Intra-Aortic Balloon Pump

Take home messages
- Don't switch it off
- The goal is to improve blood supply to the myocardium, while also reducing its oxygen demand
- Patients need to be anticoagulated
- Check renal function to ensure the renal arteries are not occluded
- Balloon pumps cause haemolysis
- If the timing isn't right, then the patient can become very unstable
Podcast episode
What is it?
What, the intra-aortic balloon pump? Well it's a balloon, and it sits...
Because clearly the logical next step when you've got a clapped out cardiovascular patient is to plumb a balloon into the biggest artery in their body and do the Hokey Cokey with a bunch of helium right?
Well read on, because there is some method in the madness.
What is counterpulsation?
The idea is volume displacement of arterial blood, to help the heart send it to the two places where it needs to be:
- The coronary arteries
- The rest of the systolic circulation
So the balloon sits in the descending aorta, inflates during diastole, and then deflates again during systole.
All very quickly, in time with the ECG (or arterial pressure trace).
Theoretically this means that systolic blood flow to the body is unimpeded, but as soon as the heart relaxes, the balloon inflates and displaces the blood in the aorta both forwards and backwards, encouraging the blood to flow down the coronary arteries, as well as giving it an extra little shove to the rest of the body.
What are the benefits of counterpulsation?
- The balloon inflates in diastole, pushing blood into the systemic circulation and back down the coronary arteries, improving coronary blood flow
