Inhalational Anaesthetic Agents

Take home messages
- Oil:Gas Partition Coefficient and Minimum Alveolar Concentration relate to potency
- Blood:Gas partition Coefficient relates to speed of onset and offset
- MAC is affected by other drugs, patient factors and concurrent illness
What is MAC?
The minimum alveolar concentration for a given anaesthetic agent, is the minimum concentration required, at 1 atmosphere of pressure, to prevent a skeletal muscle response to a standard surgical incision in 50% of patients.
What. Why only half of people...?
I'll explain.
Imagine you're asleep, and someone touches your nose with a feather for some reason. You're likely to move your arm and swat it away before returning to your undisturbed sleep. You didn't wake up, and you weren't aware of the encounter, but you moved in response to a physical stimulus.
Now imagine how sleepy you would have to be to not even flinch in response to someone inserting a scalpel into your abdominal wall.
Rather sleepy.
So rest assured that even if a patient flinches slightly to a very painful stimulus, it doesn't mean they're aware of it or even particularly bothered by it.
MAC assumes you're only using the inhaled agent.
This doesn't even begin to take into account any other pain relief or sedation like intravenous opioids, regional anaesthesia or analgesic adjuncts that you're probably using while you anaesthetise your patient.
Just remember it also doesn't take into account any muscle relaxants either.
What are the different levels of MAC?
MAC-amnesia
- This is the level of anaesthesia needed to prevent explicit memory of a noxious stimulus
- Thought to be due to volatile agent action on the amygdala and hippocampus
- Occurs at approximately 0.25 MAC50
- For sevoflurane this would be an end-tidal sevoflurane partial pressure of approximately 0.4 kPa (which is essentially 0.4% concentration)
MAC-unconscious
- Occurs at approximately 0.5 MAC50 (0.8 kPa for sevoflurane)
MAC50
- This is the standard definition of MAC - the amount required for half of people to not flinch in response to incision
MAC-bar
- Blockade of autonomic response, so no tachycardia, pupil dilatation or hypertension is seen in response to a painful stimulus
- Thought to occur around 1.5 MAC50
MAC-intubation or MACEI
- This is more frequently used in children, when it is relatively common to intubate a child using only inhalational anaesthesia, without muscle relaxants or opioids
- For children this occurs at approximately 1.3 MAC50
- For adults it would be approximately 3 MAC50, which is enormous, and would likely result in cardiovascular instability
- This is one of the reasons muscle relaxants are employed to facilitate intubation in adults
What are Guedel’s Stages of Anaesthesia?
In 1917 Arthur Guedel devised a chart designed to teach nurses and orderlies how to monitor depth of anaesthesia, so that they could administer anaesthesia to wounded soldiers safely, without him having to be there all the time for every case.
His chart described four stages:
Stage 1
- From induction of general anesthesia to loss of consciousness
- Analgesia and amnesia but conversational
Stage 2
- Excitement or Delirium
- Disinhibition and uncontrolled movements
- Loss of eyelash reflex (at the lower end of stage 2)
- Hypertension and tachycardia
- Airway reflexes intact and often hypersensitive to stimulation - avoid manipulation
- There is a higher risk of laryngospasm
- Risk of vomiting and irregular respiration
Stage 3
- Surgical Anesthesia
- No eye movement and respiratory depression
- Airway manipulation is now safe
Stage 3 is then subdivided into four planes
Plane 1
- Regular, spontaneous breathing, central gaze and constricted pupils
- Eyelid, conjunctival and swallow reflexes disappear
Plane 2
- Pauses in breathing, increased lacrimation
- Loss of corneal and laryngeal reflexes, reduced ocular movements
Plane 3
- True surgical anaesthesia, with complete relaxation of intercostal and abdominal muscles
- Loss of pupillary light reflex
Plane 4
- Irregular respiration, full diaphragm paralysis, apnoea
Stage 4
- Progressing from apnoea to death
Best avoided.
It is important to remember that Guedel was using ether, a splendidly explosive analgesic vapour that took ages to take effect and caused all manner of laryngospasm and breath-holding along the way.
Things have changed a little since then.
However many of the same principles apply - you want your patient just the right amount of sleepy.
