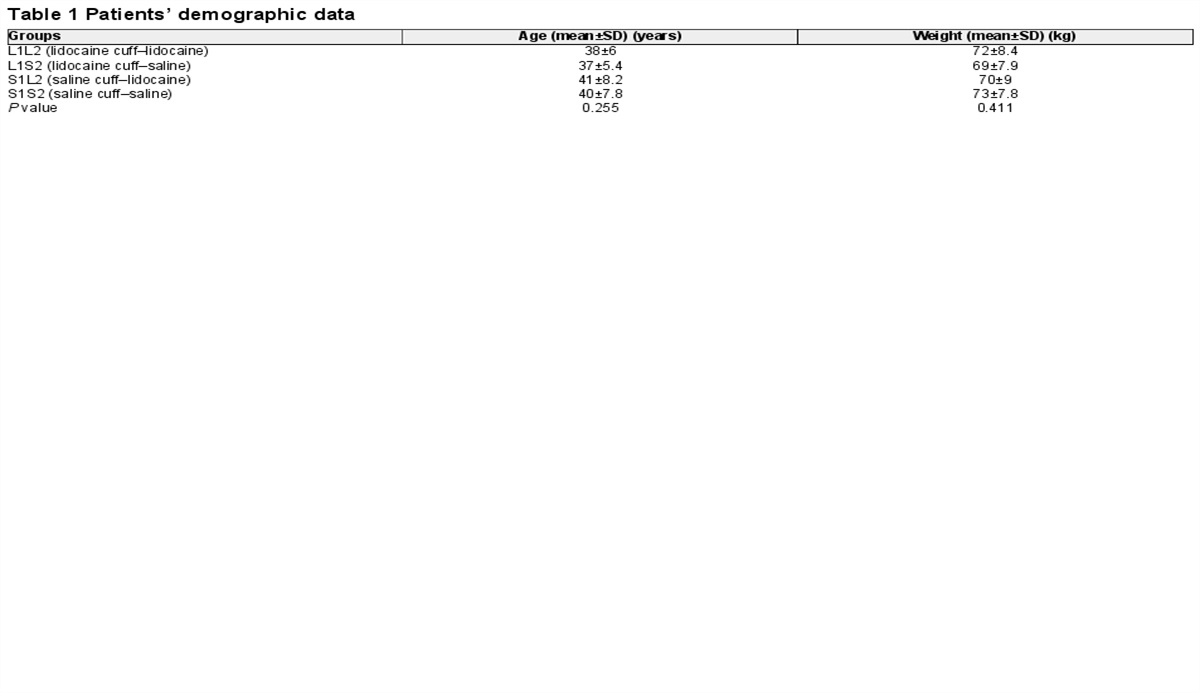
Intracuff lidocaine

I highly doubt this will constitute examinable material, however it is interesting, and after all - that's why we're here.
The take home messages
- You can put lidocaine in the ET tube cuff
- It will probably help a little to prevent coughing on emergence and sore throat after the operation
- Very few people do it
- Pointless if the procedure is less than 30 mins
How it works
Not especially complicated - you shove a load of local anaesthetic into the cuff, and it diffuses through the membrane of the cuff itself and into the tracheal mucosa, providing gentle topical anaesthesia to the areas in physical contact with the tube.
Invented in 1943 by Swedish chemist Nils Löfgren, lidocaine was the first amide local anaesthetic agent to hit the market, massively outperforming the main contender at the time procaine in terms of:
- Speed of onset
- Duration of action
- Risk of allergic reaction
- Stability in solution
And once PVC cuffs became more common on endotracheal tubes from the 1990s onwards, this new off-label route of administration started to come into fashion.
Advantages of intracuff lidocaine
- Easy
- Safe
- Reduces coughing
- Reduces sore throat
- Seems to reduce the incidence of laryngospasm
- May also improve haemodynamic response to extubation
Disadvantages
- You're overcomplicating a procedure that doesn't necessarily require overcomplication
- Many ODPs will look at you funny
- Theoretical risk of cuff rupture as liquid not compressible like air
Some physics and pharmacokinetics
- Minimal systemic absorption (safe dose 9mg/kg but you won't get anywhere near this)
- Takes around 15-30 minutes to diffuse through to the tracheal mucosa
- Alkalinised lidocaine lasts longer and works faster
Most modern endotracheal tubes have some form of polyvinyl chloride cuff, which fat soluble drugs can diffuse through passively without too much encouragement.
If you add bicarbonate to your lidocaine, you play with the pKa and keep more of the lidocaine molecules in their unionised state, allowing them to diffuse across the cuff, much like any other lipid membrane in the body.