- The balloon deflates just before systole, decreasing aortic pressure and reducing afterload
Then when the balloon deflates again immediately prior to systole, it causes a slight negative pressure in the aorta, reducing afterload on the left ventricle by reducing the pressure gradient across the aortic valve.
What is the Windkessel effect?
- The 'Windkessel Effect' refers to the elastic recoil of the aortic root, generating pressure to squeeze blood down the coronary arteries in diastole. The balloon aims to supplement this.
Effects on the heart
- Reduces systolic pressure and increases diastolic pressure in the aorta
- Reduces end-diastolic pressure and afterload on the left ventricle
- Increases cardiac output and hopefully coronary blood flow
What factors affect how well the balloon works?
- The volume of the balloon - determines how much blood is displaced
- Aortic compliance - a more compliant aorta will distend, reducing the backpressure and producing less augmentation
- Heart rate - a shorter diastole means less balloon time and less augmentation
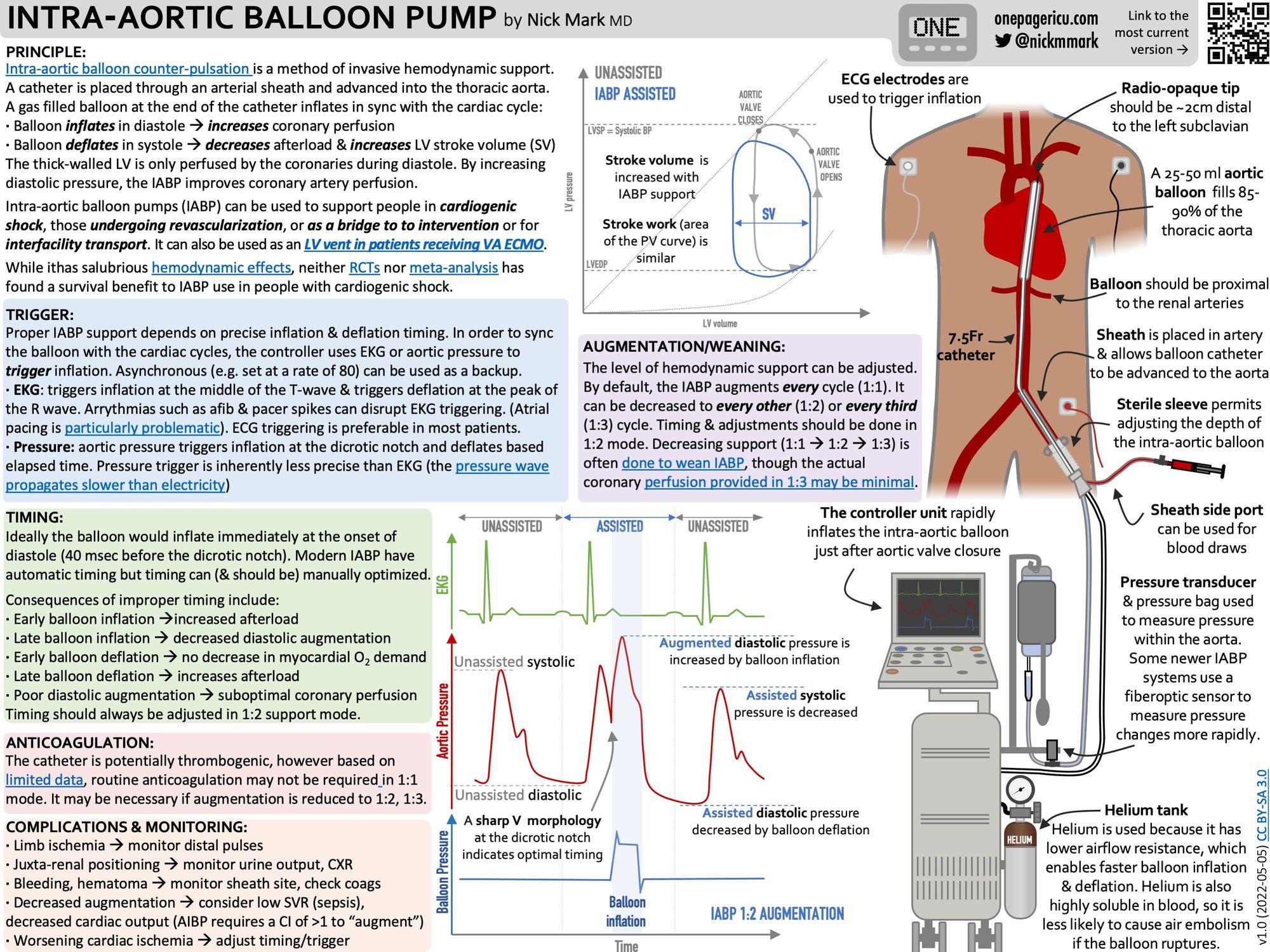
The Timing Sequence and Arterial Waveform
You need to be able to draw and explain this bit.
We've borrowed the following image from the amazing Deranged Physiology website, because it explains it perfectly.
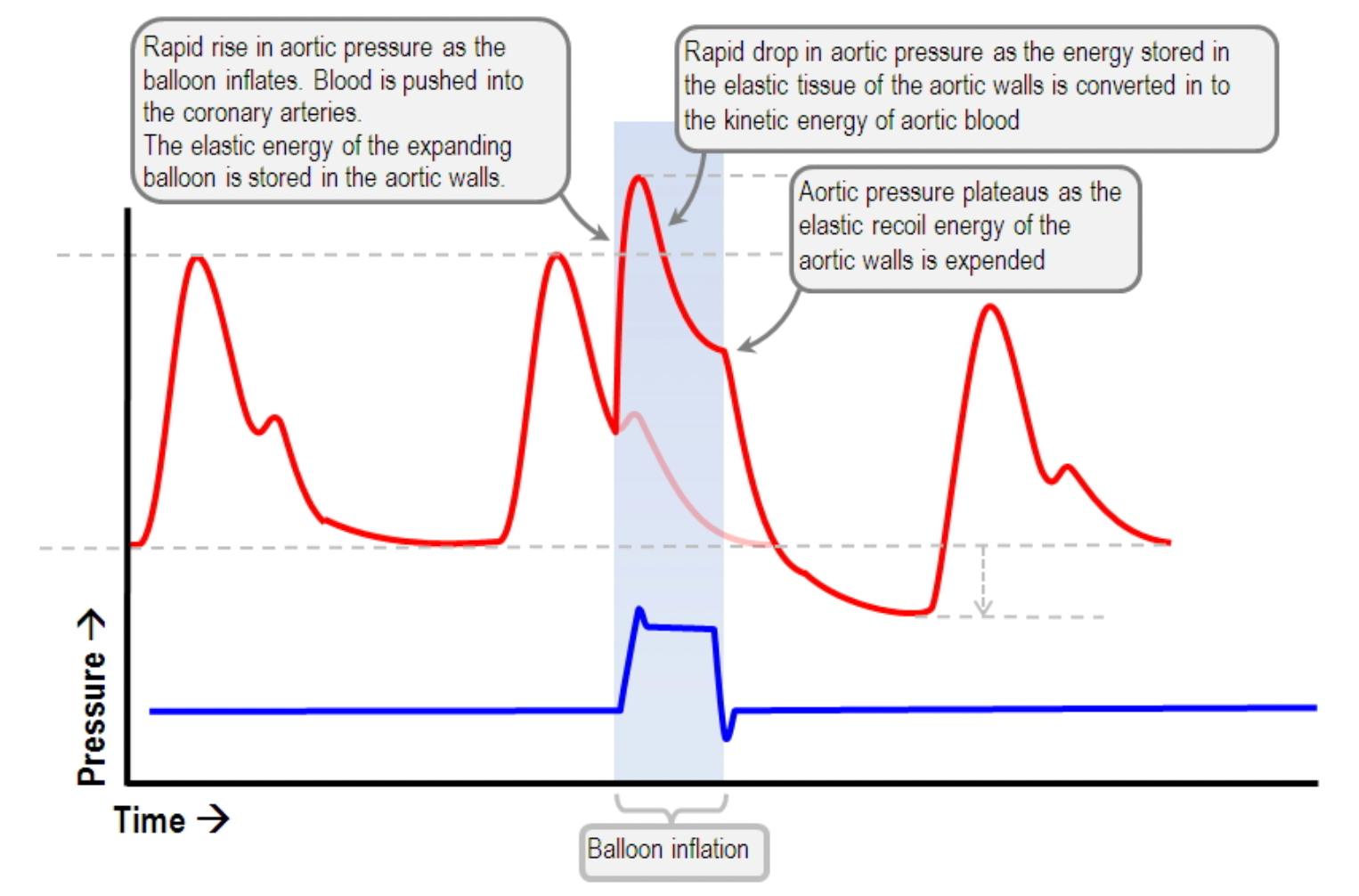
The dicrotic notch on the arterial waveform occurs when the aortic valve closes. The balloon inflates immediately after this, and then deflates again just before the valve opens in systole. This point is the lowest point of the arterial pressure waveform.
