Head Trauma

Take home messages
- You're trying to prevent secondary brain injury
- Don't forget about the other problems
- Hypoxia doubles mortality, as does hypotension
The damage is done
When head trauma happens it's usually fairly brisk - something large, heavy or speedy interacts enthusiastically with the skull in a short space of time.
The primary injury has already happened, and there's little you as the tube-wielding anaesthetic registrar in the hospital down the road can do to prevent this.
Who gets it?
- 80% male
- Falls
- Assault
- RTC
The more severe injuries are usually RTCs and around 1/3 will have other injuries as well.
What you, the paramedics, HEMS, ED and the neurosurgeons are all trying to do is reduce the severity of secondary injury.
Blunt vs penetrating
As a general rule, trauma can be blunt, penetrating or psychological.
All are important, but here we'll focus on the first two.
If you have a patient with penetrating head trauma, they need to be in front of a neurosurgeon as soon as possible, and often this process is expedited by the prehospital team, meaning you don't see them at all if you're running CEPOD overnight in a sleepy DGH.
But hey - there are always surprises.
What are my key concerns?
- Airway and C spine protection
- Oxygen delivery to an injured brain
- Maintenance of cerebral perfusion pressure
- Avoidance of secondary brain injury
What is neuroprotective ventilation?
You use your vast understanding of physics, physiology and chemistry to twist dials and push buttons on the ventilator that will mean less pressure and more oxygen in the brain.
To do this you want enough arterial pressure taking blood to the brain, enough venous drainage to ensure the pressure inside the head doesn't get too high, and the right levels of oxygen and CO2 to avoid excessive vasospasm or vasodilatation.
Here are all the things to do for your patient that don't involve surgery.
Encourage adequate venous drainage
- 30° head up to
- Use tube tapes not ties
- Avoid excessive PEEP
Avoid cerebral vasospasm or raised intracranial pressure
- Avoid hypercapnoea
- Avoid hyperoxia
Maintain adequate blood supply to the head and avoid secondary metabolic injury
- Aim MAP 80-90 mmHg
- Sedate and treat seizures
- Normoglycaemia
- Prevent fevers and hyperthemia
A Scan is not a Plan
The point here is that the surgery is the important bit for any traumatic intracranial haemorrhage, and any unnecessary delay is going to increase mortality and morbidity
Realistically speaking, your trauma patient is getting a scan before the neurosurgeons are going to be interested, especially if a prescription of diesel or kerosene is required to get them there.
The key is not to delay unnecessarily - the surgeon will fix things, the scan won't.
Who gets an urgent scan?
- GCS less than 13 on initial assessment
- GCS less than 15 at 2 hours after the injury
- Suspected open or depressed skull fracture
- Haemotympanum, panda eyes, Battle's sign, CSF leak - signs of basal skull fracture
- Post-traumatic seizure
- Focal neurological deficit
- More than 1 episode of vomiting
Resuscitate what you can treat, then get in the van.
Monro Kellie
There is a 1.5kg blob of impossibly intricate neural wetwork inside a closed box, with a litre of fluid being pumped in and drained out every minute.
And it's just been assaulted by something large, heavy or speedy, so it swells.
It's already angry, it might be bleeding as well, and it needs careful TLC to stop the existing injury from spreading.
Maintaining perfusion pressure
Just as electrons need a potential difference to flow, fluid needs a pressure gradient to drive forward movement.
- Flow = pressure gradient/resistance
Now, your pressure gradient is also called your cerebral perfusion pressure and is determined by:
- CPP = Mean arterial pressure - (ICP + CVP)
Your cerebral perfusion pressure needs to be at least 60 mmHg, so if your ICP is 10, and your JVP is 10, then you're looking at a MAP of 80 mmHg to achieve this.
