Hering-Breuer and the respiratory reflexes

You're now thinking about your breathing.
You weren't before, but you are now.
Sorry.
It's okay, you can just breathe normally. Except you can't, because you're still thinking about it.
Normal breathing is called eupnea - think about that instead.
Humans are strange creatures in many ways, and one of them is that we have extremely powerful conscious control of our breathing allowing us to choose how and when we breathe - within survivable limits of course.
Now, unless you suffer with Ondine's curse, you fortunately don't need to consciously think about your breathing all the time, it's mostly automatic.
Negative feedback
Pretty much every homeostatic mechanism in the body is driven by a negative feedback loop, where too much of something switches the machine off, and too little switches it on again.
The same applies to breathing, with a variety of inputs to the respiratory centres in the medulla and pons providing highly sensitive, breath-to-breath adjustments to the respiratory rate and depth, to keep all the numbers where they should be.
The medulla
This is the main protagonist of the respiratory show, with direct neural connections to the muscles of respiration.
It has two main regions of interest:
- The dorsal respiratory group stimulates inspiration
- The ventral respiratory group stimulates expiration
The pons
Sits just below the medulla.
- Controls rate of respiration
Also has two main regions to do this:
- The apneustic centre - stimulates inspiration for long, deep breaths
- The pneumotaxic centre - inhibits inspiration, coordinating timing and respiratory rate
These two work as antagonists and thus maintain a steady homeostatic breathing pattern.
You also have a bunch of reflexes built in, most of which pass through the medulla, with or without a bit of pontine poking.
Pulmonary reflexes
As a general rule, the neuromuscular reflexes that have been pre-programmed into your body by billions of years of evolution are pretty nifty.
They allow an action or effect to be initiated quickly and efficiently by the organs involved, without the input of the higher decision making components slowing things down.
Maybe the NHS needs some reflexes.

If you think of the lungs as a delicate sponge of incredibly thin tissue, suspended in a constantly moving cage of muscle and bone, responsible for keeping everything else alive, it then makes sense that it has rather a few safety reflexes to stop everything going wrong rather rapidly.
What receptors are there in the respiratory tract?
Larynx
- Cold
- Irritant
- Pressure
- C-fibre
Lower airways
- Slowly adapting stretch receptors
- Rapidly adapting stretch receptors
- C-fibres
- Neuroepithelial bodies
Meet Doctors Hering and Breuer
In 1868 these spritely German-and-Austrian-respectively gentlemen noticed that animals would briefly stop breathing if you inflated their lungs for a sustained period while anaesthetised.
Before getting bored and wandering off to become the founder of psychoanalysis with his buddy Freud, Breuer and his chum Hering decided to investigate this further.

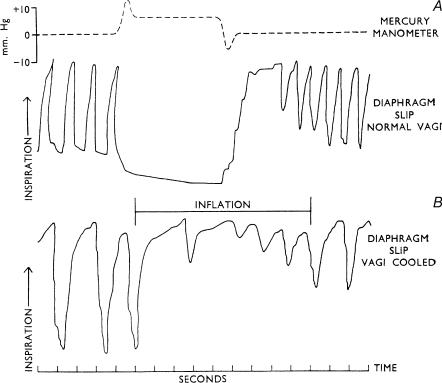
The Hering-Breuer reflex protects mammalian lung from overinflation.
Birds, reptiles and amphibians have similar mechanisms, but not quite as swish as ours.
How it works
- The lung inflates
- Stretch receptors in the bronchial and bronchiolar walls activate the vagus nerve
- This relays to the inspiratory area of the medulla and the apneustic centre of the pons
- The inspiratory centre is directly and indirectly* inhibited - *the apneustic centre is prevented from activating the inspiratory centre
- This inhibits the motor neurons supplying the inspiratory muscles
- It also stimulates motor neurons to the expiratory muscles
The net result is that the inspiratory effort is reduced and then terminated as the lungs reach maximum safe levels of inspiration, preventing overstretching and potential volutrauma.
At the same time, the afferent pathways send projections over to the cardiac vagal motor neurons in the nucleus ambiguus as well as the dorsal motor vagal nucleus.
- This reduces vagal tone to the heart
- This causes a transient increase in heart rate while the lungs are fully inflated
- This is called sinus arrhythmia
An entirely personal anecdote
When extubating a patient, many anaesthetists (ourselves included) recommend having some PEEP on board, and even squeezing the bag to fill the lungs as you take the tube out.
The proposed benefits are:
- Recruits the lung and reduces atelectasis
- Fills the FRC with oxygen such that any silliness (laryngospasm) isn't quite as stressful to manage
- Activates the stretch receptors and the HBR, possibly reducing the likelihood of a big inspiration and coughing fit but this is anecdotal at best
The deflation reflex
This is the other much less famous lung reflex named by the same dynamic duo.
This one aims to shorten exhalation when the lung is deflated, and is activated by a combination of stretch receptors and proprioceptors that tell the brain how inflated the lung is.
Again, travels via the vagus but only stimulates the inspiratory centre of the medulla.
Doesn't appear to be overly important in humans but may play a role during exercise.
A really nerdy bit you definitely don't need
Breuer didn't know whether the inflation reflex (the Hering-Breuer reflex proper) and the deflation reflex (the other bit) were part of one reflex arc, or two separate mechanisms.
In theory, if stretch causes vagal inhibition of the inspiratory centre to reduce inspiratory effort, surely the simple removal of this vagal tone will cause an increase in inspiration?
Henry Head (see below) had a terribly clever idea.
He gave a few unhappy rabbits bilateral traumatic pneumothoraces, and compared the resulting inspiratory effort to others, in whom he simply cut the vagus nerves.
The logic goes like this:
- If it's all mediated through simple vagal tone, then cutting the vagus should give a maximal response
- If there's something else going on, triggered by the deflation of the lungs themselves, then a bigger response will be seen here
He found a much stronger inspiratory effort to be generated by the pneumothorax, clearly suggesting the existence of an entirely separate reflex pathway.
So there you go.
This is of no exam value whatsoever.
Other reflexes to know about
Cough reflex
Reason for existence
- To clear objects causing potential obstruction and irritants from the airway
How it works
- Mucosal receptors in larynx, trachea and bronchi detect foreign irritants
- Afferents via vagus to medulla
- Efferents via multiple pathways resulting in rapid inhalation, glottis closure, forced expiration against closed glottis, then glottic release
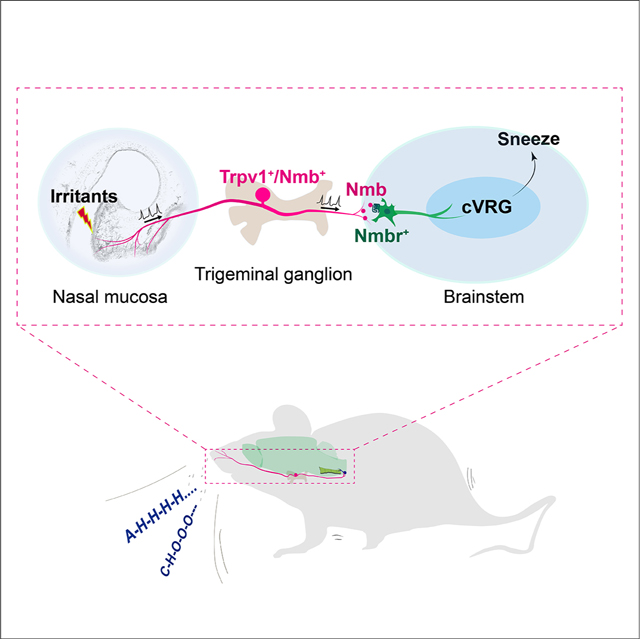
Sneeze reflex
Reason for existence
- To clear irritants from nose and nasopharynx
How it works
- Mucosal receptors in nasal mucosa
- Afferents via trigeminal to the caudal ventral respiratory group in the brainstem
- Efferents to various targets resulting in a deep inspiratory effort, followed by a forced expiration with varying glottic involvement (a.k.a. the Dad sneeze)
Apneustic reflex
Reason for existence
- To help regulate depth and rhythm of breathing
How it works
- Activation of the apneustic centre causes prolonged inspiration
- The pneumotaxic centre then inhibits the apneustic centre, and terminates inspiration
J-receptor reflex