When the balloon inflates, it obstructs arterial blood flow, causing a rapid drop in blood pressure at the point of the dicrotic notch. However by increasing or augmenting diastolic pressure, it produces a large second peak, which is unsurprisingly labelled 'diastolic augmentation'.
Hopefully the diastolic augmentation will be higher than the systolic pressure.
You can then set the pump to assist every beat, every alternate beat, or any ratio that is required. As the patient's cardiovascular status improves, the support can be weaned off with less and less augmentation. It should never, however, be left deflated, as it is a huge thrombosis risk.
Indications and Contraindications for IABP
Indications:
- Acute Myocardial Infarction
- Refractory left ventricular failure
- Cardiogenic shock not responding to pharmacological therapy
- Sepsis
- Cardiac surgery and weaning from cardiac bypass
- Acute MR and VSD
- Infant with cardiac abnormalities
- Refractory unstable angina
Absolute contraindications:
- Aortic dissection
- Aortic regurgitation
- Previous Aortic stenting
- Chronic end stage heart failure deemed inoperable
Relative contraindications:
- Severe uncontrolled sepsis
- Severe peripheral vascular disease
- Abdominal aortic aneurysm
- Anatomical abnormalities or previous arterial reconstructive surgery
- Tachyarrhythmias
The Balloon
The intra aortic balloon pump is divided in to two parts - the balloon itself and the control pump.
The polyethylene balloon is usually between 25 and 50ml and is loaded onto a double-lumen 8 - 9.5 Fr catheter.
The control pump coordinates the timing of inflation and deflation, and often uses helium for two reasons:
- Its very low density makes it ideal for rapid inflation and deflation
- It's very rapidly absorbed by the blood, which is helpful if the balloon ruptures
Complications
As you might imagine, inserting a large catheter into the aorta of a patient with heart problems, and then attempting to inflate and deflate a balloon to occlude the aorta in time with the heartbeat, can sometimes go wrong.
- Balloon rupture and gas embolus
- Haemolysis and thrombocytopenia
- Occlusion of cerebral or renal arterial supply
- Limb ischaemia
- Aortic trauma or dissection
- Bleeding and infection
- Tamponade
- Thromboembolism
- Compartment syndrome
- Balloon entrapment
What is the equation for coronary perfusion pressure?
- Coronary perfusion pressure (CPP) = ADP - LVEDP
- ADP = Aortic diastolic pressure
- LVEDP = Left ventricular end diastolic pressure
Our favourite YouTube video
Check out this amazing infographic from Dr Mark
I asked ChatGPT to write a poem about the complications of IABP.

Useful Tweets and Resources:
Here’s a fun ICU puzzle: what is causing this crazy spiking pattern on the ECG waveform of both an intra-aortic balloon pump & ICU monitor?
— Nick Mark MD (@nickmmark) November 19, 2022
A #MedEd 🧵 on an important clinical artifact & the triboelectric effect that we’ll need to go back in time 2500 years to understand!
1/ pic.twitter.com/1y5ltyBiz8
Today's pair of ICU #OnePagers are two widely used #cardiac support devices: the intra-aortic balloon pump (IABP) & the external cardiac pacer.
— ICU OnePager (@OnePagerICU) May 17, 2022
These OnePagers explain how these machines work, what all the settings mean, & how to adjust them.#FOAMed #FOAMcc pic.twitter.com/fdqyn3Gkkn
Normal #anatomy of the heart and major thoracic vessels with correct positioning of various lines.
— NephroPOCUS (@NephroP) February 1, 2023
(IABP = intra-aortic balloon pump)
Courtesy: https://t.co/Uuj8ztaurO#MedEd #xray #radiology pic.twitter.com/4lrDrm0iqv
References and Further Reading:




