HME Filters

Take home messages
- Cheap, easy to use and reliable
- Take 20 minutes to start doing anything useful
- Can get clogged and cause trouble
Warm and moist
The only thing that cake and the trachea agree on is their ideal operating conditions.
Usually the nose picks up the job of warming and humidifying the air we breathe, so that by the time it touches the delicate epithelium of the trachea and bronchi, it doesn't dry it to a crisp and freeze-exfoliate the living daylights out of it.
Oh, and all that snot covering the turbinates acts as fly paper for a variety of particulate matter and pathogens.
Enter the tube
You've just slid your tube between the cords with dexterity and skill, and in the process have bypassed the finely-tuned apparatus for achieving this beautiful warm moistness we desire.
Moist.
What happens when you don't humidify inspired gases
- Nothing, for a little while*
- Mucus dries out and thickens
- Cilia slow down and struggle to waft mucus
- Mucosa starts to dry out
- Epithelium peels off and ulcers develop
- Thick, dry mucus forms clumps that occlude lower airways
- Atelectasis and infection begin
*Most short anaesthetics will fall into this time category
Now enter the HME
If you've ever worn a scarf/balaclava/ninja mask over your mouth and nose in the winter, you'll have noticed that the material ended up warm and soggy rather quickly.
In 1953 clever Dr Cole used a glass cylinder with moist paper pellets inside and reported that it was "found to condition respiratory air as effectively as the highly vascular mucosa of the upper respiratory tract".

How it works
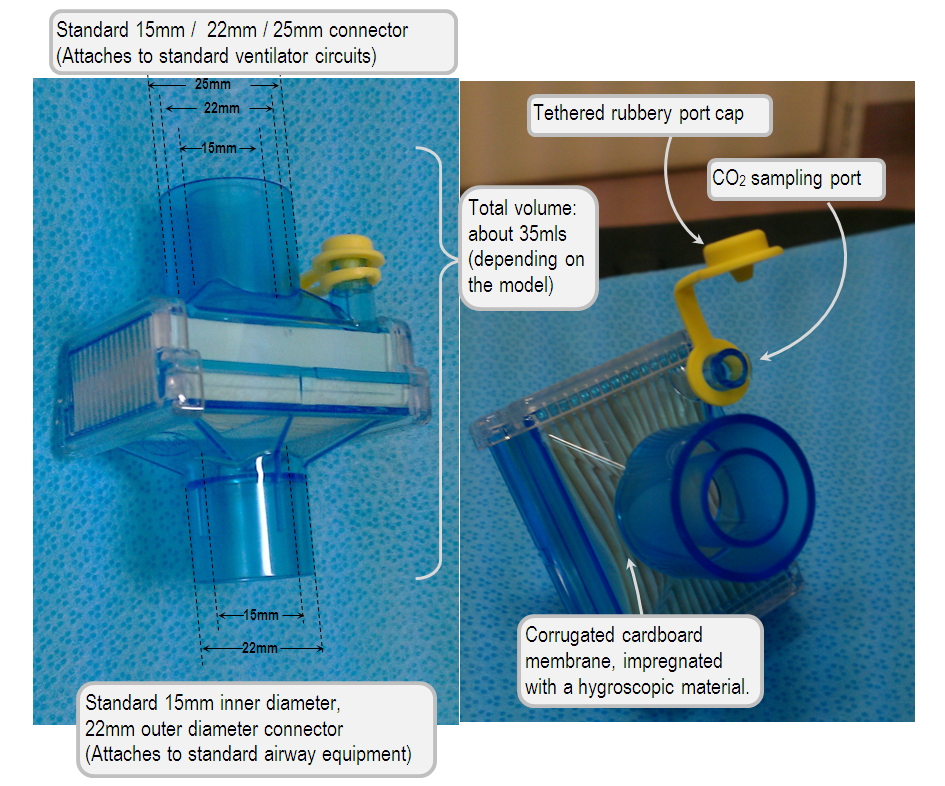
These compact little widgets slot directly into the breathing circuit - with standard 15 and 22 mm connectors - usually at the patient end.
They consist of a paper or sponge filter covered by a hygroscopic material, which is a posh word for 'something that sucks moisture out of air'.
The filter collects water and heat from the exhaled gas (Condensation is an exothermic reaction).
Inspired fresh gas is then warmed and humidified by the water on the filter, and in the process this cools and dries the HME, ready for the next exhaled breath.
It's generally pretty good:
- Cheap and easy to use
- Easy to replace when expired or waterlogged
- Effective for short-term ventilation (up to 48 hours or so)
- The HME filter can achieve 25 g/m3 , compared to 34 g/m3 achieved by the nose and pharynx, meaning it has approximately 65% efficiency
- This is insufficient for long term ventilation but slows damage sufficiently for a day or two
Disadvantages:
- Takes 15 minutes to reach working humidity and temperature
- Relies on enough but not too much minute ventilation and tidal volume to work (especially important for paediatric patients)
- Affected by temperature and humidity of respiratory gases
- Only properly efficient for around 24 hours
- Resistance to gas flow of 0.1 – 2 cmH2O
- Can become blocked with secretions and water
- Increases dead space of circuit
- Theoretical infection risk, particularly pseudomonas
What gets stuck in the sponge?
- Water
- Particles and dust from gas supply
- Bacteria
- Soda lime dust
- Volatile organic compounds
- Anaesthetic gases
- Nebulised drugs
CO2 sampling

