Hyponatraemia on ICU

Take home messages
- Look at urine sodium, and paired osmolalities
- Don't increase sodium by more than 6mmol per 24 hours
- Give hypertonic saline to acutely symptomatic patients
It's common
Hyponatraemia is the most commonly encountered electrolyte disturbance that you're going to see in your day-to-day practice.
Sodium is rather important, not only for jumping in and out of nerves, and driving literally every active process in your body, but also because over 85% of your osmotic drive comes from sodium.
It's also bad
Hyponatraemia causes cerebral oedema, dizziness and altered mental state.
It is an independent risk factor for mortality and general badness, so it's good to know what to do with it.
It also comes up in the exam
This question was a new one in the CRQ Februrary 2024. Classification of hyponatraemia, causes of pseudohyponatraemia, how quickly you can correct hyponatraemia, and the difference between cerebral salt wasting syndrome and SIADH was not well answered.
So we thought we'd go through it here.
Some salty numbers to start
- Sodium should be around 134 - 146 mmol/litre
- Usually you have around 58 mmol in your body per kilo of body weight
- Daily requirement is 2 mmol per kilo
- Serum osmolality 280–295 mOsm kg−1
- 99% of sodium is reabsorbed in the proximal tubule and loop of Henle
- Most of the fine tuning happens in the distal tubule and collecting ducts
Let's build it up slowly
Hyponatraemia is complex and poorly understood (especially by yours truly) so we'll start with the basics and work it out as we go.
How does the body control sodium concentration?
Using a mechanism that only evolution could possibly have devised, the body controls water levels by adjusting sodium, and vice versa.
All of this relies on the fact that sodium is hugely osmotically active, and is responsible for most of the tonicity or osmolality in the blood.
If you move salt, water will follow
Symptoms of acute hyponatraemia happen when the change in osmolality is too fast for the brain to compensate for, and fluid is sucked into the now relatively more tonic intracellular space, causing cerebral oedema, seizures, coma and other badness.
Symptoms of chronic hyponatraemia (fatigue, dizziness) occur when the change is slow enough for the brain to adjust for initially, but eventually reaches a point where it runs out of other osmotic tools with which to effectively compensate.
Adjusting sodium concentration with water
- Any change in sodium or water level will produce a slight alteration in extracellular fluid osmolality
- You only need an increase of around one or two percent to stimulate the posterior pituitary to start producing antidiuretic hormone (a.k.a. vasopressin)
- This triggers V2 receptors in the distal convoluted tubule and collecting duct, shoving aquaporin-2 channels into the tubular membrane and increasing water reabsorption
- The patient also feels rather thirsty
- This leads to increased water retention and intake, and brings the sodium concentration back down
- If on the other hand the osmolality drops, then ADH secretion is reduced and fluid is excreted, and the sodium concentration increases
Voila, sodium levels are nicely controlled.
Adjusting water level with sodium
- Hypovolaemia means less sodium passes through the distal convoluted tubule
- This induces renin secretion from the juxtaglomerular apparatus
- Renin then converts angiotensinogen into angiotensin 1
- ACE in the lungs then converts 1 to 2
- Angiotensin 2 tells the adrenal cortex to release aldosterone
- This tells the collecting ducts to increase sodium retention
- This drags water along for the ride
- Baroreceptors also sense reduced vascular volume and trigger ADH release
- More water is retained as described above
It's quite an effective mechanism too, demonstrated by the huge range of possible urine osmolalities, from around 50 to 1300 mOsm per kg.
Step 1: Resuscitate
You're called to resus because a patient has started seizing and the blood gas shows a sodium of 115 mmol/litre.
At this point it doesn't matter one jolly jot what underlying mechanism is causing the hyponatraemia, whether its euvolaemic, mevolaemic or anyoneelsevolaemic:
The patient has cerebral oedema and is at risk of brain herniation.
Then test the sodium and see if symptoms have improved, and repeat the dose if required
Continue until symptoms improved and sodium has risen by around 2-5mmol.
