Muscle Relaxants
Take home messages
- If in doubt, rocuronium is rarely a bad idea
- Avoid suxamethonium in malignant hyperthermia, burns and spinal cord injury (conditions apply)
- Make sure your patient is adequately anaesthetised
Why paralyse a patient?
It sounds terrifying, and we'd strongly advise not using the word 'paralyse' around your patient, but we frequently inject patients with medications that stop them moving and breathing on purpose.
Use something like 'relaxant' instead - it sounds much more appealing.
The ability to reversibly prevent a patient from moving their skeletal muscles is enormously helpful in anaesthesia, primarily for three reasons:
- To facilitate intubation by relaxing the muscles of the pharynx and vocal cords
- To provide an optimal environment for the surgeon by ensuring the patient stays completely still
- To allow better control of the patient's ventilation by preventing respiratory effort, coughing and hiccups
Just remember that they will also stop breathing, so you'll need to have some sort of plan for their airway and ventilation in place first.
The most important thing to remember about these drugs is that they only provide muscle relaxation, and neither of the other two vital components of a satisfactory anaesthetic:
- They provide no anaesthesia, so the patient will be fully conscious
- They provide no analgesia, so the patient will feel everything
If that sounds terrifying, that's because it is - these are enourmously powerful and highly dangerous drugs that need to be used appropriately with the respect and caution they deserve.
What are the types of muscle relaxants?
- Depolarising - (suxamethonium)
- Non-depolarising*
*These are either aminosteroids such as rocuronium and vecuronium, or benzylisoquinoliniums such as atracurium.
Benzylisoquinolinium is worth 45 points in scrabble.
Or it would be if a scrabble board had more than 15 squares in a row.
A bit of history
Don't confuse the noun Curare with the Latin verb 'curare' meaning to heal or cure
Curare doesn't cure very much at all, because it's a paralysing plant toxin.
- For a long time (i.e. prior to the 1500s) curare was used to poison darts for hunting in the Caribbean and South America
- 1825, Charles Waterton kept a curarised female donkey alive by ventilating it with bellows through a tracheostomy, proving that it was asphyxiation, and not the drug itself, that killed the victim
- 1942 Griffith and Johnson had the bright idea that d-tubocurarine (dTC) could be used to provide muscle relaxation for surgery
To be fair to them it worked, but a fair number of patients died because they obviously stopped breathing and the severity of this problem probably wasn't given the due attention it deserved.
Oh, and a bunch of them were totally awake for the whole surgery.
- 1952 along comes succinylcholine or suxamethonium, courtesy of Thesleff and Foldes (et al.) and proves to be a game changer for tracheal intubation
- Gallamine, d-methyltubocurarine and alcuronium are then introduced over the next ten years or so, but don't add a whole lot of advantage
- 1967 pancuronium is found to have a similar (enormous) duration of action to dTC, however was much more cardiostable and released far less histamine
- Atracurium and vecuronium hit the stage in the early 1980s and added the benefit of faster onset, quicker recovery and reduced the reliance on adequate kidney function for clearance
- Vecuronium's legendary cardiostability became the new benchmark against which other agents were measured
- Meanwhile atracurium shone for being completely organ-independent for its metabolism
- In the 1990s along come mivacurium and rocuronium to steal the show with reliable rapid onset and offset
- 1995 cisatracurium is approved for human use, with greater potency and reduced histamine release compared to atracurium
Nowadays most people use rocuronium for most things, but everyone has their preferences.
Depolarising Agents
Non Depolarising Agents
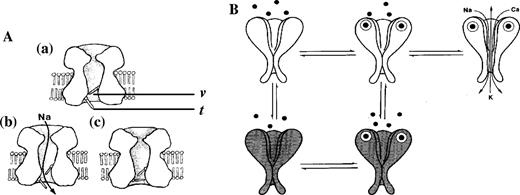
Non-depolarising neuromuscular blocking drugs are competitive antagonists at nicotinic acetylcholine receptors.
There are 2 classes of NMBDs:
- Aminosteroids
- Benzylisoquinoliniums
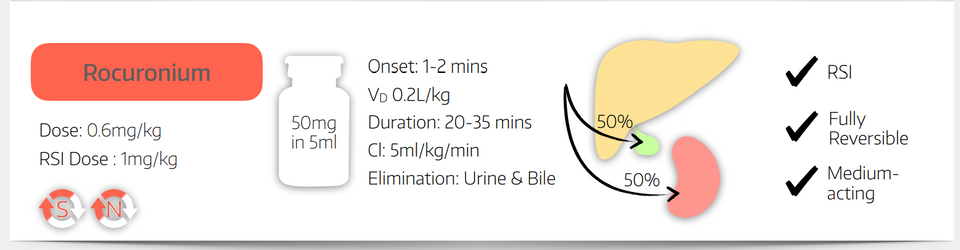
You’ll likely use Rocuronium most often in your practice, which is an Aminosteroid, so we’ll look at those first.
