Muscles

Take home messages
- The functional contractile unit of the muscle is the sarcomere
- Cardiac muscle is incapable of tetany
- Calcium binds troponin in skeletal and cardiac muscle, and calmodulin in smooth muscle
A strong contender for 'driest examinable material', muscle structure is one of those topics that you don't think all that much about until you're staring at a vignette outside your second OSCE station, at which point you start to wish you'd thought about it a little earlier.
Alongside electrical safety and equipment decontamination, it gets examined disproportionately frequently in the Primary FRCA.
You know, because your life isn't hard enough already.
First up, you need to know about the three distinct types of muscle tissue in the body.
- Skeletal
- Smooth
- Cardiac
And of course, what makes each one so special.
The vast majority of exam questions focus on skeletal muscle, because it tends to be most relevant to anaesthetic practice, when you think about neuromuscular blocking agents, muscular dystrophies etc. but you do need to be aware of how cardiac and smooth muscle differ.
Spot the difference
Mitochondria
- Skeletal muscle - very few
- Smooth muscle - very few
- Cardiac muscle - lots
Fibre structure
- Skeletal muscle - long cylinders, striations
- Smooth muscle - sheets
- Cardiac muscle - branched cylinders with gap junctions
Response type
- Skeletal muscle - all or nothing
- Smooth muscle - graded contractile response
- Cardiac muscle - all or nothing
Innervation
- Skeletal muscle - voluntary
- Smooth muscle - autonomic
- Cardiac muscle - autonomic
Pacemaker function
- Skeletal muscle - none
- Smooth muscle - slow
- Cardiac muscle - fast
Calcium binding site
- Skeletal muscle - troponin
- Smooth muscle - calmodulin
- Cardiac muscle - troponin
Capable of tetany?
- Skeletal muscle - yes
- Smooth muscle - yes
- Cardiac muscle - no
Skeletal muscle
Skeletal muscle is striated, meaning it has little stripes visible under the microscope, and looks like this:

The long pink tubes are myofibrils, which are organelles within the muscle cell that contain the contractile machinery necessary for muscles to do what they do.
