Propofol
Podcast episode
Take home messages
- It's definitely probably almost certainly our favourite drug
- You need to know it inside out for the exam
- Be very cautious in patients with low blood pressure
A spot of history
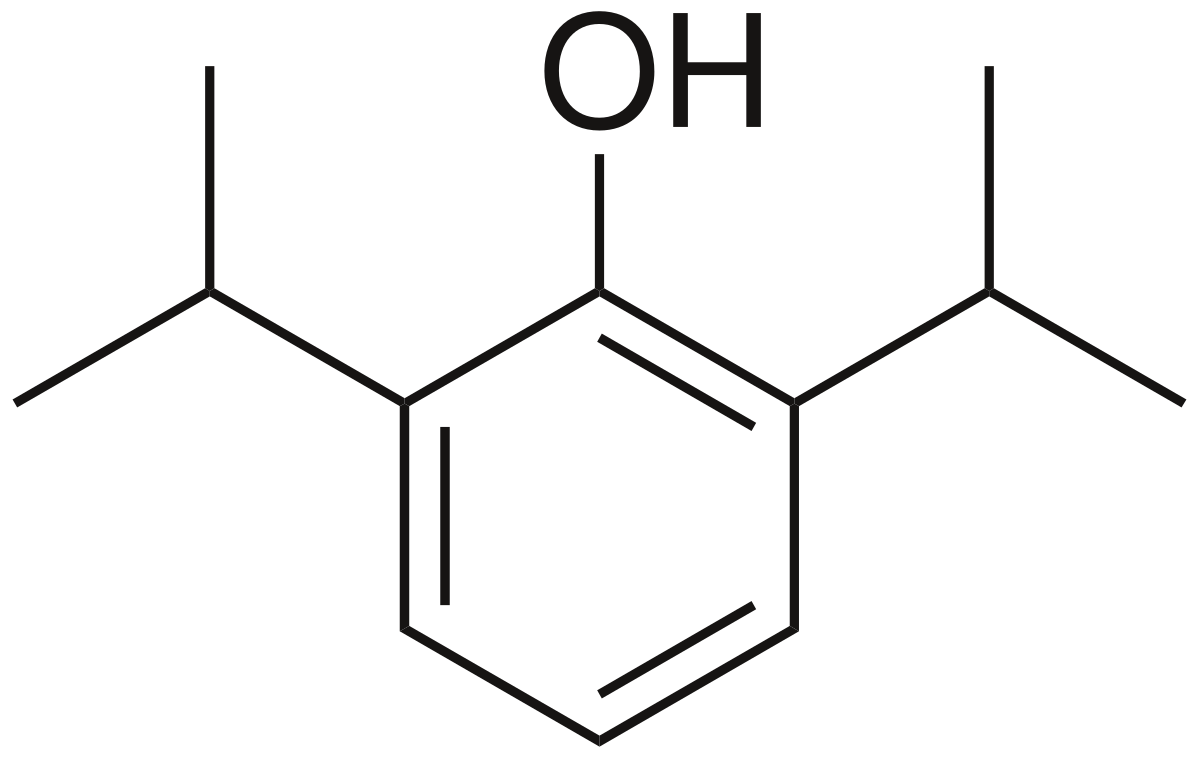
In 1973, after isolating a bunch of compounds and testing them in mice, veterinary anaesthetist Dr Iain Glen found that 2,6-diisopropylphenol was rather good at knocking them out - and even better - only temporarily.
Phenol is quite good at knocking people out, but it's a smidge too permanent for our liking, so we stick a couple of isopropyl groups on and suddenly it's a marvellously safe and reliable way to induce 'the best sleep I ever had'.
Initially propofol was dissolved in polyethoxylated caster oil, which did indeed allow it to be administered intravenously, but also caused enough anaphylaxis for the sensible decision to switch to soybean oil to be made.