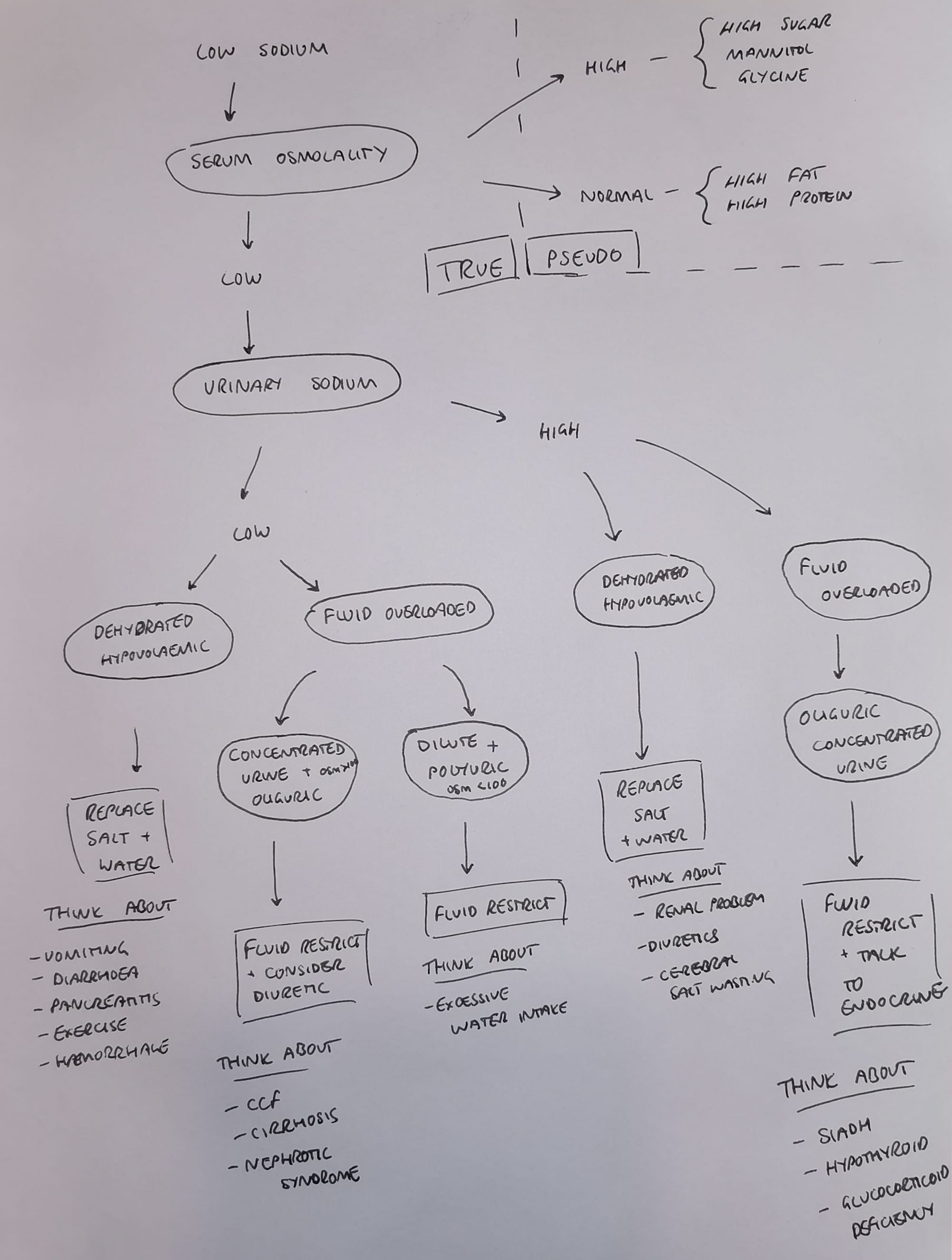
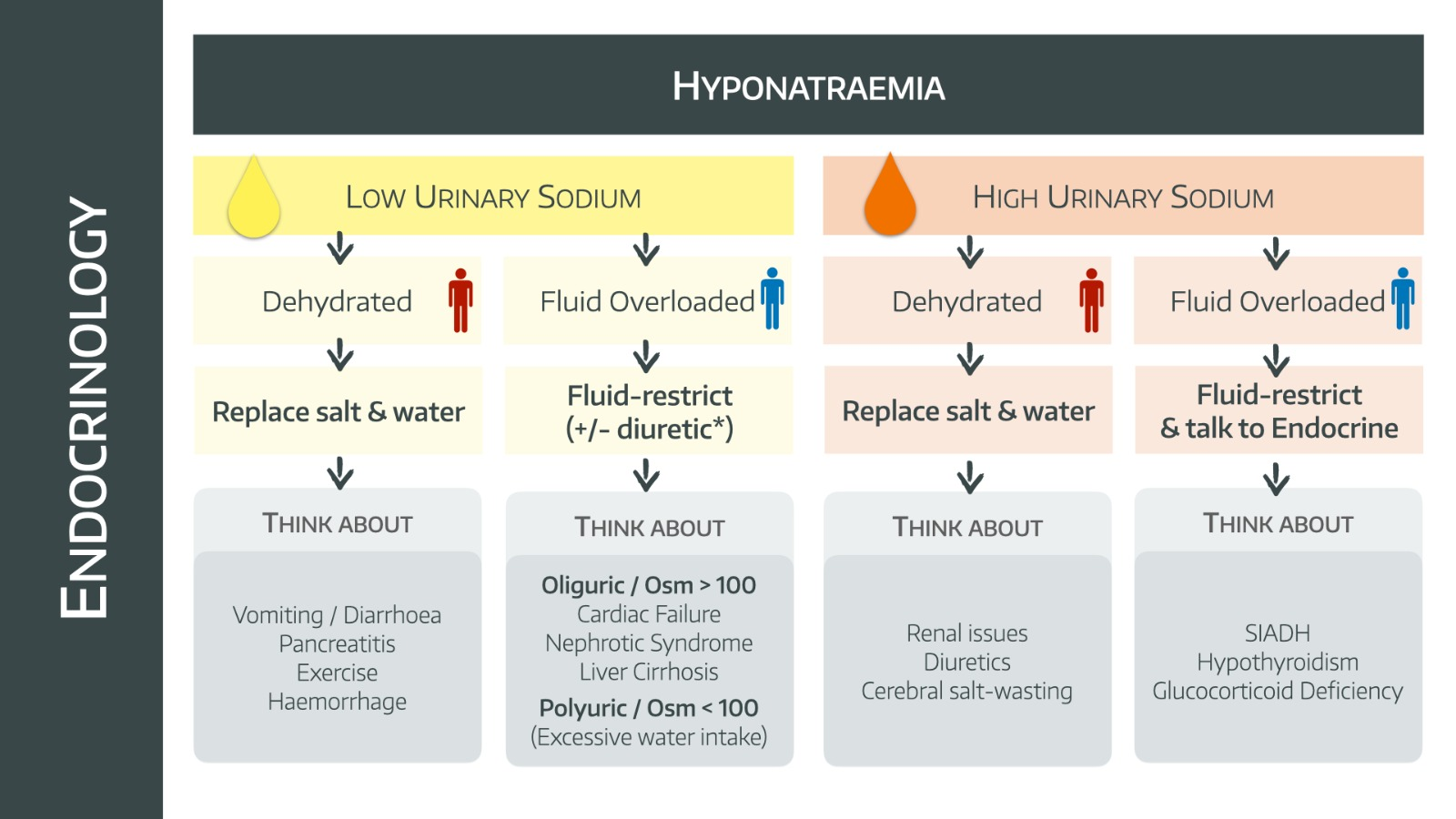
Step 2: True vs pseudo
Now that we have a non-seizing patient with a slightly less disastrously low sodium, we have a bit of time to do some thinking.
If you're the anaesthetist on the crash team, be honest you're probably leaving at this point, but if you're on ICU then you're going to start doing some of the following.
We mentioned earlier that sodium gives the blood much of its osmolality. Therefore if the sodium is truly low, we'd expect the blood to lose much of its osmolality.
Here we meet our first decision in the flow chart.
