Obstetric Cardiac Arrest

Take home messages
- Do exactly what you would normally do for an adult
- Add in lateral uterine displacement
- Resuscitative hysterotomy should be done within 5 minutes
Obstetrics as an anaesthetist is scary
The Marmite of anaesthesia, obstetrics is a beautiful blend of high pressure, ridiculously acute work that requires you not only to be the medical registrar for labour suite, but to also be calm, reassuring and to manage a team of often very stressed and panicky people.
Oh, and it's the only time we poor anaesthetists have to think about more than one patient at a time.
Probably the scariest thought is what to do if your young, pregnant patient were to collapse in cardiac arrest.
Mercifully the incidence of cardiac arrest in pregnancy is generally very low - in the developed world at least - hovering around the 1:20 000 to 1:30 000 mark depending on your sources.
But now and again, suprises happen, and you need to be able to manage the scenario appropriately, and quickly.
Who do you want at a maternal cardiac arrest?
- Anaesthetics
- Obstetrics
- Neonatology
- Nurses
Why do mothers arrest?
Generally speaking, you need to be fairly young and healthy in order to carry a child to term, as the physiological demands on the mother's cardiovascular, respiratory and musculoskeletal systems are far from trivial.
With 140% of their usual circulating volume hammering around a low-pressure vascular system, these women's hearts are working hard, but usually can cope with it very well indeed.
What are the causes of maternal mortality?
This depends on where in the world you are, but assuming we're talking about a developed nation with decent healthcare (no comments please) available:
- Ischaemic heart disease
- Cardiomyopathy
- Sepsis
- Amniotic fluid embolism
- Haemorrhage*
*Haemorrhage becomes the leading cause of mortality once you start looking at developing nations and those with reduced access to adequate healthcare.
So why has my patient gone into cardiac arrest?
As the obstetric anaesthetist responding to a crash call, it's likely you may not have met the patient prior to managing their collapse, so part of the challenge is getting the bottom of why a young and presumed healthy woman has gone into cardiac arrest.