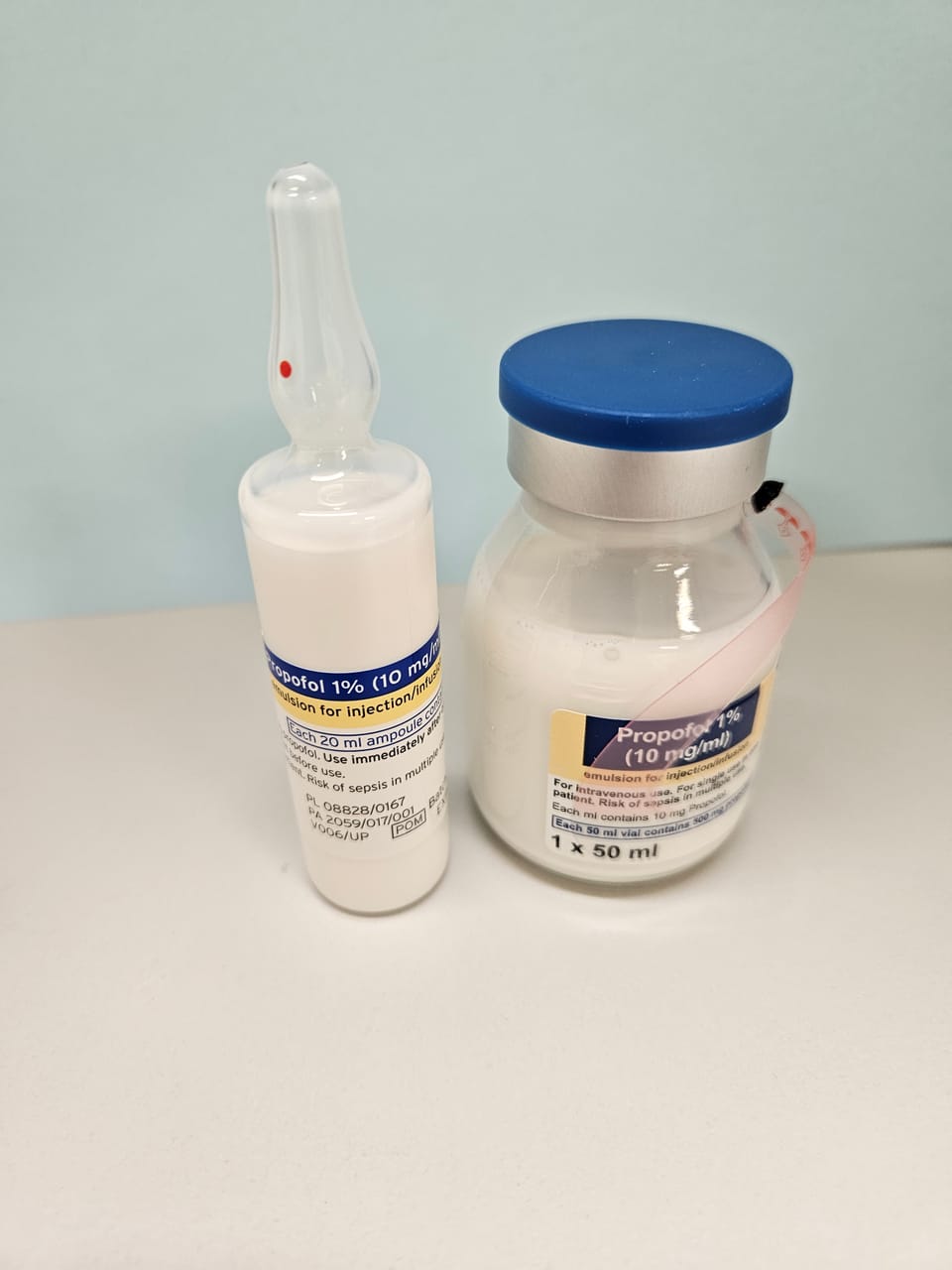
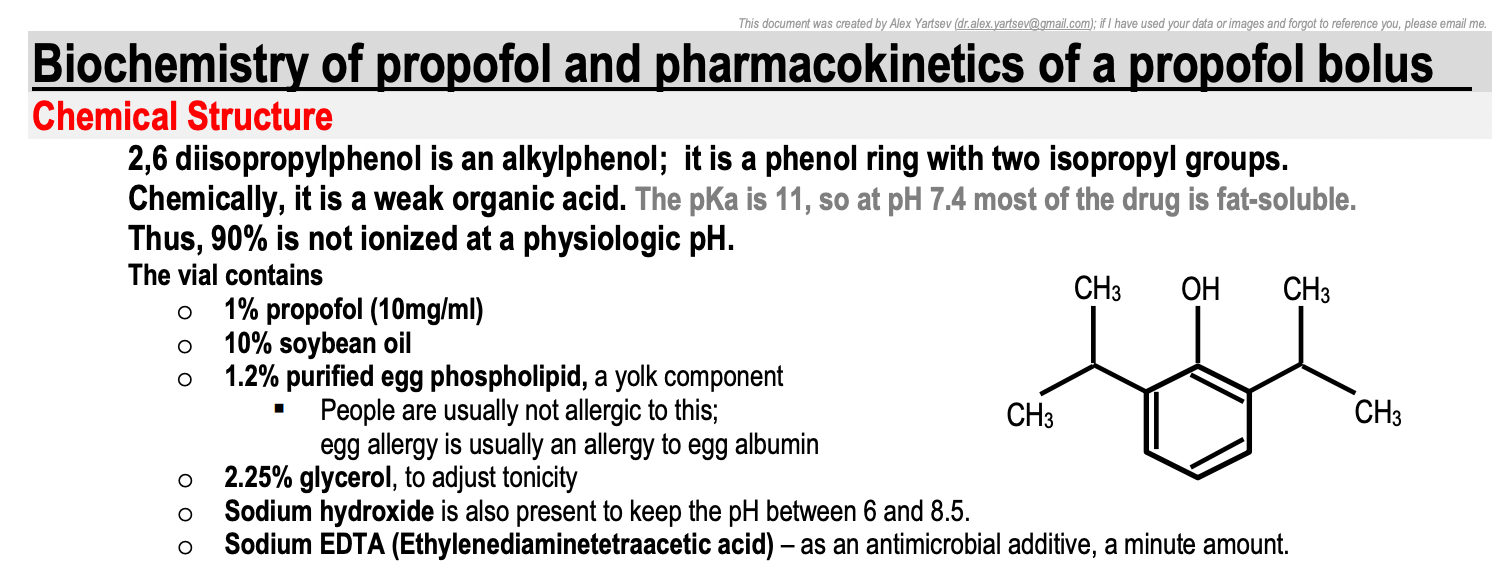
What's actually in the vial
Due to its enormous penchant for dissolving into fat, propofol is presented as a white lipid emulsion.