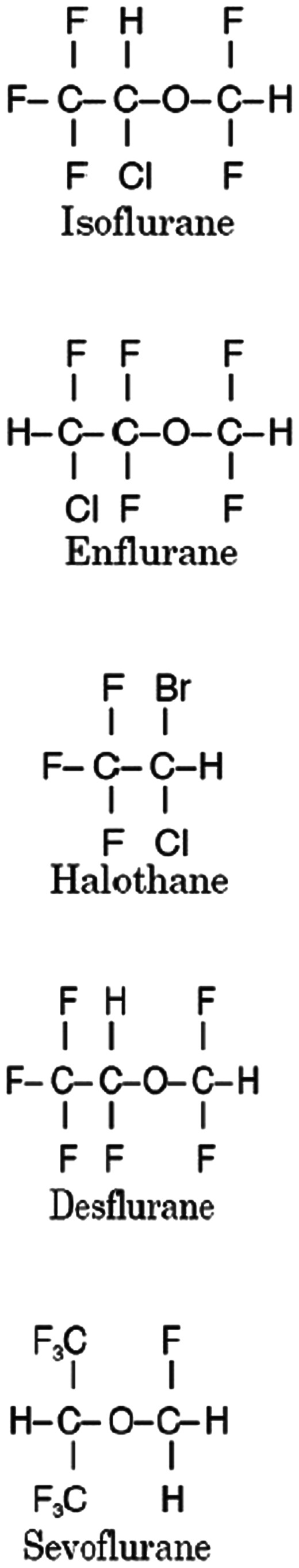
Isoflurane
Tell me about Isoflurane
Class and uses
- Halogenated ethyl-methyl-ether
- Used for maintenance of general anaesthesia
- Pungent smell makes it impractical for gas induction
Effects and side effects
Cardiovascular
- Reduction in systemic vascular resistance and blood pressure, with reflex tachycardia
- Coronary steal phenomenon has previously been suggested but evidence suggests not a clinically significant issue if coronary perfusion is adequately maintained
Respiratory
- Dose dependent reduction in minute ventilation
- Can cause breath holding and laryngospasm if used for gas induction
Neurological
- Reduced CMRO2
- Stable cerebral blood flow with maintained autoregulation up to 1 MAC
Other
- Can react with dry soda or baralyme to produce carbon monoxode
Metabolism
- Almost entirely excreted unchanged by the lungs
- 0.2% metabolised by the liver CYP2E1
Sevoflurane
Tell me about Sevoflurane
Class and uses
- Polyfluorinated ether
- Used for induction and maintenance of general anaesthesia
- Sweet odour
- Stored in polyethylene napthalate bottles because glass is a source of Lewis acids which can cause sevoflurane to break down to form hydrofluoric acid
Effects
Cardiovascular
- Reduction of SVR, often without compensatory tachycardia, causing a drop in blood pressure
Respiratory
- Dose dependent reduction in minute ventilation and subsequent increase in PaCO2
- Some bronchodilatation
Neurological
- Hypnosis
- Reduced CMRO2
Metabolism
- 2% of sevoflurane metabolised by hepatic CYP2E1
Desflurane
Tell me about Desflurane
- Needs its own vaporiser as boiling point of 23.5°C makes it too volatile for normal variable bypass vaporisers
- Hence it has its own TEC6 vaporiser that heats it to 39°C and 2atm of pressure
- It then injects the vapor directly into the fresh gas flow using a differential pressure transducer
Effects and side effects
Cardiovascular
- At high doses, desflurane can cause a paradoxical tachycardia
- Reduces SVR
Respiratory
- Dose dependent decrease in minute ventilation
- Pungent smell can trigger laryngospasm and breath holding
Neurological
- Hypnosis with MAC of 6.6
Metabolism
- 0.02% metabolised by hepatic CYP450 enzymes
What is the blood gas partition coefficient?
- The ratio of partial pressure of anaesthetic agent in the blood vs the alveolar gas when the two phases are at equilibrium
Assuming both blood and gas phases are of equal volume and at the same pressure at 37ºC.
- This coefficient corresponds to the speed of onset of the anaesthetic agent
- This is because it is the partial pressure exerted by the agent in the blood and therefore the brain that determines the depth of anaesthesia, not the total number of molecules present
- Agents that are more soluble in blood exert a lower partial pressure, and therefore have to build up a much higher concentration before having any clinical effect
The blood:gas coefficients you need to know
- Desflurane - 0.42
- Nitrous oxide - 0.47
- Sevoflurane - 0.65
- Isoflurane - 1.4
- Enflurane - 1.8
- Halothane - 2.3
- Methoxyflurane - 12
A higher blood gas coefficient means slower onset.
What is the oil gas partition coefficient?
- The ratio of partial pressure of anaesthetic agent in oil or fat vs gas at equilibrium
This essentially tells you how much the agent enjoys clambering into the brain and exerting its anaesthetic effect. The higher the coefficient, the greater the proportion of your vapour that finds its way into the brain.
- It relates to the potency of the agent, and therefore the MAC
- Isoflurane has a O:G coefficient of 98, and is therefore much more potent than Desflurane, with an O:G of 19
The oil gas coefficients you need to know
- Nitrous oxide - 1.4
- Desflurane - 19
- Sevoflurane - 51
- Enflurane - 98
- Isoflurane - 98
- Halothane - 224
- Methoxyflurane - 0.16
A large oil:gas coefficient means more potent, so a smaller MAC required for adequate anaesthesia.
Useful Tweets
When hypothermia starts (30.0ºC), hypnotic requirements are exponentially reduced.
— P Gonzalez-Pizarro (@dratropin) February 21, 2023
Here’s the pEEG with fentanyl 7 mcg/kg/h and Sevoflurane 0.25%
📍Only slow and delta waves
Monitoring allow us to decrease drugs without compromising safety pic.twitter.com/UBPcrGETKR
The financial and environmental impact of purchased anaesthetic agents in an Australian tertiary hospital@gingersauruz @Austin_Health
— Anaesthesia and Intensive Care (@AICjournal) February 9, 2023
🔗 https://t.co/rBp6TCLjpl pic.twitter.com/1DhpX3j4nx
References and Further Reading

Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
