OSCE Station #13 for the Primary

Practical skills station
You are the anaesthetic registrar on call for the evening.
Your CT1 colleague has called you for assistance, having independently anaesthetised an ASA1 patient for an appendicectomy.
It was a grade 1 intubation and they have just transferred the patient to the operating table, and connected to the machine.
Please assess and manage the situation as you would in your day to day practice.
All of the equipment required will be provided for you.
Station set up
This is a practical skills station of moderate fidelity. The manikin may be of variable completeness but the only requirement is that it can be intubated.
- Manikin intubated attached to anaesthetic machine
- Endotracheal tube tied at 26cm at teeth
- Sevoflurane running with O2/Air mix
- Drapes over patient
- Equipment available to candidate - laryngoscope, IGEL, LMA, BVM and facemask, stethoscope
Monitor set up
- Low tidal volumes
- High pressure alarm
- SPO2 to decrease from 95% to 85% over the first minute of the station*
- Airway pressure 40
- FiO2 0.4
*As soon as the candidate finds and manages the problem, the sats rapidly increase. If the candidate does not solve the issue, or only applies 100% oxygen, the sats continue to drop.
Mark scheme
- Notes abnormal observations - 2 marks
- Switches to 100% oxygen and increases flow rate - 2 marks
- Uses stethoscope to listen to the chest - 2 marks
- Assesses tube position at the teeth - 2 marks
- Deflates cuff and withdraws the tube - 2 marks
- Re-assesses the chest with stethoscope - 2 marks
- Reduces the FiO2, flow and adjusts sevoflurane appropriately - 2 marks
What other therapeutic manoeuvres may be required?
- Increasing PEEP
- Recruitment manoeuvre
- Hand bagging
Any 2 for 2 marks
What was your differential diagnosis for this clinical picture?
- Pneumothorax
- Airway obstruction
- Accept any cause of significant shunt
Any 2 for 2 marks
Why did the patient not respond to 100% oxygen?
- Large shunt due to endobronchial intubation - 2 marks
Tips and Tricks
If bad stuff is happening quickly in a practical skills scenario, there's a good chance it's an A problem, because A is the examiners' favourite letter to assess*.
*Well, it's definitely in the top three.
If you get into the habit of immediately:
- Applying 100% oxygen
- Increasing flow
- Assessing the tube position at the teeth and checking the breathing system tubing back to the machine
- Listening to the chest
Then you'll quickly pick up on pretty much any airway problem they can throw at you.
(e.g. the examiner deliberately standing on the tubing)
Signs of Endobronchial intubation
- A tube that's rather too many cm at the teeth (more than 25cm should be raising an eyebrow)
- High pressure alarms
- Poor sats despite a raised FiO2
- Poor tidal volumes
- A generally angry ventilator
- You might also see unilateral chest rise and hear unequal breath sounds
Key times to think about endobronchial intubation
- When you have a short patient
- When you have an obese patient
- When you position the patient head down
- In little kids where any head movement can move the tube in the trachea quite substantially
ChatGPT wrote us a poem about endobronchial intubation
In the depths of the airway's gentle curve,
Where breaths should flow with quiet verve,
A tube misplaced, a path astray,
Brings forth a challenge, come what may.
Endobronchial, the word so vast,
An intubation's shadow cast,
A breath intended for both lungs,
Now whispers where a song's unsung.
One lung's breath, the other's still,
A silent chest, an urgent thrill,
The signs arise, uneven chest,
A gasping call for urgent quest.
The patient stirs, discomfort clear,
A wheeze, a drop, a rising fear,
A prompt review, a careful ear,
To guide the tube where lungs adhere.
First, check the tube, confirm its place,
A stethoscope to lead the chase,
A chest rise missed, a capnograph,
These tools will guide, avoid the gaffe.
Adjust the depth, a measured slide,
Until the breath is not denied,
Withdraw, recheck, ensure the flow,
In both lungs now, a steady glow.
If signs persist, a different sight,
A chest X-ray to shed the light,
A picture clear, a view precise,
To see the tube in airway's slice.
Correct the course, return to norm,
Restore the breath, a vital storm,
A team at hand, with skill and grace,
To set the tube in proper place.