We'll discuss the 'untrue' or 'pseudo' categories in a bit, but let's assume we have a true or hypotonic hyponatraemia in front of us.
It's one or the other
If you're measuring a serum sodium concentration and the result is a lower number than you'd like, then there are really only two options:
- The water level is low, but the sodium is even lower
- The sodium level is okay (or high) but the water level is even higher
That's it really.
Deciding which of these it is, brings us to Step 2
Step 2: Look at the urinary sodium
Low urinary sodium
Dehydrated patient with poor urine output
This one is a normal response of the body's fluid retention mechanism.
- You're injured with massive haemorrhage, or disastrously dehydrated
- Your body desperately tries to retain fluid
- To do this the renin-angiotensin-aldosterone system is running overtime and ADH has shoved as many aquaporins into the collecting duct as possible
- This is all entirely appropriate as a survival mechanism
- You're retaining as much salt as possible in order to retain fluid
- You're also now incredibly thirsty, and probably drink a whole load of hypotonic water, rather than isotonic fluid
- With this and the ADH working full tilt, you manage to retain a little more water than sodium, and so you become hyponatraemic
- But you're still dehydrated, so you're hypovolaemic
- And you've still lost salt in the original bleed/diarrhoea, so you're hypotonic
Hence we call this hypotonic, hypovolaemic hyponatraemia.
This process, and this hypovolaemic, hypotonic hyponatraemia, happens in anyone with major loss of extracellular fluid.
- Diarrhoea
- Burns
- Haemorrhage
- Third spacing
The patient's urinary sodium will be low in non-renal losses, because the kidneys are working and are appropriately retaining salt.
The patient needs salt and water replacement, along with treatment of the underlying cause.
Fluid overloaded patient with poor urine output
This one is not a normal physiological response - it's inappropriate fluid retention.
- Something has activated inapproprate RAAS and ADH activity (such as heart failure or cirrhosis making the kidneys think there isn't enough blood volume)
- The body inappropriately retains salt and water (giving small volumes of concentrated urine with a low sodium)
- You become hypotonic and hyponatraemic, but you're fluid overloaded
The patient needs loop diuretics and/or ACE inhibitors
Causes:
- Heart failure
- Cirrhosis*
- Nephrotic syndrome (low protein = third spacing = intravascular depletion = RAAS and ADH activation)
*This is a double whammy, because not only does the liver disease cause low blood pressure and hypoperfusion of the kidneys, it also means the ADH that is inappropriately released then doesn't get broken down either.
Fluid overloaded patient with lots of dilute urine
This is a normal response to a pathalogical state of fluid excess.
Dilute urine means a urine osmolality of less than 100
- The sodium level in the body may be normal, but is diluted by the extra water
- The body is sensibly trying to get rid of all the excess fluid, while retaining the salt as much as possible
- The urine is less than 100 mOsm/litre and is 'maximally dilute', and has low sodium as this is all being sensibly retained
Causes:
- Beer potomania*
- Water intoxication
*Beer is lots of water and a bit of carbohydrate, with not much sodium, so when you drink lots of it, you metabolise the carbohydrate and suppress any protein break down, reducing the urea production.
This means you don't have much in the way of solute to put into the urine, and therefore struggle to produce enough urine, as it is already maximally diluted.
This leads to fluid retention and hyponatraemia.
It's actually really hard to overwhelm a healthy kidney's ability to excrete water, so usually hyponatraemia due to excessive water intake is usually in the context of existing renal problems.
For example psychogenic polydipsia usually occurs in patients with another cause for iatrogenic SIADH such as SSRIs.
High urinary sodium
Dehydrated patient with inappropriately high urine output
This is still hypotonic hypovolaemic hyponatraemia but for a different reason.
- Something is making the kidneys malfunction
- They're losing salt and water into the urine
- The urinary sodium is therefore high (>20mmol/litre)
Causes
- Diuretics
- Renal failure
- Chronic pyelonephritis
- Saltwasting nephropathy
- Aldosterone deficiency
- Nephrocalcinosis
- Proximal renal tubular acidosis
- Ketonuria
- Cerebral salt wasting syndrome*
The diuretic causes sodium and water loss, triggers ADH release and therefore a bit of fluid retention, but no sodium retention.
