Myasthenia Gravis
Take home messages
- The key feature is fatiguable weakness
- You need to tell the difference between myasthenic and cholinergic crises
- Continue steroids and pyridostigmine if the patient is already on them
The highlights
- MG is the most common neuromuscular junction problem with a prevalence of around 1/10 000 in the UK
- Bimodal distribution <30 years old and >50 years old (usually younger women and older men)
- The key feature is fatigable weakness of skeletal muscle
- B-cell mediated autoimmune condition
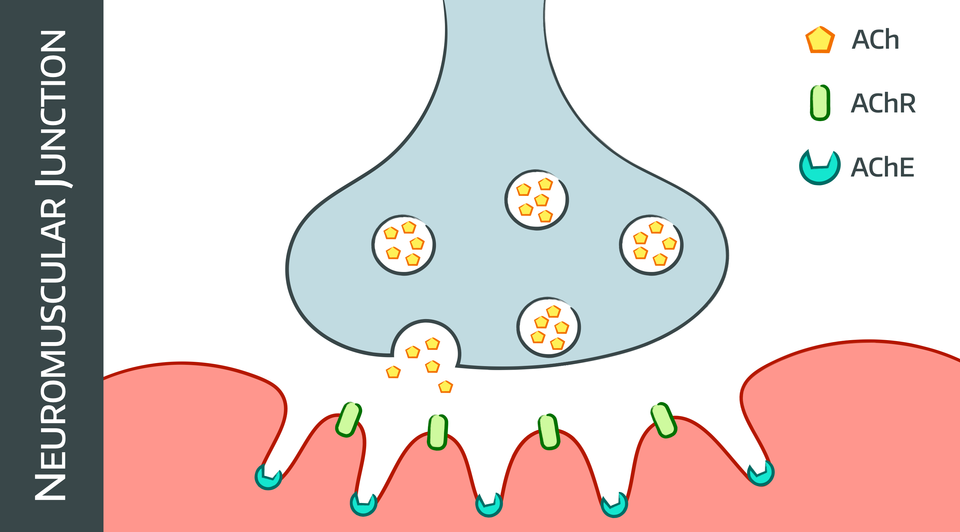
- 90% have IgG auto-antibodies against post-synaptic nACHR at neuromuscular junction
- Antibodies against AChR at the neuromuscular junction block the receptor, induce conformational change and crosslinking, and degrade the receptors
- Or to other things on the post synaptic membrane such as MuSK, LRP4**, or agrin
- 65% have hyperplasia of thymus
- 12% have a thymoma
- Associated with hyperthyroidism
*Muscle specific kinase
**Lipoprotein receptor-related peptide 4
Lambert-Eaton syndrome is similar but has autoantibodies to pre synaptic receptors.
You need to know how to treat a myasthenic crisis, and also how to safely anaesthetise someone with known MG, who is hopefully not currently in myasthenic crisis.
We don't really know why it happens, but we do know that the thymus is involved at least 75% of the time, so we pin the blame on that.
What it looks like
As with many conditions in medicine, the answer is variable, but it always involves some form of weakness, which can be:
- Mild and localised
- Severe and generalised, including respiratory and bulbar muscles
- No muscle wasting
- No fasciculations
- Normal tone
- Normal reflexes
- Normal sensation
Classically your patient will feel fine in the morning, and over the course of the day will become progressively weaker and more exhausted.
- Ptosis
- Diplopia
- Proximal muscle weakness
The types
- 15-20% have purely ocular symptoms
- 75% will see a progression to generalised weakness in three years
How is MG diagnosed?
- Clinical examination
- Serological testing - AChR antibodies, TFTs, anti-MuSK, anti-LRP4
- Neurophysiological testing - looking for fatiguability
- MRI to look for thymoma
The edrophonium or Tensilon test uses a short acting anticholinesterase to demonstrate a rapid (after 30 seconds) and transient (lasts 5 mins) improvement of symptoms.
Compound muscle action potential testing is the most commonly used neurophysiological study - basically if you keep stimulating the motor neurone, the muscle contraction steadily gets weaker, a term called decrement.
AChR antibodies are present in 80-85% of cases.
How is myasthenia gravis managed?
- Treat symptoms with anticholinesterases like pyridostigmine
- Immunosuppression with steroids and azathioprine
- Can escalate to mycophenolate mofetil, rituximab or methotrexate as required
- IVIG and plasma exchange for bulbar and respiratory symptoms or rapid disease progression
- Thymectomy
How to anaesthetise them
The main aim is minimising your effects on muscle weakness, and preserving respiratory function.
What are the key points for the anaesthetic assessment ?
- Bulbar symptoms
- Respiratory symptoms
- History of crises
- Dysphagia and dysphonia
- Other autoimmune conditions
- Current medications
Continue steroids and anticholinesterases perioperatively.
These patients should ideally be first on the list.
