Post Dural Puncture Headache
Take home messages
- A tension headache is the commonest cause of post-partum headache
- Dural puncture headaches need sorting out to avoid potential complications
- Don't forget the other important causes, of which parturients are at increased risk
Headaches
I had a headache three days after my first child was born, and I'm the father.
The commonest cause of headache after delivery is a tension headache.
- Over 30% of parturients develop a headache within seven days of giving birth
- Three quarters of these are migraines or tension headaches
If, however, there is a clear history of the mother having had a dural puncture, then clearly the probability of a post-dural puncture headache (PDPH) goes up somewhat markedly.
The key is not to forget about the other sinister causes that may be responsible.
- 25% of peri-partum headaches are caused by pre-eclampsia
Severe causes of headache to rule out
- Venous sinus thrombosis
- Pre-eclampsia
- Meningoencephalitis
- Intracranial haemorrhage
Even if there is an obvious history
August Bier 1898
Describing a personal experience of post-dural puncture headache after playing around with his assistant, some enormous spinal needles, and an unspecified quantity of cocaine:
“Toward the evening I was forced to take to bed and remained there for nine days, because all the manifestations recurred as soon as I got up. At midnight a violent headache set in that quickly became insupportable.”
Diagnosing the headache
There are clear guidelines set out by the International Headache Society on how to properly diagnose a headache.
You can find the full guidelines here, or download the freely available 'pocket version' below if you're interested
Headaches can be primary or secondary.
Primary Headaches
- Tension Headache - dull, diffuse tightness around the head
- Migraine - classically throbbing unilateral pain +/- aura +/- nausea
Secondary Headaches
Vascular problems
- Venous sinus thrombosis
- Subarachnoid haemorrhage
- Other intracranial bleed
- Stroke or ischaemia
- Dissection
- Posterior Reversible Encephalopathy Syndrome (PRES)
- Reversible cerebral vasoconstrictive syndrome
- Pituitary apoplexy
Non-vascular problems
- Post-dural puncture headache
- Benign intracranial hypertension
- Hypertension and pre-eclampsia
- Space occupying lesions
- Pneumocephalus
Infective problems
- Sinusitis - treat with antibiotics and decongestants
- Meningitis - fever, rigidity, mental status change
- Generalised sepsis
Pharmacological problems
- Caffeine withdrawal
- GTN and calcium channel blockers
Treatments for primary headaches
- Paracetamol
- NSAIDs
- Sumatriptan
How to spot a post-dural puncture headache?
The IHS states that a PDPH occurs due to low cerebrospinal fluid pressure, and it almost always occurs within five days of the procedure.
Features include:
- Front to back (fronto-occipital) distribution
- Positional - worse on standing
- Stiff neck
- Tinnitis
- Photophobia and visual disturbance
- Cranial nerve palsy
- Positive Gutsche sign - increasing abdominal pressure can help relieve the headache by increasing intracranial pressure
The vast majority will self-resolve without intervention, but leaving them untreated for a longe period of time can result in significant complications, so an epidural blood patch may be required.
How can you reduce the risk of a post dural puncture headache when performing a spinal injection?
- Use a smaller needle
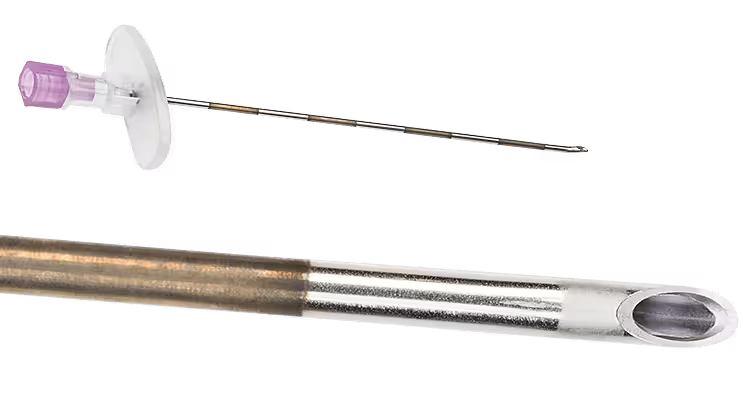
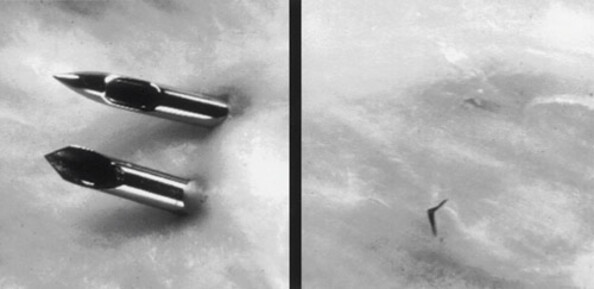
- Pencil point needle rather than cutting bevel
- Re-insertion of stylet prior to removal of spinal needle
- Experienced operator
- Other techniques to improve first pass success - Optimal positioning and use of ultrasound
What is Gutsche's test?