The unimaginatively named sarcomere (sarx "flesh", meros "part") is everything between two Z lines, and represents the functional contractile unit of the myofibril.
Each sarcomere only contracts a miniscule distance, but by having thousands of them linked together, the myofibril is able to contract much further.
To start with you can immediately see there are some thicker filaments (green) and thinner ones (grey).
- Thick = myosin
- Thin = actin (plus tropomyosin and troponin, wrapped around and studded along it respectively)
You might get asked to label a diagram like the one below in your Primary SOE or OSCE, so you just need to learn three bands and two lines.
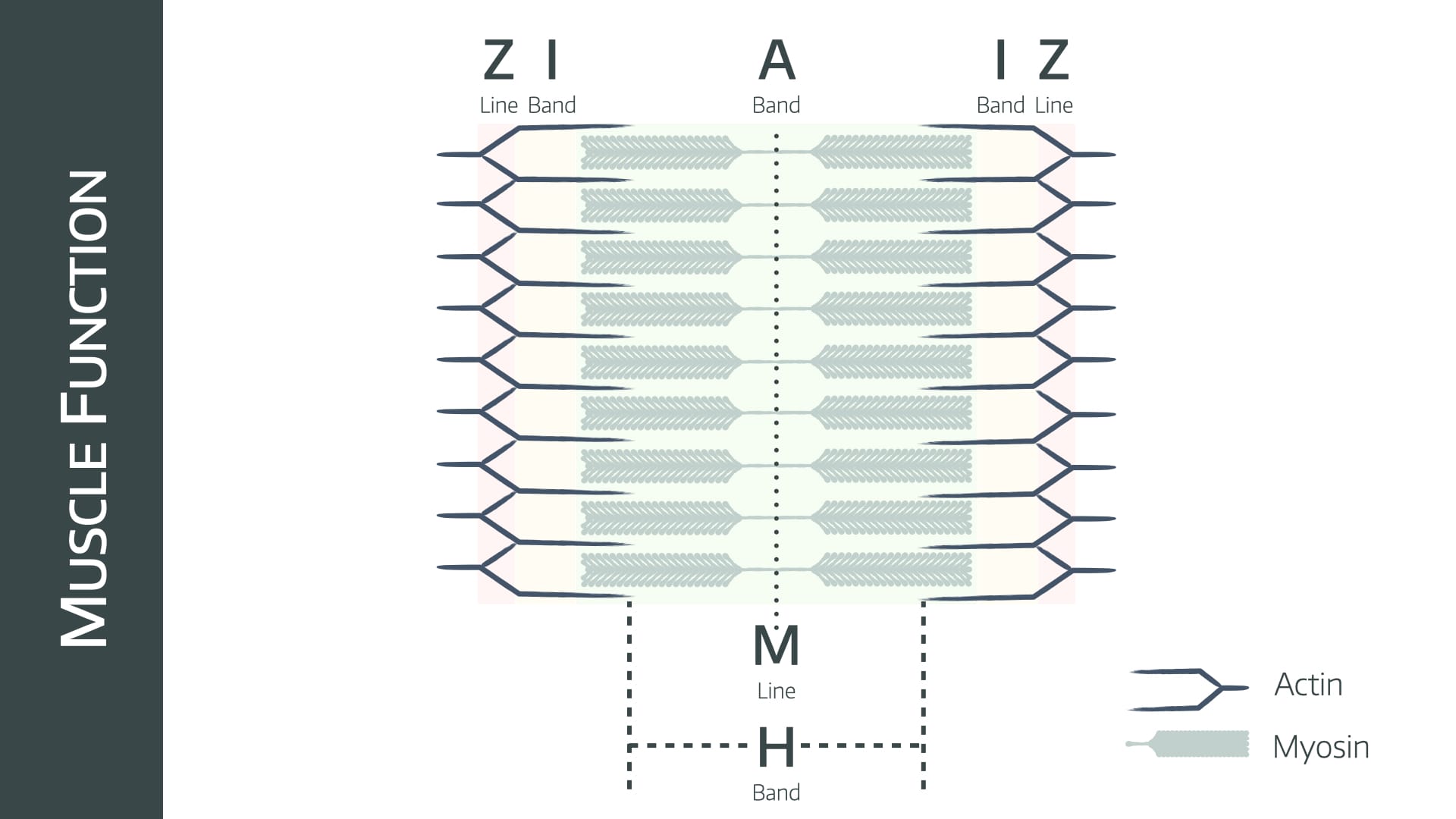
A band
- The length of the thick myosin filament
- A stands for anisotropic if you're interested
- Doesn't change length as muscle contracts
I band
- Isotropic band
- The area of actin filaments that are not overlapping with myosin
- Gets smaller as muscle contracts and Z lines move closer together
H band
- The area of myosin filaments that are not overlapping with actin
- Gets smaller as muscle contracts
Occasionally referred to as the H 'zone', which makes it precisely zero percent more interesting.
Z line
- The actin anchor points between the sarcomeres
M line
- The myosin junction at the middle of the sarcomere
- It has no cross-links between filaments
A quick break
This isn't muscle tissue contracting, but it's hella cute.

This is Kinesin, a vesicle-dragging motor protein, and definitely in the top ten rankings for happiest protein.
Just look at its SHOES.
Right back to work.
How does skeletal muscle contract?
Explain it to me like I'm 5
The myosin has sticky little oars that grab onto hooks on the actin threads, and pull them along like a rope, dragging the thick and thin filaments past one another, bringing the Z lines closer together.
Each oar, or head, then requires ATP to allow it to let go of the actin, swing back to its starting position, and do it all again.
To stop this happening accidentally, there's a safety cover over the hooks, called tropomyosin, and the button that you press to release the safety cover is called troponin.
Calcium pushes the button.