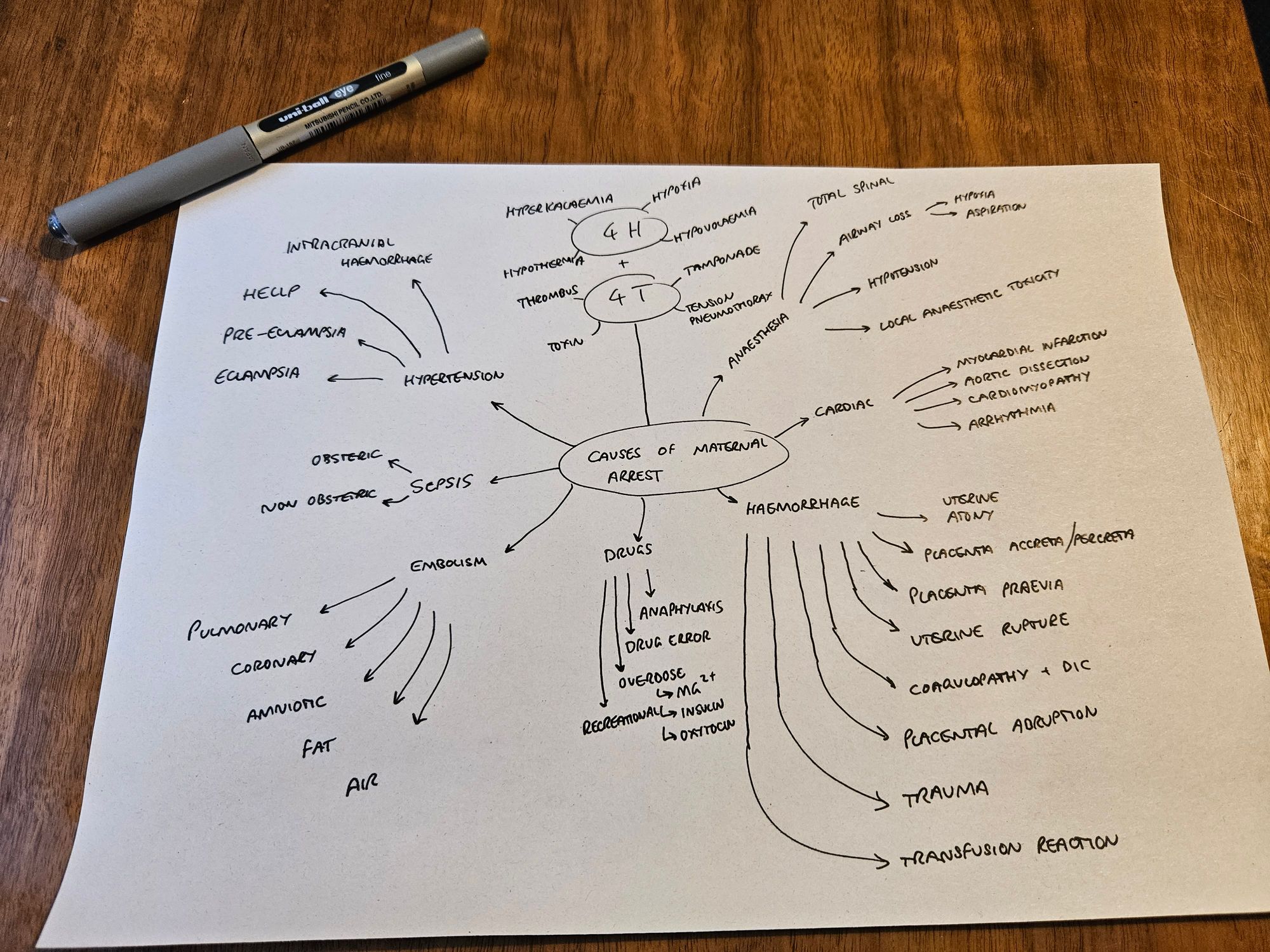
You're still doing your 4Hs and 4Ts as you would normally, but you also need to think about obstetric causes of arrest that might need some fixing as well.
The following image has a fairly comprehensive differential diagnosis:
As always - good CPR is paramount
Time and again, early and high quality BLS and ALS have been shown to make a huge difference to survival, and it's no different here.
This study found that if you start high quality CPR quickly, you give a pregnant woman in cardiac arrest a 58% chance of survival, but clearly this is going to depend on the cause:
- If the arrest is a complication of anaesthesia, and therefore likely rapidly reversible, the outcome is generally good
- If the arrest is the result of an underlying disease process then the prognosis is somewhat less favourable
So how do you manage a maternal cardiac arrest?
Take a deep breath, remember your training, and do the following:
- Call for help - 2222 Maternal cardiac arrest should bring you
- Adult cardiac arrest team
- Anaesthetics
- Neonatologist
- An obstetrician with a knife
2. High quality ALS
- 100-120 compressions per minute
- Manual left uterine displacement
- Early defibrillation as indicated
- Airway management with ETCO2 monitoring
- Resuscitation drugs at normal doses
- Resus fluids
3. Resuscitative Hysterotomy
- If no ROSC by four minutes
4. Identify and fix cause
- History from notes/obstetric team/family
- Arterial blood gas analysis
- Bloods
- Ultrasound
Lateral uterine displacement
CPR uses sternal pressure to generate increased intrathoracic pressure and push blood through the one-way system of blood vessels and valves to reduce hypoxic damage to the vital organs.
An occupied uterus tends to disrupt this process, from 20 weeks onwards, through three mechanisms:
- It makes CPR more difficult, because the abdomen gets in the way
- It increases oxygen consumption, in an already hypoxic patient
- It compresses the inferior vena cava, reducing venous return to the heart
To reduce this problem, you need a dedicated person at the arrest whose only job is to push the uterus to the side (ideally the left, but whatever you can manage).