The reason thiazides are particularly bad is because they don't mess up the osmotic gradient in the medulla (which furosemide does mess up).
As a result with thiazides you can still reabsorb water fairly well, but not sodium, and so you get high urinary sodium and hyponatraemia.
The patient still needs salt and water replacement, and treatment of the underlying condition or removal of the offending medication.
*Exam answer - Cerebral salt wasting syndrome gives you a dehydrated, inappropriately polyuric patient while SIADH gives you a fluid replete or overloaded and inappropriately oliguric patient.
Fluid overloaded patient with inappropriately low urine output
This is a patient with far too much water on board who is still retaining fluid, but unlike the CCF/Liver patients we've discussed above, their kidneys aren't churning out renin to retain salt and water, they're actively trying to lose salt and water, but something endocrine is stopping them from getting rid of enough water.
They have a high urinary osmolality of greater than 100.
- SIADH
- Glucocorticoid deficiency
- Hypothyroidism
Just give me an algorithm
Here's our algorithm, which we've designed to avoid the incredibly inaccurate process of trying to decide whether someone is 'overloaded' or 'euvolaemic'.
You now just have to decide between 'dehydrated' or 'overloaded'.
Some endocrine bits
Corticosteroid deficiency
- If you have Addisons then you lose your aldosterone production
- This means there's no stimulation of the ENaC channel in the collecting duct
- Therefore you can't reabsorb as much sodium (and excrete potassium)
- Then add in the fact that cortisol is also an ADH inhibitor, so if you're not producing enough cortisol you've got more active ADH floating around
- This leads to water retention and high urinary sodium
This can either be a primary adrenal problem or as a result of stopping steroid therapy too quickly, or by giving too much spironolactone.
The treatment is steroids.
Hypothyroidism
- Unclear exactly how this works
- It's probably a bit like heart failure, where decreased cardiac output means less kidney perfusion
- The kidneys and baroreceptos get upset and more ADH is produced, causing fluid retention
The main thing is to test hyponatraemic patients' thyroid function, and give thyroxine if needed.
SIADH
- There is pathological production of antidiuretic hormone, for whatever reason (trauma/surgery/infection etc)
- Their ion excretion mechanisms still work, so they're able to produce urine with a high urinary sodium
- But as you give them more and more fluid they simply retain the water and excrete the salt
What are the causes of SIADH?
Neuro
- Trauma
- SAH
- Surgery
- Stroke
- Epilepsy
- Meningitis
- Cancer
Respiratory
- Sarcoidosis
- Abscess
- TB
- Pneumonia
Neoplastic
- Small cell lung cancer
- GI cancer
- GU cancer
- Lymphoma
- Mesothelioma
Drugs
- Proton pump inhibitors
- SSRI
- TCA
- Valproate
- Keppra (levetiracetam)
- Oxytocin (very chemically similar to ADH)
- Ecstasy
Other
- Acute intermittent porphyria
- Guillain-Barré syndrome
- HIV
- VR2 gene gain-of-function mutation (nephrogenic SIADH)
How is SIADH diagnosed?
- Hyponatraemia with low serum osmolality
- Urine osmolality higher than serum osmolality
- Urine sodium greater than 20 mmol/L
- Normal hepatic, cardiac and endocrine function
- No other causes
- No hypovolaemia
- Gets better with water restriction
Talk me through cerebral salt wasting
- ANP and BNP are released by damaged brain (and heart) tissue
- This produces a natriuresis and profound dehydration with salty urine
- The distinguishing point is the patient is inappropriately dehydrated with high urine output.
SIADH, on the other hand, causes water retention and low urine output.
ADH is high in both CSW and SIADH, but in CSW it's in response to the dehydration, and therefore appropriate.
Treatment
This isn't particularly complex - the three options are:
- Giving salt
- Giving salt and water
- Removing water
For the acutely symptomatic patient, you start with hypertonic saline
As we mentioned above, the key here is fighting the cerebral oedema as that's the most pressing (literally) issue at hand.