The end tidal CO2 sampling tube connects to the side facing away from the patient - after the moisture and gunk has been removed from the exhaled gas - for obvious reasons.
There are often other points in the breathing circuit with holes where CO2 monitoring can be attached instead.
In which case this little hole may make its existence known now and again by randomly popping open and creating an enormous leak, triggering a variety of alarms and sending you on a fishing expedition to find the break in the circuit.
If your sponge is completely waterlogged then lots of CO2 can get trapped in the filter itself, and if it's clogged with secretions then the resistance will start climbing as well.
Baseline resistance of a new filter:
- 0.8cm H2O resistance at 30 litres/min gas flow
- 2.1cm H2O resistance at 60 litres/min gas flow
- Clearly this resistance will increase as it becomes clogged up with water, drugs and secretions
So if you're looking at a strange trace on the monitor with high pressures on the vent, maybe try changing the HME?
Limitations
Dead space
- The filter adds dead space, the volume of which needs to be added to the achieved tidal volume in order to ventilate the patient effectively
- If you're already struggling with a tight, stiff lung and huge PaCO2, then the HME isn't exactly helping the cause.
Secretion sponge
- The HME filter is spectacularly good at getting completely blocked up with secretions
- This causes high resistance, hypoxia and lots of alarms to start bleeping
- If you have lots of secretions, you need active humidification
Big breaths
- If your patient is taking enormous tidal volumes and hitting a large minute volume (more than 10 litres per minute or so) then your HME filter will struggle to keep up
- A large inwards breath will rapidly cool and dry the filter to the point where it's not humidifying or warming the second half of the breath
Long term use
- HME filters last for a maximum of 72-96 hours and ideally should be changed every 24-48 hours
- The longer you ventilate someone, the more they need active humidification
- Otherwise they'll get thicker and thicker secretions and the HME will just clog up with gunk and stop working
Nebulisers
- If you are regularly nebulising a patient then a lot of the drug is going to deposit into the HME filter with the exhaled breath
- It will be even less effective if you make the mistake of putting the filter downstream of the nebuliser
Where should I put it?
If you've managed to attach it somewhere in the breathing circuit, the right way round and without a leak, then you've already done marvellously, well done you.
However to actually work, you want it as close as physically possible to the patient's airway, where both temperature and humidity are highest.
If you stick it at the machine or ventilator end, then the heat is lost to the tubing and the moisture forms droplets in the breathing circuit contributing nothing helpful to society and causing the ventilator to alarm.
Two points about low flow circle systems
- There is a little bit of humidification and warming offered by the soda lime canister, which reduces as fresh gas flow increases
- Soda lime dust is less of a risk nowadays with modern 'dustless' canisters, however the HME does also help protect the patient against dust particles
A Poem
We asked ChatGPT to write us a poem about the HME filter, and frankly, we love it.
The Tale of the HME Filter
In the world of breath, where air flows free,
Lives a humble hero, the HME.
With gentle grace, it stands its ground,
Warming the air as it moves around.
It catches moisture from each breath out,
And gives it back with never a doubt.
A clever filter, cool and neat,
Keeping the lungs from feeling the heat.
No power it needs, no plugs or wires,
Yet it fights off dryness and cool that tires.
It traps the heat from breaths expired,
And returns it warm, just as required.
But like all things, it’s not immune,
To clogging up too soon, too soon.
So handle with care, replace with pride,
For in patient comfort, it does confide.
So here’s to the HME, small but bright,
Working each day, and through the night.
In the breath of life, it plays its part,
A quiet guardian with a generous heart.
Here are some closely related posts


Useful Tweets
Today I learned: Inhaled epoprostenol clogs HME filters due to glycine diluent➡️should change filter q 2-4 hrs.
— Jordan Holloway, MD (she/her) (@jholloway_MD) March 24, 2023
Signs HME should be changed:
- ⬆️ peak pressures
- Unexplained hypoxia/hypercapnia
- ⬆️ PA pressures
- Filter accumulation#MedTwitter #Anesthesia #MedEd #FOAMEd pic.twitter.com/HVlu9chuir
References and Further Reading
Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.