Regional anaesthesia
As with any major systemic disease process, if you can use regional or local anaesthesia and avoid the faff of GA altogether - that's usually a good shout.
- Use amides - ester metabolism affected by anticholinesterase medications
- Spinals and epidurals - extra caution for high block if bulbar or respiratory weakness
- Brachial nerve blocks - can block the ipsilateral phrenic nerve with respiratory complications
Sedation
- Use short-acting titratable agents
- Any sedation will exacerbate existing respiratory weakness
- Atropine and glycopyrrolate for secretions
If you have to use paralysis then do what you always do - roc and sugammadex.
General anaesthesia
- Use the shortest acting agents you can get away with
- The response to muscle relaxants will be unpredictable
- The reduced number of functional nAChR makes them relatively resistant to depolarising muscle relaxants - use rocuronium and give a very reduced dose*
- Reversal with neostigmine is also variable - too little and you get myasthenic crisis, too much and you get cholinergic crisis**
- TIVA can facilitate intubation without paralysis
- Lidocaine can also help with the laryngoscopy response, just note that it will enhance any neuromuscular blockade
- Ideally keep them on spontaneous ventilation with a bit of pressure support for short procedures
- For longer procedures use mechanical ventilation to rest the patient's respiratory muscles
- Consider atropine to prevent cholinergic crisis.
*Give aliquots of 1/10th the usual dose for intubation.
**Just use Sugammadex.
What if they miss a dose of pyridostigmine?
Your patient may be under anaesthesia when their next dose of pyridostigmine is due, and if missed this can present as weakness by the time the end of the operation finally comes around.
Consider giving some during the procedure if appropriate.
Post op
Clearly this is going to depend on the procedure and how you anaesthetised them, as well as how they fared during the operation.
- Small operation under regional with no respiratory concern - consider day surgery
- Intubated, long laparoscopy, residual O2 requirement - consider HDU for 24 hours
You may need to ventilate the patient on ICU for a while after a large or more invasive procedure, especially if substantial amounts of muscle relaxant is used or they're showing evidence of myasthenic crisis.
Risk factors for needing post-op ventilation
You know the drill - categorise or die.
Patient factors
- BMI >28
- COPD
Pathology factors
- MG for more than 2 years
- Bulbar or respiratory disease
- History of crises
- More than 750mg per day pyridostigmine
- FVC <2.9 L
- AChR antibody concentration >100 nmol/ml
- Noticable decremental response
Surgical factors
- >1 litre blood loss
- Lung resection surgery
Myasthenic Crisis
This is essentially severe respiratory muscle weakness leading to respiratory failure, and the commonest trigger is infection.
Other triggers
- Surgery
- Pain
- Drugs
- Hypothermia
- Hyperthermia
- Pregnancy
- Stress
- Sleep deprivation
- Residual neuromuscular blockade
In your patient, who is currently asleep and intubated, you'll only find out when you try and wake them up and find they're not taking very deep breaths or moving very much, despite full reversal with sugammadex.
- In an awake patient, a vital capacity of less than 20 - 25 ml/kg is suggestive of major weakness
If there's a tube in place, leave it there, if not, put one in.
- Talk to neurology pronto
- They're likely to need high dose steroids, IVIG or plasma exchange
"This doesn't look like just weakness"
The other possibility is throwing them to the other end of the spectrum and causing a cholinergic crisis, possibly because of too much neostigmine and not enough glycopyrrolate.
- Weakness
- Bradycardia
- Hypotension
- Bronchospasm
- Secretions
- Sweating
- Vomiting
- Diarrhoea
Give atropine up to 2mg to fix it.
What if they're pregnant?
You just know this is going to happen to you at three in the morning on a Sunday, so listen up.
- They should have had an MDT approach during their pregnancy, with a bespoke management plan for their labour and delivery
Should.
Fortunately for the anaesthetist most problems with MG are more common in the first trimester rather than the last few weeks.
General anaesthesia may be required for patients with severe respiratory or bulbar weakness, as they may not be able to tolerate thoracic blockade.
Around 30% of babies of mothers with MG will get a transient neonatal MG, so NICU needs to be aware and available.
What if they have pre-eclampsia as well?
- Blood pressure control with methyldopa or hydralazine
- Avoid beta blockers and calcium channel blockers if at all possible
- IV magnesium is very high risk - only give if seriously concerned about eclampsia
- Keppra or valproate can be used to prevent seizures if needed
Useful Tweets
Suspected Lambert Eaton Myasthenic syndrome patient with Initially absent knee jerk that is enhanced briefly by tapping the tendon repeatedly. pic.twitter.com/CKugLGWY47
— Neurophilia (@bobvarkey) March 25, 2023
Neuromuscular Junction and Key Elements for the Pathogenesis of Myasthenia Gravis. See the full Review Article: https://t.co/l9A7XNF8RP pic.twitter.com/SgsaRBVLbi
— NEJM (@NEJM) January 4, 2017
References and Further Reading


Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!