Now explain it to me like I'm taking the FRCA
Start with a summary statement to sound like you know exactly what you're talking about:
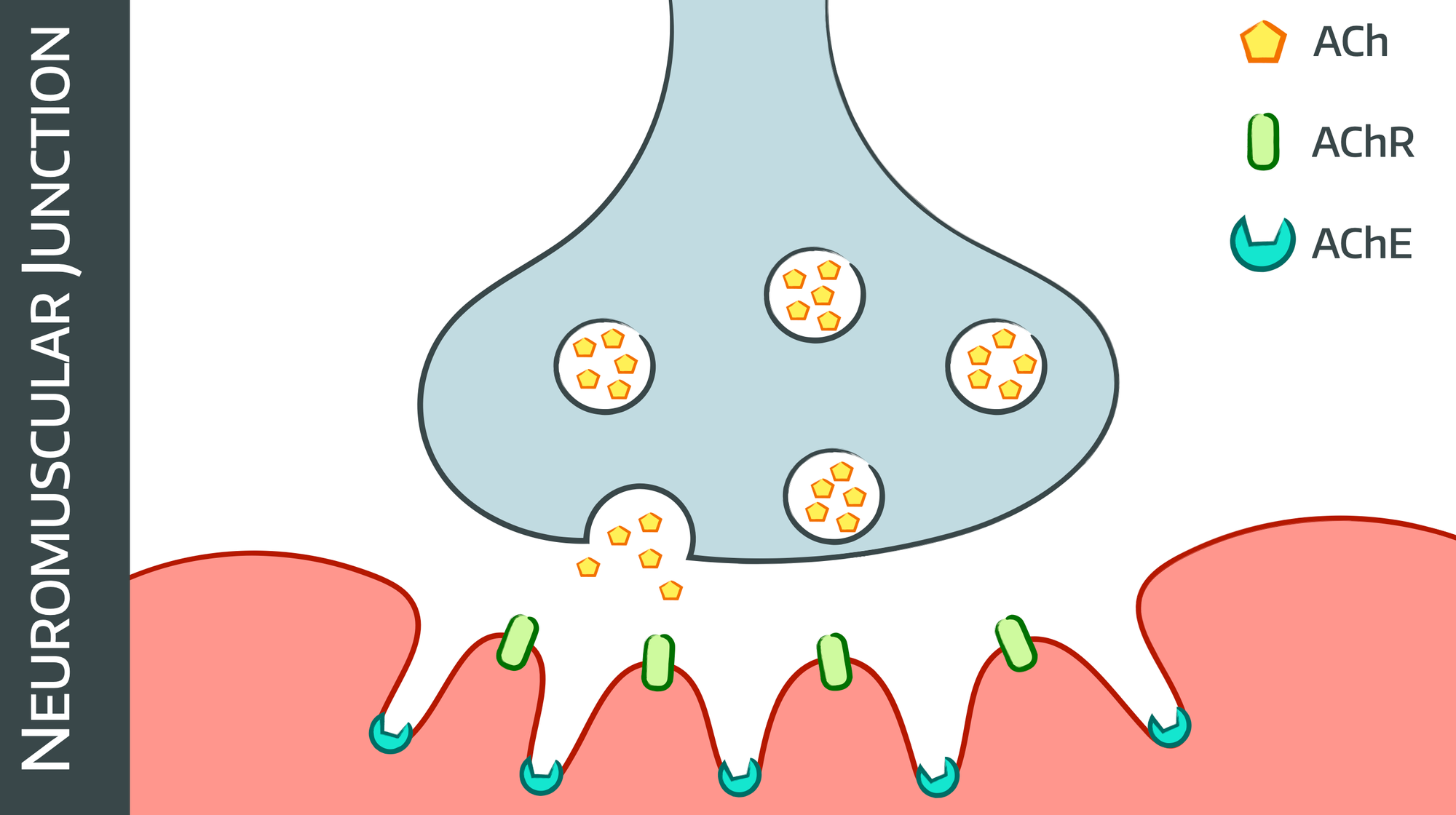
The first step is turning action potential into calcium release
- The action potential spreads across the post-synaptic membrane and down into the T-tubule system
- This induces a conformational change in the dihydropyridine (DHP) receptor
- The DHPr interacts with the ryanodine receptor on the sarcoplasmic reticulum, triggering calcium release
- This in turn causes calcium-induced calcium release to increase the concentration of intracellular calcium and therefore force of contraction
The second step is making myosin move
- At rest the myosin heads sit bound to ADP
- Calcium binds to the C subunit of troponin, next to the myosin binding sites on actin
- Troponin also has an I subunit (bound to actin) and T subunit (bound to tropomyosin)
- Calcium binding induces another conformational change in the troponin molecule, and the tropomyosin rotates, exposing myosin binding sites
- Myosin heads bind to actin on these sites, and this binding causes the myosin head release the ADP
- Releasing ADP induces a conformational change in the myosin head, making it pivot, pulling the actin and myosin past each other like little oars on a teeny tiny rowing boat (don't say teeny tiny rowing boat in the exam)
- This is called the power stroke, and represents around 10nm of movement
The third step is recharging the system
- ATP binds to the myosin, forcing it to release the actin binding site
- ATP is hydrolysed, which activates the myosin head for the next cycle
- The process can repeat, and contraction continues, as long as there is enough calcium to keep moving tropomyosin away from the actin binding sites
- Calcium levels then drop due to timed inactivation of calcium channels
- Sodium-Calcium exchange pump then moves calcium back into the sarcoplasmic reticulum and out of the cell
- The low calcium concentration causes tropomyosin to cover the actin binding sites
- Contraction stops
And repeat.