Through careful checks, the path aligned,
The breath restored, the patient fine,
A lesson learned, a skill refined,
In airways’ depths, we are defined.
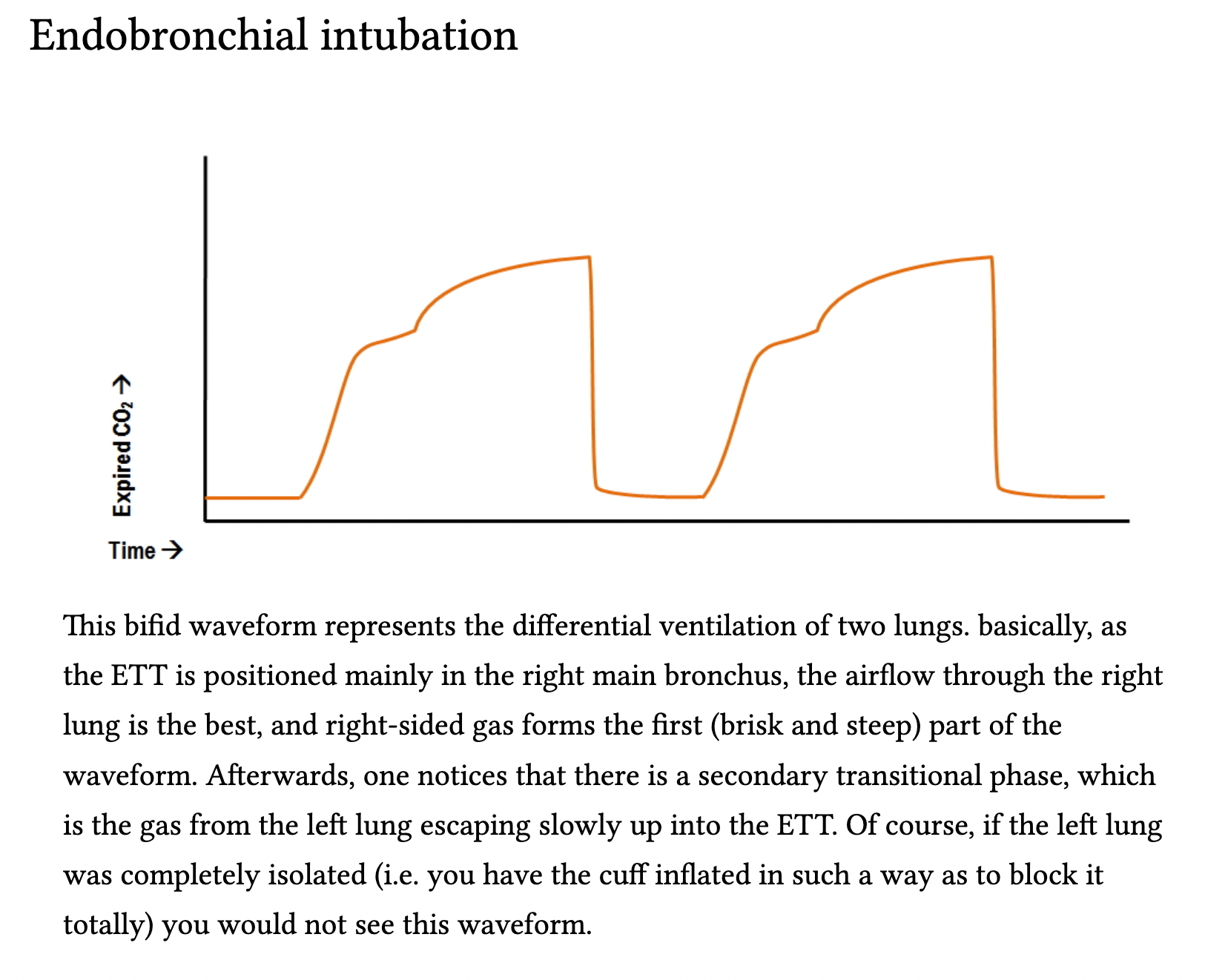
Here's a highly useful page from Deranged Physiology
(Shared with permission - click the image to go to the full page on pathalogical capnography waveforms)
Here's an amusing exchange of four anaesthetists throwing very polite shade at each others' intubating skills