- Press on the abdomen under the right costal margin while patient is in a sitting position
- If this relieves the headache, this vaguely supports a diagnosis of PDPH
- It also suggests that an epidural blood patch may be effective
The idea is that the hepatic squeeze pushes blood into the epidural veins and squeezes CSF back up into the head.
You have to push really hard, it hurts, and probably doesn't add much to your rapport with an already distressed mother.
What do I do about it?
We tell people that they should have plenty of fluids, caffeine and rest, and that the vast majority of PDPHs will go away by themselves.
This is partly true - most will resolve spontaneously, especially if caused by a dinky spinal needle rather than a Tuohy battering ram.
Fluids and bedrest are not actually effective treatments for PDPH, but they don't do any harm, they treat other causes of headache and the post-partum mother probably needs more rest and fluid anyway.
The key is giving them plenty of multi-modal analgesia, as allowed by breastfeeding etc. and talking to the mother about a possible procedure.
The procedures
- Epidural blood patch remains the most effective treatment for a true PDPH
- Sphenopalatine ganglion block is another option, but not widely done in the UK
In case you're wondering, no you can't whack in a prophylactic EBP after ploughing through the dura and then siting the epidural a space higher. It doesn't work and just carries more risk.
How to do a blood patch
Data suggest that complete, permanent relief of PDPH by a single blood patch occurs in 31%-50% of patients after puncture with an epidural needle, and up to 75% after a spinal needle. Complete or partial relief occurs in approximately 90% of patients.15–17 About 30% of patients require a second blood patch.
Preparation
- ID, informed consent, dedicated equipment, sterile set up, skilled assistance, monitoring as with any procedure we do
- Two anaesthetists, at least one senior and the other to do venepuncture
- (make sure venepuncture kit compatible with neuraxial kit, e.g. NRfit)
Procedure
- Locate epidural space with loss of resistance technique as per usual epidural technique
- Sterile venepuncture, aspirating 20ml autologous blood, remove venepuncture needle
- Inject blood slowly via Tuohy needle
- Stop when patient experiences back pain or they get symptomatic relief
- Remove Tuohy needle
- Lie patient down for 2 hours
Do not perform if patient febrile or has high white cell count.
Can cause transient bradycardia.
If it doesn't work, they need head imaging.
What about caffeine?
- Thought to cause vasoconstriction
- Dosage from 75mg to 500mg have been studied, both PO and IV
- Evidence was rubbish quality but suggested it might help
- You have to think about the cardiovascular and neurological side effects and consequences of telling a post-partum breastfeeding woman to take the equivalent of three red bulls a day
- Basically - if they already use caffeine, then continue to use it, but don't start smashing cans of Monster in the hope of ridding yourself of a headache it probably won't fix
Even if it does help with the headache, the newly-caffeinated raging steam-baby at three in the morning will probably cause another one.
When was this examined?
- March 2017
- March 2013
Really helpful tutorial of the week
Useful Tweets and Resources
Here's NYSORA's video on performing an epidural blood patch (shared with permission as always).
Recently we had a case of CVST in a patient with PDPH, In this nice review of the current literacases evokes a possible connection beween inadvertent dural puncture and the risk of this rare complication https://t.co/yyCuw2iwJa pic.twitter.com/aIsNZWsl2O
— Margarita Borislavova (@drborislavova) December 5, 2024
Accidental dural puncture
— 𝘈𝘯𝘢𝘦𝘴𝘵𝘩𝘦𝘴𝘪𝘢 (@Anaes_Journal) September 30, 2024
• Inserting an intrathecal catheter does not decrease the incidence of PDPH but does decrease the need for epidural blood patch.
• There is no benefit in leaving the catheter in for 24 h postpartum.
• In patients with an intrathecal catheter,… pic.twitter.com/OJ37FRczI0
References and Further Reading
Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