This works better than the left lateral tilt we use after a maternal spinal, largely because CPR is vastly easier in a flat patient.
Why is airway management more challenging in maternal collapse?
- Reduced FRC due to abdominal pressure on diaphragm and weight of breast tissue on thoracic cage
- Increased oxygen consumption
- Mucosal oedema of pharynx and airway
- Breast tissue may make laryngoscope insertion more difficult
- Increased risk of airway bleeding
Do I need to alter my drug doses for resuscitation?
No.
Yes, pregnant women have different physiology, but this all pales into relative insignificance once the blood is stationary.
Furthermore, you're likely to be pretty maxed out on the cognitive front, and most anaesthetists can run through an ALS algorithm without thinking very hard, so just do that, and do it as well as you can.
- Stop oxytocin (negative inotrope and vasodilator)
- Stop magnesium
- Stop local anaesthetic infusions
Equally, don't fret about foetal scalp electrodes or CTG monitors when defibrillating - just get on with it.
The decision to cut
This is the scariest bit.
Rule 10
Most anaesthetists would agree that the hardest part of emergency front of neck access is the decision to cut, and the same applies to resuscitative hysterotomy.
- Hysterotomy should be performed where the woman collapsed, do not waste time moving them to theatre
Why get baby out?
As we mentioned earlier, a gravid uterus makes CPR much harder, increases the oxygen and cardiovascular demand on the mother and therefore reduces the survival rate of both patients.
Equally, if the mother is in cardiac arrest, then the uterus is no longer the best place for the foetus to be, assuming the baby has passed the threshold of viability.
Therefore a resuscitative hysterotomy should be performed within five minutes, to maximise chances of successful CPR.
After ROSC
Hopefully your resuscitative efforts are successful and both mother and baby make a full recovery.
However this requires a whole suite of post-ROSC care - not just a heartbeat - and the mother now has a long journey to returning to normality.
Haemostasis
- The incision was made with a blood pressure of (not much/even less)
- Hopefully your patient now has enough blood pressure to bleed, so this will need attention before anything else
Cardiovascular support
- Post-ROSC syndrome involves substantial myocardial stunning, as well as any underlying pathology causing the arrest in the first place
- Your patient needs admitting to ITU for vasopressor and inotrope support as required to maintain a perfusing pressure to the brain
- Depending on your hospital policy, they may require targeted temperature management
Intubation and ventilation
It's likely that an airway was in place before ROSC, but either way, the patient definitely needs sedation and a tube now for the following reasons:
- Pain control and compassionate sedation
- Reduced cerebral metabolic demand
- Respiratory support after a likely aspiration
Antibiotics, nutrition and electrolytes
- As with any ITU patient - as many physiological parameters need to be optimised as possible to maximise the chance of a meaningful recovery
Useful Tweets and Resources
🔐 Emergencies in obstetric anaesthesia:
— 𝘈𝘯𝘢𝘦𝘴𝘵𝘩𝘦𝘴𝘪𝘢 (@Anaes_Journal) November 1, 2022
-Cat-1 LSCS
-Difficult/failed airway
-Massive obstetric haemorrhage
-Hypertensive crisis
-Neuraxial anaesthesia
-Cardiac arrest
This review from @charlieprior11, @Intrathecalcat and @antonchau1 has everything!
🔗https://t.co/EhrFkK72f1 pic.twitter.com/iio8tZUAHf
Out now: great must-have resource for maternity units - a quick reference guide for obstetric cardiac arrest. Amazing collaboration between @ResusCouncilUK @mbrrace and @OAAinfo Thanks to all involved for getting this off the ground
— 🌏Emma Evans ♻️ (@DrEdebates) August 7, 2021
▶️ https://t.co/SqqWWwhP8Q
#teamwork pic.twitter.com/fBQZ0qBgA8
References and Further Reading

Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.