You need to be able to recite the following mantra:
- 1% propofol (10mg/ml)
- 10% soybean oil
- 1.2% egg phospholipid
- 2.25% glycerol, to adjust tonicity
- Sodium hydroxide to maintain pH between 6 and 8.5
- Sodium EDTA to prevent bugs growing
You can give propofol to patients with egg allergy, because egg allergy is usually to the albumin (white) rather than the yolk, where the phosopholipid comes from.
Likewise the allergenic proteins have been removed from the soybean oil, so soy allergy isn't generally an issue.
Tell me about propofol
When asked in the OSCE or viva scenario for the entirety of your knowledge on a certain drug, it's best to approach with a standardised structure, for the sanity of both yourself and your examiner.
Something along the lines of...
- Class and uses
- Mechanism of action and dose
- Clinical effects and side effects
- Pharmacokinetics - absorption, distribution, metabolism, excretion
...is at least a decent start.
The molecule
Class and uses
- Intravenous anaesthetic agent
- Alkylphenol - 2,6 - di-isopropylphenol to be exact
- Used for induction and maintenance of general anaesthesia
- Used for sedation of patients on intensive care
Also used for refractory PONV and refractory status epilepticus.
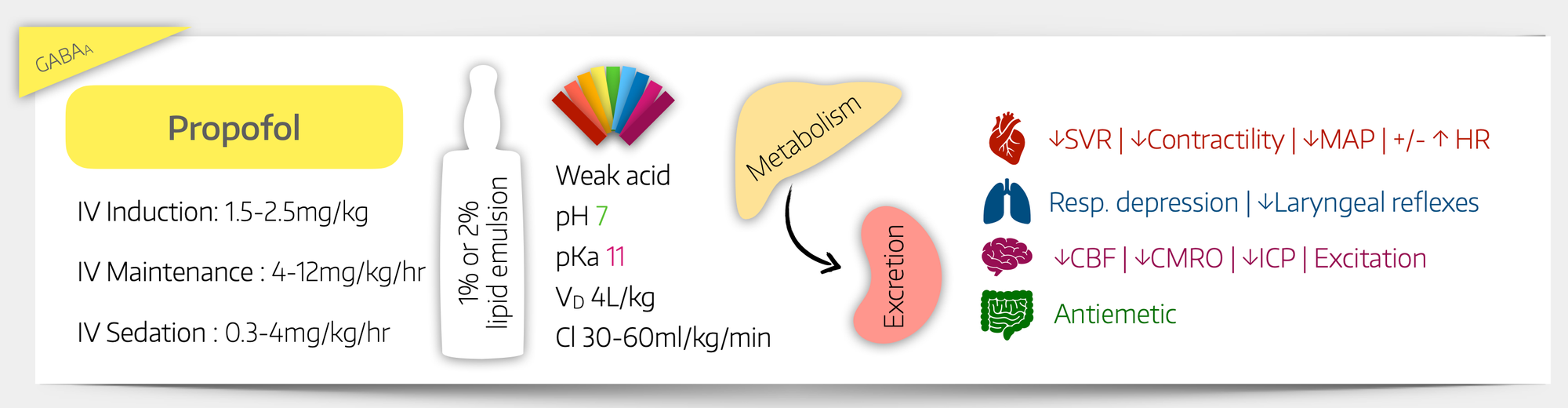
Mechanism of action and dose
- Positive allosteric modulator at the GABAa and glycine receptors
- Inhibitor of nicotinic acetylcholine receptor and serotonin (5HT-3) receptor
- Induction dose is 1-2.5mg/kg
- A plasma concentration of around 5 microgram/ml is needed for general anaesthesia
Clinical effects on the body
When talking about effects, it's generally best to break it down by bodily system.