Aminosteroids
Benzylisoquinoliniums
- Cisatracurium is a bisbenzyltetrahydroisoquinolinium if you're interested
- Bisbenzyltetrahydroisoquinolinium is worth 67 points in scrabble
How can we measure muscle relaxation?
It's useful to know approximately how paralysed a patient is during surgery, firstly to know that they're not going to move at the crucially important points during the operation, but also to know that when the time comes to wake them up and extubate them, they're going to be able to breathe and move on their own.
You can do this clinically, by seeing how effective their breathing is on the monitor, and asking them to lift and hold their head off the pillow, but these methods are unreliable and can miss rather significant residual weakness.
To assess the degree of neuromuscular blockade more scientifically, we use a nerve stimulator, which fires a small electrical impulse through the skin to cause depolarisation of the motor neurone and therefore elicit a muscle twitch.

Note that the positioning of our electrodes is important, because we want to stimulate the nerve and not the muscle directly.
What modes of stimulation can be used by a nerve stimulator?
This is a classic OSCE question, and unfortunately for the exam they do expect you to know the frequency and amplitude of the impulses delivered by the nerve stimulator.
Aside from being able to deliver a single impulse and muscle twitch, there are four main modes on a nerve stimulator:
Train of Four
- This mode delivers four supramaximal stimuli (around 80mA) at a frequency of 2 Hz (one every 0.5 seconds)
- Depolarising muscle relaxants will produce four equally reduced or absent twitches, depending on the level of blockade
- Non-depolarising muscle relaxants will cause fade (gradually decreasing twitch amplitude)
How many twitches you can see correlates with the amount of blockade:
- 0 twitches = >95% of receptors blocked
- 1 twitch = >90%
- 2 twitches = >80%
- 3 twitches = >70%
- 4 twitches = <70%
Note that a patient with four strong muscle twitches can still have up to 65-70% of their acetylcholine receptors blocked, so four twitches doesn't necessarily mean they're not going to have weakness or difficulty breathing in recovery - if in any doubt, give some reversal agent
Train of Four Ratio
- This modality provides the same four stimuli as TOF
- However the amplitude of the last (4th) twitch is then compared to that of the first
- A ratio of >0.9 is advised before attempting extubation
Double Burst Stimulation (DBS)
- This mode delivers three shocks at 50 Hz followed by another identical three shocks 750ms later
- This is a slightly more crude method of measuring blockade, but it makes assessment of fade easier than TOF
Post Tetanic Count (PTC)
- This mode delivers a tetanic stimulus of 50Hz for five seconds, then waits three seconds before delivering pulses at 1 Hz, or every second
- The tetanic stimulus floods the neuromuscular junction with acetylcholine, temporarily overpowering the neuromuscular blockade
- The number of twitches seen is then inversely proportional to the degree of blockade
- As a rough guide, a post tetanic count of 4 suggests approximately five minutes before there will be one twitch visible on train of four
Caution - do not repeat this within five minutes as it can give false positives and potentially damage the muscle tissue
Reversal Agents
There are two reversal agents available for non-depolarising neuromuscular blocking agents - sugammadex and neostigmine
- Note that you can only use neostigmine if there are already two twitches visible on train of four
- Remember that it takes up to 10 minutes to work
Syllabus
- PC_BK_84 Assessment of neuromuscular blockade
- PR_BK_12 Anticholinesterases: Classification of drugs that inhibit acetylcholinesterase and plasma cholinesterase including organophosphates
- PR_BK_36 Muscle relaxants. Classification. Sites of action. Properties of an ideal muscle relaxant. Dantrolene and management of MH
- PR_BK_37 Depolarizing muscle relaxants: Structure, mechanism of action. Organophosphate poisoning. Adverse effects and contraindications
- PR_BK_38 Non-depolarizing muscle relaxants: Structural classification; sub-classification according to onset-time and duration of action. General comparison of aminosteroids and bisbenzyisoquinoliniums. Comparison of individual agents; metabolism and active metabolites. Unwanted effects.
- PR_BK_39 Reversal of neuromuscular blockade: Indications for use; mechanisms of action; clinically unwanted effects of reversal of neuromuscular blockade
Download our free summary here
Useful Tweets and Resources
One of the scariest moments of my career was in 2021 when a patient of mine had anaphylaxis to rocuronium - a neuromuscular blocker. Anything that will make these reactions rarer is great.
— Dr Helgi (@doctorhelgi) March 14, 2023
Cough medicines containing pholcodine withdrawn over safety fears https://t.co/AL5JHG7aIa
140kg bearded quad biker, ‘clothesline injury’ to neck from wire fence, GCS 3, subcut emphysema and crepitus to anterior neck, diaphragmatic breathing, priapism, BO 85/50, history of porphyria and consequent ‘problems with anaesthetics’
— Cliff Reid (@cliffreid) October 24, 2022
@Buzzmf87 pic.twitter.com/dUS3YEIUw4
References and Further Reading

Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