The recipe
- 4% lidocaine with 8.4% bicarbonate appears to be the standard approach
- Mix 2 mL 8.4% NaHCO₃ with 8 mL 4% lidocaine to make 10 mL of alkalinised solution
- But you can also use 2%, 10%, non-alkalinised, anything by the sounds of it
- Cuff needs to be entirely filled with liquid, air will make absorption slow and patchy
Evidence
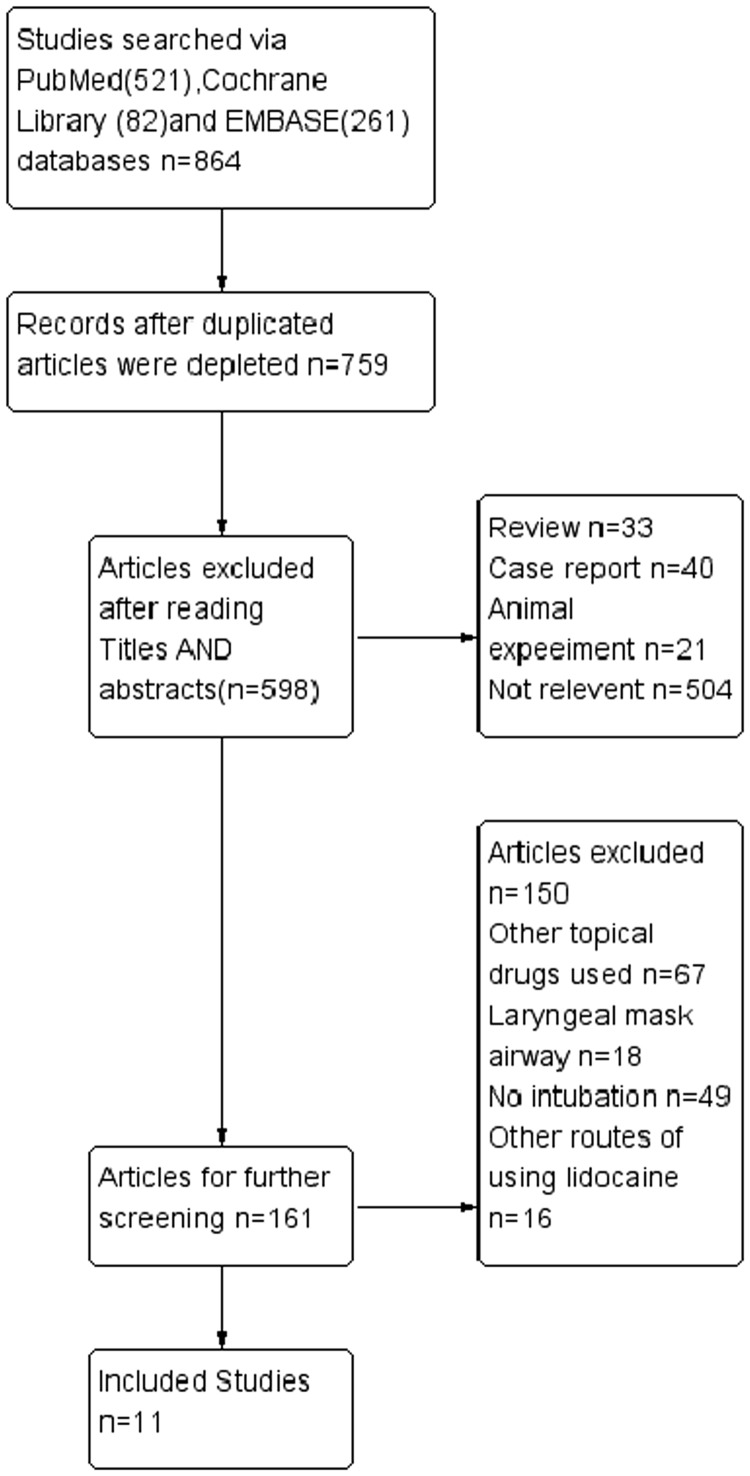
The results of this meta-analysis of 11 RCTs involving 843 patients showed that the administration of alkalinized or non-alkalinized lidocaine to endotracheal tube cuffs significantly reduced coughing on tube and other intubation-related complications (i.e., hoarseness, agitation/restlessness and/or dysphonia) during the extubation process. In addition, by comparison with controls, intracuff administration of alkalinized lidocaine tended to be more effective than non-alkalinized lidocaine. Importantly, the outcome was similar when studies with high risk patients (i.e., children, smokers and those with hyperactive airways)21,23,24 were excluded from the analysis. However, according to GRADE recommendations the studies were classed as ‘low level of evidence quality’ and results from a funnel plot indicated potential publication bias.

Remind me what I need to know about lidocaine for the FRCA?
Class and Structure
- Amide local anaesthetic (two i's in the name = amide, one i = ester)
- Aromatic ring joined to an amine via an amide linkage
- Also a Vaughn-Williams Class 1B antiarrhythmic agent
- Shortens action potential duration
- Used IV for refractory VT
Mechanism of action
- Blocks voltage-gated sodium channels
- In a use-dependent fashion
- from the intracellular side of the channel (needs to get into the cell first)
- Prevents neural depolarisation and transmission of afferent pain signals
Doses
- 3mg/kg when infiltrating alone
- 7mg/kg if using subcutaneously with adrenaline
- 9mg/kg if applying topically to airway mucosa
Onset and duration
- Rapid onset
- Intermediate duration
- pKa = 7.9 (around 25% unionised in the body)
- 65% protein bound to alpha-1-acid glycoprotein
Metabolism
- Hepatic - CYP1A2 and CYP3A4
- Renal excretion
Presentation
- Clear colourless solution for injection - 1%, 2% and 4%
- Transdermal patch - 5%
- Gel or spray - 4% and 10%
Avoid spinal use as high risk of transient neurological symptoms
Here are our posts on local anaesthetics
Useful Tweets and Resources
Intracuff lidocaine
— SIVA Trainees (@SIVATrainees) November 28, 2024
'If they recognise their name their brain stem is functioning'#SIVA24 pic.twitter.com/u7Q91QUhlc