- 150ml 3% saline over 20 minutes
- Test the sodium
- Repeat if needed
- Continue until symptoms resolve and sodium increased by 2-5mmol/l
Then you want to switch over to the slower, more gradual replacement (or fluid restriction) based on the pathology you think is at play.
For the dehydrated patient, you start with isotonic fluid
They're dehydrated, so they're churning out ADH, so they're diluting down their sodium, but they've also lost sodium.
Give them both back and they get better.
The extra fluid switches off the ADH and with the help of the sneaky salty top up they will urinate their sodium back to normal.
For a hypervolaemic patient, you start with a fluid restriction
The patient rarely enjoys this, but the idea is they'll eventually urinate out the extra fluid and restore the osmotic balance within.
Note that this is likely not going to work if:
- The urine output is very low
- The urine osmolality is very high
Because it suggests the body is in a strong 'retain fluid' mood - probably because the kidneys are underperfused - and might need a bit of extra encouragement to shed some water.
Consider a diuretic, and consider talking to an endocrinologist.
How quickly can I change it?
We know you don't want to drastically change sodium concentrations in a short space of time, because it causes swelling or shrinkage of important structures like the brain and leads to nasty symptoms like seizures and myelinolysis.
Volume replacement can switch off ADH in hypovolaemic patients, and lead to a sudden increase in sodium concentration as they start diuresing properly, so it's crucial to keep monitoring their sodium concentration closely as they start to urinate again.
A bit about osmotic demyelination syndrome
This terrifying and irreversible condition manifests after 48 hours to a week, with symptoms including confusion, dysphagia, dysarthria, paralysis and seizures.
- It's not really called 'pontine' any more, because it can happen anywhere that myelin is present
- It can also be triggered by other osmotically active molecules like glucose or urea
- It can happen even without giving hypertonic saline, if the patient happens to auto-correct too quickly
- Generally only happens below a sodium of 120
Patients at risk:
- Severe malnutrition
- Alcoholism
- Diuretic use
- Liver transplant patients (enormous risk factor)
The cause is an excessively rapid rise in extracellular fluid osmolality.
How quickly can I raise the sodium?
Rate of correction:
- Your brain is far better at adapting to hypotonic extracellular fluid than it is to hypertonic fluid
- Hence you can use this to your advantage with hypertonic saline in raised ICP
- The most important number is less than 6mmol per 24 hours
But what about in acute hyponatraemia where they're seizing and I need to fix it quickly?
Yes good - you do need to alter the sodium concentration rapidly, but by much less than you think.
They're seizing because they've got cerebral oedema and raised ICP, thanks to our closed-box skull and the good old Monroe-Kellie doctrine.
So you only need to bring the intracranial fluid volume down by a tiny percentage to reduce the pressure by a lot.
This means you can give some hypertonic saline initially just to drag some volume out of the brain and get symptom control, (aim to increase sodium by a max of 2-4% over 30 minutes) and then you can slowly bring that level up to something a little more normal over the next few days.
That's where we get the 150 ml of 3% saline over 20 minutes that we keep batting on about.
Some example patients for you
Try the algorithm above on these patients and see if it works for you.
Example patient 1
- 58 year old woman collapses at home and is shown to have extradural and subarachnoid haemorrhage on CT
- Transferred to neurosurgical centre for decompression
- Day six post operative bloods show a sodium of 119 and patient is profoundly oliguric
- Euvolaemic on examination
- Serum osmolality 274
- Urine osmolality 190
- Urinary sodium 38 mmol/litre
This is SIADH, classically kicking in 5 - 7 days after neurosurgery, subarachnoid haemorrhage or head trauma.
Treatment:
- Fluid restrict to less than one litre per day
- Demeclocycline if needed, to induce a spot of nephrogenic diabetes insipidus
- Tolvaptan (V2 receptor antagonist) should only be considered by senior endocrinologist if all else fails
Example patient 2
- 22 year old male with vomiting and diarrhoea
- Tachycardic and hypotensive
- Sodium 128, potassium 3.4, urea 12 and creatinine 163
- Serum osmolality 275
- Urine osmolality 344
- Low urinary sodium
This is a dehydrated patient with high urine osmolality and high urinary sodium.