What are the types of contraction?
- Isotonic - muscle generates force against a constant load with a decrease in muscle length
- Isometric - muscle generates force against a load but doesn't change length
Isotonic contraction occurs in your arm muscles as you lift the tongue with the laryngoscope
Isometric contraction occurs as you hold the laryngoscope in place, desperately looking for some vocal cords
At this point a variety of unrelated sphincters may contract or relax at random.
What about smooth muscle?
- The whole contraction mechanism is essentially the same
- Calcium binds calmodulin instead of troponin, but it does the same job
- Instead of tightly arranged myofibrils, you have a sheet of muscle cells that generally contract together
- Not under voluntary control, mostly autonomically innervated
That's pretty much all you need to pass the Primary OSCE station.
Check out this awesome infographic by Eleanor Lutz over at Tabletop Whale
Other stuff they might ask you
What happens in muscular dystrophy?
- Dystrophin is a scaffold protein that connects the myofibrils to the membrane of the sarcolemma, giving muscles their shape and structural integrity
- Duchenne muscular dystrophy is caused by absence of dystrophin
- Becker muscular dystrophy is an X-linked recessive mutation of the very large dystrophin gene
Explain the monosynaptic reflex
This is a stretch reflex for maintaining posture
- Muscle spindle detects stretch and fires via the afferent nerve
- Travels to the dorsal root and synapses in the anterior horn
- Synapses directly with efferent motor neurone, and with interneurons
- Efferent motor neurone triggers contraction of the stretched muscle
- Interneurons inhibit the antagonistic group of muscles, to facilitate more efficient contraction
- This is called reciprocal innervation
How does malignant hyperthermia happen?
- Ryanodine receptors RYR1 coordinate calcium release from the sarcolemma
- Defective receptors exposed to a triggering agent result in uncontrolled calcium release and muscle contraction
- This leads to excessive oxygen consumption and production of heat and carbon dioxide
- Excessive muscle contraction leads to a dramatic rise in serum potassium level because the intracellular potassium concentration is around 155mmol per litre, and if there is excessive muscle cell damage this leaks out into the circulation.
- Triggering agents include volatile anaesthetic agents and suxamethonium

Syllabus
- PB_BK_29 Action potential generation and its transmission
- PB_BK_30 Neuromuscular junction and transmission, motor end-plate
- PB_BK_33 Muscle contracture – malignant hyperthermia, myoclonus, burns
- PB_BK_34 Muscle types; skeletal, smooth, cardiac
- PB_BK_35 Skeletal muscle excitation-contraction coupling
- PB_BK_36 Smooth muscle contraction: sphincters
- PB_BK_37 Motor unit concept
- PB_BK_71 Autonomic nervous system; organization, ganglia, adrenergic vs cholinergic
- PB_BK_72 Neurological reflexes: monosynaptic, polysynaptic, stretch, inhibition
- PB_BK_73 Motor function: basal ganglia, spinal and peripheral
Useful Tweets and Resources
Here’s a rare & unique perspective on what’s happening inside a sarcomere (muscle tissue): myosin heads (pink) bind to actin filaments (blue), and pull them towards the center of the sarcomere to contract the muscle 💪#sciart #kinesiology #medicalanimation pic.twitter.com/YhrAgxg2F7
— AXS Studio (@axs_studio) October 22, 2020
References and Further Reading

Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.