Juxtapulmonary capillary receptors are found in the pulmonary interstitium, right next to the capillaries, and detect interstitial pressure
They're also called pulmonary c-fibre receptors
Reason for existence
- To adjust respiratory mechanics to deal with excessive fluid or increases in pressure in the lung (we think)
- Particularly activated in pneumonia, heart failure and pulmonary embolus
How it works
- Afferents through nonmyelinated fibres via vagus nerve
- Induces apnoea, followed by rapid shallow breathing, bradycardia and hypotension
Chemoreceptor reflexes
These are the main drivers of your day-to-day respiratory effort.
Reason for existence
- To adjust ventilation to maintain homeostatic levels of CO2 and oxygen in the blood
How it works
- Peripheral chemoreceptors respond to PCO2 and pH via the carotid bodies (glossopharyngeal) and aortic bodies (vagus nerve)
- Central chemoreceptors in the medulla respond to CO2 levels in the CSF
- These activate the respiratory centres in the brainstem, causing an increase or decrease in minute ventilation as required
Dive reflex
Most babies will reflexively hold their breath if you dunk them into cold water.
Please don't dunk babies into cold water.
Reason for existence
- Avoid drowning
How it works
- Cold stimulation of the face sends afferents via the trigeminal nerve
- This induces a reflex bradycardia, apnoea and peripheral vasoconstriction
Laryngeal reflex
Different to the cough reflex.
Reason for existence
- Stimulation of laryngeal receptors by a potentially airway-compromising foreign body causes the glottis to slam shut and protect the delicate trachea and bronchi
- Particularly useful during swallowing
How it works
- Laryngeal irritant receptors
- Trigger afferents via superior laryngeal nerve
Head's paradoxical reflex
Sometimes, stretch of the lung tissue and respiratory muscles induces further inspiration.
This is one of the very few examples of positive feedback in an otherwise homeostatic physiological system.
Henry Head - the world's most appropriately named neurologist - himself wrote of this reflex 'I am totally at a loss to account for its appearance'
It was later found that entirely different receptors were responsible for this reflex:
- Rapidly adapting pulmonary stretch receptors (RARs) increase inspiratory effort
- Slowly adapting receptors (SARs) are responsible for the Breuer-Hering reflex
Reason for existence
- Great for babies taking their first breath
- Also useful during exercise, and in preventing atelectasis during normal quiet breathing*
*If you've ever wondered why you'll just randomly take a big breath out of nowhere - it's probably this.
What's the difference between apneustic breathing and Cheyne-Stokes?
Apneustic breathing
- A prolonged period of gasping inspiration
- Followed by a brief and insufficient expiratory effort
- A rate of 1 to 2 breaths per minute
- Caused by pontine trauma, stroke or ischaemia
Cheyne-Stokes breathing
- A cyclical respiratory pattern that includes periods of apnoea
- A progression of increased rate and depth of respiration followed by smaller, shallower breaths
- Can occur while awake but usually occurs during sleep or when unconscious
- Can be associated with cardiac or renal failure, and overdose
So what's agonal breathing?
- Slow, shallow, irregular respiratory pattern as a result of hypoxic brain injury
- Often progresses to apnoea
References and further reading
Authors to follow
If you're interested in reading more about this topic then we suggest following the works of John Widdicome who has written extensively on the topic and is enjoyable to read.