This is a completely normal response to profound dehydration. He has lost water and salt, but proportionately more salt as the kidneys desperately tried to retain water.
You still need to test TSH to rule out hypothyroidism.
Treatment
- IV fluids (don't forget potassium)
- Stop any meds that might be making things worse (diuretics)
Example patient 3
THIS IS THE ONE THAT GETS EXAMINED A LOT
- 68 year old man has just had a TURP
- He's become confused and short of breath in recovery
- You do a blood gas
- Na 121, K 3.2, slight metabolic acidosis with respiratory compensation
- Serum osmolality low
- Bibasal crackles
This is TURP syndrome
- 1.5% glycine was classically used for irrigation
- It gets absorbed into the blood, and drags the osmolality of the serum down (1.5% glycine is hypotonic at around 200 mOsm/kg)
- This causes an initial hypervolaemic hypotonic hyponatraemia
- Then the glycine causes an osmotic diuresis
- This leads to a later hypovolaemic hypertonic hyponatraemia
Treatment:
- Usually self limiting
- Furosemide can help
- Sodium replacement might be required
Example patient 4
- 72 year old woman with heart failure and alcohol excess presents with shortness of breath and abdominal distension
- Sodium 109
- Potassium 5.3
- Creatinine 144
- Serum osmolality 246
- Urine osmolality 300
- Urinary sodium 20
This is fluid overload, or hypervolaemic hypotonic hyponatraemia
The heart failure causes bad perfusion, which makes the adrenals and kidneys think the body is dehydrated, which causes secondary hyperaldosteronism, and inappropriate fluid retention.
Treatment:
- Loop diuretics (furosemide infusion can be titrated to an acceptable rate of sodium increase)
What can go wrong?
What are the risks of giving hypertonic saline?
- Demyelinolysis
- Hypernatraemia and hyperosmolality
- Fluid overload and heart failure
- Hypokalaemia and metabolic acidosis
- Dilutional coagulopathy
- Phlebitis
- Renal failure
- Rebound intracranial hypertension
- Seizures
- Intracranial haemorrhage
A word about dialysis
- Dialysis can be risky in hyponatraemia, as the dialysate has around 145 mmol/L of sodium, which will gleefully and enthusiastically equilibrate with the blood, causing an intolerably rapid correction of the sodium level, and a shredded pons
- It is possible to make up a hypotonic dialysate and use dialysis to correct hyponatraemia safely, but please don't bring this up in your exam - you'll regret it
What if it's not true?
If your most osmotically active agent is reading low, but you've got enough osmolality happening in the blood, something else is clearly going on.
Pseudohyponatraemia with normal osmolality
- Hyperlipidaemia
- Hyperproteinaemia
This is simple maths-fudging.
Salt can't dissolve in fat or protein, so if there's loads of either of these two in the blood, they'll artificially inflate the apparent volume of blood, and cause the concentration of sodium to seem low.
This is referred to as isotonic pseudohyponatraemia
- Sodium is measured in an ABG machine using indirect ion selective electrode (ISE) sampling which is affected by this problem
- Lab readings can often use a direct ion-sensitive electrode which isn't fooled by the fat or protein
Pseudohyponatraemia with increased osmolality
Something even more tonic than sodium has entered the chat.
- Glucose - drags fluid into vascular compartment and dilutes sodium down
- Mannitol (initially, but then becomes hypernatraemia after all the water gets diuresed out)
- Alcohol intoxication (technically, but usually an alcoholic is hyponatraemic because of the fluid overload and high triglycerides)
- Glycine
Useful Tweets and Resources
Another of the Acute Illness Management series for you. Here we approach the diagnosis of hyponatraemia. #FOAMed #FOAMcc #MedEd #medtwitter https://t.co/fNeobT7yDY pic.twitter.com/SKZXWchhzS
— Jonny Wilkinson (@Wilkinsonjonny) August 24, 2020

References and Further Reading
Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.