Some people talk about the 'effects' and 'side effects' separately, but others just clump them all together by system. Your choice.
Neurological
- Anaesthesia*
- Reduced cerebral O2 consumption
- Reduced intracranial pressure
- Antiemetic
- Antipruritic
- Anticonvulsant
- Can cause hiccups
- Some patients demonstrate subcortical excitation (not seizures) which can produce a shivering effect
*Onset of action is one arm-brain circulation
Respiratory
- Respiratory depression
- Can cause apnoea if large doses given
- Suppression of laryngeal reflexes useful for supraglottic airway use
- Mild bronchodilator
Cardiovascular
Indirect via switching sympathetic tone off
- Reduced heart rate
- Reduced vascular resistance, sometimes with reflex tachycardia
- Reduced blood pressure (MAP)
- Reduced central venous pressure (MSFP)
The net effect is of relatively preserved cardiac output, just at a lower pressure, lower resistance flow.
This is fine for the majority of patients, but use extreme caution in already hypotensive (particularly cardiac) patients, who may not tolerate a further drop in MAP very well at all.
Renal
- Renal hypoperfusion if significant drop in blood pressure
- Green urine
Haematological
- Can cause hyperlipidaemia if you give loads for a long time
- This can lead to propofol related infusion syndrome
Other miscellaneous stuff
- Hurts on injection - give some 1% lidocaine first
- Can't use it for long term sedation in kids
Here's a pretty picture
Pharmacokinetics
Absorption
- Given intravenously
- If you’re interested, these people tried giving it orally and essentially all of the propofol administered is metabolised by either the gut bacteria or first pass metabolism, meaning only 11mg of 400mg administered was actually absorbed
You do not need to know this for the exam.
Distribution
- Volume of distribution is 4 litres/kg body weight for a bolus*
- Highly lipophilic and rapidly redistributes into fat
- pKa 11
- Weak organic acid, so almost entirely unionised at physiological pH
- 98% protein bound
- Does cross the placenta, but not thought to be directly harmful to the foetus
- Bolus half life = 120 seconds**
- Half life from steady state = 5-12 hours
*2.1 l/kg for a steady state infusion
**The wearing off of a bolus dose is largely due to redistribution away from the effect site, into other fatty tissues, rather than elimination from the body
Propofol is enormously fat soluble, as well as being highly protein bound in the plasma.
This means that the drug rapidly distributes throughout every bit of fatty tissue in the body, and what remains in the blood is bound to proteins.
This is why propofol wears off so quickly, and also why it has a large context sensitive half time. (see below)
Metabolism
- Hepatic metabolism mainly via CYP450
- High hepatic extraction ratio of 0.8 - 0.9, meaning very high first pass metabolism if administered orally
- 40% metabolised via conjugation to glucuronide
- 60% to quinol compound, which then goes to glucuronide or sulfate
If you're interested, clearance of propofol is faster than hepatic blood flow, meaning there must be some other place in the body that it's also getting metabolised, but we're not totally sure where that is.
Excretion
- Renal excretion
- Clearance 30-60 ml/kg/minute
- Elimination half life of approximately 8 hours
- Distribution half life after single bolus dose is 2 - 8 minutes
- Context sensitive half life at 8 hours is approximately 40 minutes
Don't be surprised if the urine is a little green - it's the harmless metabolic breakdown products.
A recap of CSHT
We've talked about context sensitive half time here but we'll gladly wax lyrical a little here as well.
If you infuse propofol for a few minutes and then switch it off, the patient wakes up fairly promptly.
If you infuse it for a few hours, the patient takes a lot longer to wake up after you hit stop.
This is because propofol accumulates in the fat stores in the body, and then leaches back into the plasma after the infusion stops.
This 're-infusion' maintains a certain plasma concentration and prolongs the anaesthetic effect.
The longer the infusion, the more propofol has seeped into the fat, and the longer the effect - the context is simply the duration of the infusion.
TIVA
If you really really like propofol then you can use it for your entire anaesthetic if you like.
You can find more about TIVA and TCI here

Is there anything like it?
The only drug we have that's even remotely similar is fospropofol, which is propofol with a phosphate group stapled onto the side, making it water soluble.
This makes it water soluble, so it doesn't hurt so much on injection and there's much less risk of hyperlipidaemia.
However...
Fospropofol is a prodrug, metabolised in the liver to propofol, phosphate and... formaldehyde.
The leaflet says there isn't a clinically significant increase in the amount of formaldehyde detected in the serum after giving fospropofol, however there also isn't any long term data on what happens after wilfully injecting a known carcinogen into patients' blood either.
Here's our video
Here are all the other induction agents

References and Further Reading
Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.