengths of red and infrared light to different extents.

- Oxyhaemoglobin absorbs more infrared light, and reflects more red light, giving it the bright red appearance that we know and love
- Deoxyhaemoglobin absorbs more red light, and reflects more infrared, giving it that ominous dark appearance that we don't love quite so much
If we plot the absorption coefficient of Hb and HbO2 over different wavelengths, we can see that Hb absorbs red light to a much greater extent than HbO2 as demonstrated on the graph above.
So in theory, if we shine a red light, and an infrared beam through some samples of blood, we can detect how much is absorbed, and therefore work out the proportion of haemoglobin that is either oxygenated or deoxygenated.
Your OSCE answer to 'how does a pulse oximeter work?''
- Pulse oximetry uses infrared absorption spectrometry to determine the proportion of saturated haemoglobin present in pulsatile arterial blood via a transcutaneous emitter and detector within a probe, usually on the finger or ear
- Oxygenated haemoglobin absorbs infrared radiation at a wavelength of 940 nm to a greater extent than deoxygenated haemoglobin
- Deoxygenated haemoglobin absorbs red light at a wavelength of 660 nm more than oxygenated haemoglobin
- Light emitting diodes emit pulses of red and infrared light every five to ten ms, each time followed by an ‘off’ cycle to allow for subtraction of ambient light interference
- Then, by employing the Beer Lambert Law it can determine the degree of absorption and therefore the relative proportions of oxy- and deoxygenated haemoglobin present
What are the components of a pulse oximeter?
- Probe
- 2 light emitting diodes
- Photo detector
- Cabling
- Microprocessor connected to display*
*Displays three parameters
- Waveform
- Oxygen Saturations
- Heart rate
The Beer Lambert Law
If I have a light source on one side of the blood, and a detector on the other, then I can measure how much light gets through, and work out how much was absorbed.
Now it makes fairly logical sense that the more blood there is between the source and detector, the greater the degree of absorption, and this is where the Beer Lambert Law comes into play.
- The Beer Lambert Law states that the absorption of light through a substance is directly proportional to the length of the path and concentration of the substance doing the absorbing
For exam purposes, use the following:
- Beer’s law = absorption is directly proportional to the concentration
- Lambert’s law = absorption is directly proportional to the length
I remember that lambda = length, and beer is either weak or strong (concentration)
How does the machine know?
It's all well and good churning out a number of 'how much light has been absorbed', but how does the machine know what oxygen saturations this translates to?
The answer is by using known validated tables of absorption spectra data from experiments in healthy volunteers breathing a hypoxic gas mixtures.
This is why people often say that the sats probe isn't validated below about 75% - because they couldn't test the healthy volunteers that low.
What on earth is an isobestic point?
This is classic FRCA exam fodder with little to no clinical relevance.
The lines in the graph cross over, meaning they must have equal absorption at that particular wavelength.

They actually cross over at two points, but the other point is off the left of the graph.
By definition, the wavelengths at which oxy- and deoxyhaemoglobin demonstrate equal absorption are called the isobestic points and occur at:
- 590 nm
- 805 nm
Some machines may use isobestic points as a helpful calibration reference point, as the absorption is only proportional to the haemoglobin concentration at this wavelength.
Your job is just to be aware of them for exam purposes.
You need pulsatile flow.
Sats probes don't work very well with cardiac bypass or ECMO, because the blood flow isn't pulsatile.
If you think about the pulse oximeter sat on the patient's finger, there are quite a few structures between the light emitting diode and the detector that will absorb light:
- Skin
- Muscle
- Bone
- Fat
- Blood
- Nail polish
Most of this will be constant, and the only thing that changes is the pulsatile arterial blood flow.
We can use this to our advantage, by simply subtracting the constant component of the signal, and amplifying the variable arterial bit that we're interested in.
Sats probes do a pretty darn good job of this when you realise that the arterial component only forms around 2% of the overall signal.
Why is my sats trace not working?
There are few things more scary than beep beep boop.
The hairs on your neck stand up, your palms start to sweat as you wonder what you've done wrong, only to remember that that sats probe is on the same side as the blood pressure cuff and the same thing happened five minutes ago.
There are also few things more frustrating than a persistently rubbish trace, with one solitary little star next to a very non-committal 88% that was 72% a minute a go and will be 97% in eight seconds time.
If you know the sources of error with pulse oximetry, then you can troubleshoot a dodgy trace and hopefully get that lovely waveform back on the screen.
Movement
- A moving finger, or a probe that's being leant on and moving around too much will give a poor trace
Perfusion
- This is common - a low sats reading caused by low blood pressure rather than hypoxia
- If the pulsatile flow in the finger is insufficient to get a reading then the probe won't work, so double check that your patient's blood pressure is within acceptable limits
Abnormal haemoglobin
- Blood loaded with carboxyhaemoglobin will be falsely reassuringly red, with high sats on the monitor
- Methaemoglobin, however, is a scary 85% even though the patient isn't necessarily hypoxic
- Hyperbilirubinaemia can also give you a falsely low reading
Carboxyhaemoglobin, hyperbilirubinaemia and methaemoglobin can be detected by CO-oximeters that use many more wavelengths.
Intravenous dye
- Don't panic if the sats plummet to 65% after the surgeon injects Methylene Blue - they're just keeping you on your toes
Poor pulsations
- As mentioned previously, if there's no pulsatile flow then the probe won't work
- This also applies to irregular pulsations or venous pulsations as seen in tricuspid regurgitation
Other interference
- Ambient light
- Interference from Diathermy
- Other machinery
Our favourite YouTube Video
Hypoxia OSCE station
Everything you could possibly want to know
These amazing infographics have been created and generously shared by Dr Nick Mark at ICU onepager which you should definitely go check out - they're awesome.
Useful Tweets
Fresh IBCC chapter on ABG, VBG, & pulse oximetry
— 𝙟𝙤𝙨𝙝 𝙛𝙖𝙧𝙠𝙖𝙨 (he/him) 💊 (@PulmCrit) April 28, 2023
💉Pulse oximetry is the default for assessing oxygenation, but it has numerous limitations
💉Peripheral VBG is fine for eval of pCO2 & pH, unless the venous sat is crazy low
💉Don't forget end tidal CO2!
(https://t.co/7kXyCmm9YD) pic.twitter.com/PHcSqsRpkl
So nail Polish absolutely does! And so does skin colour. Genuinely excellent recent publication saying so.https://t.co/UP69801oaA The problem isn't the device, it's the population used to set the reference.
— Joanna Poole 💙 (@jopo_dr@critcare.social) (@Jopo_dr) April 2, 2021
References and Further Reading

Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.