Intracranial pressure
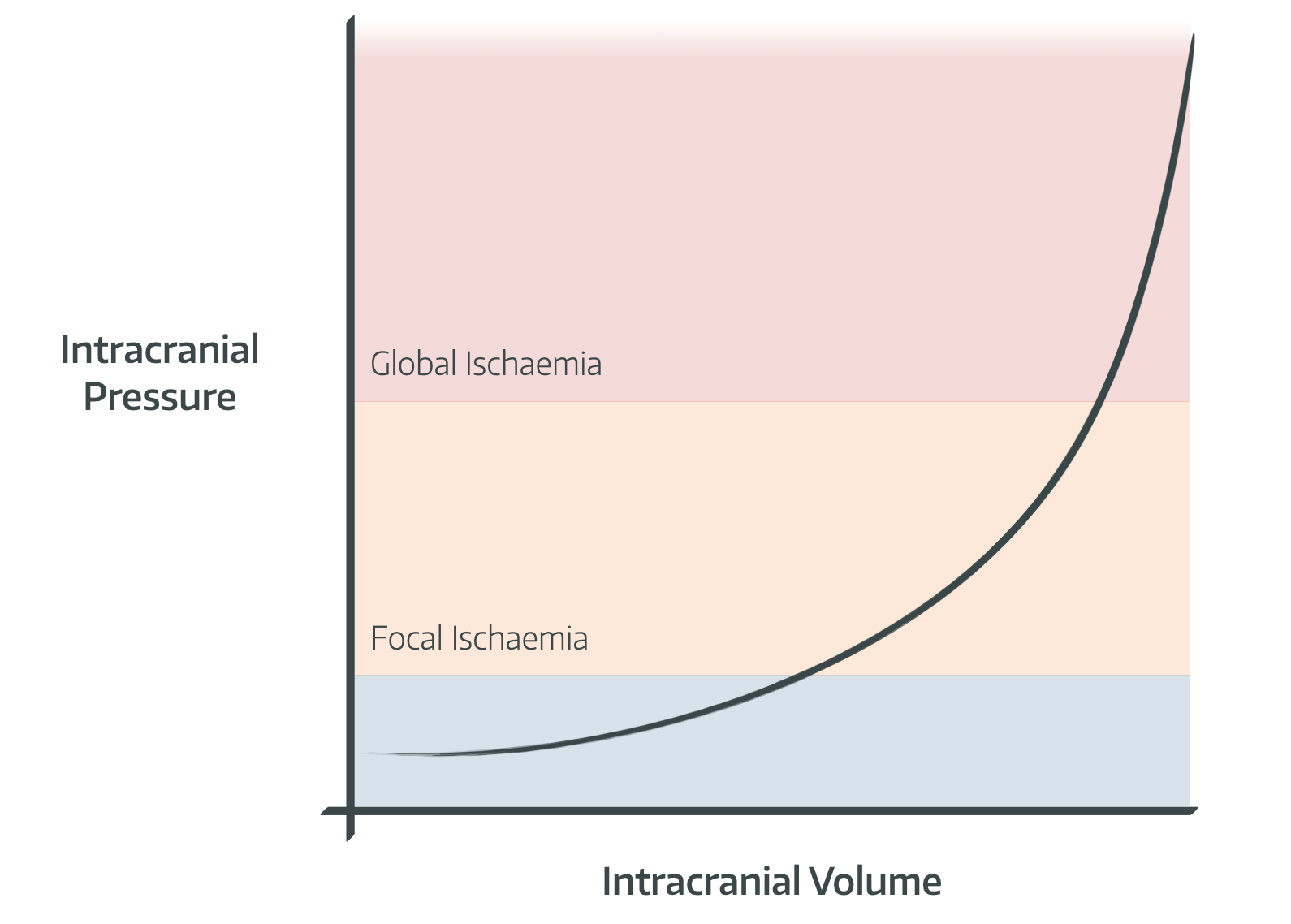
Numbers to know
- Normal intracranial pressure is 10mmHg
- Above 20 mmHg is bad news
- Above 70 mmHg and you're looking at brain herniation
- Normal blood flow is around 50-55ml per minute per 100g brain tissue
Here's our more in depth post on intracranial blood pressure
How bad is it?
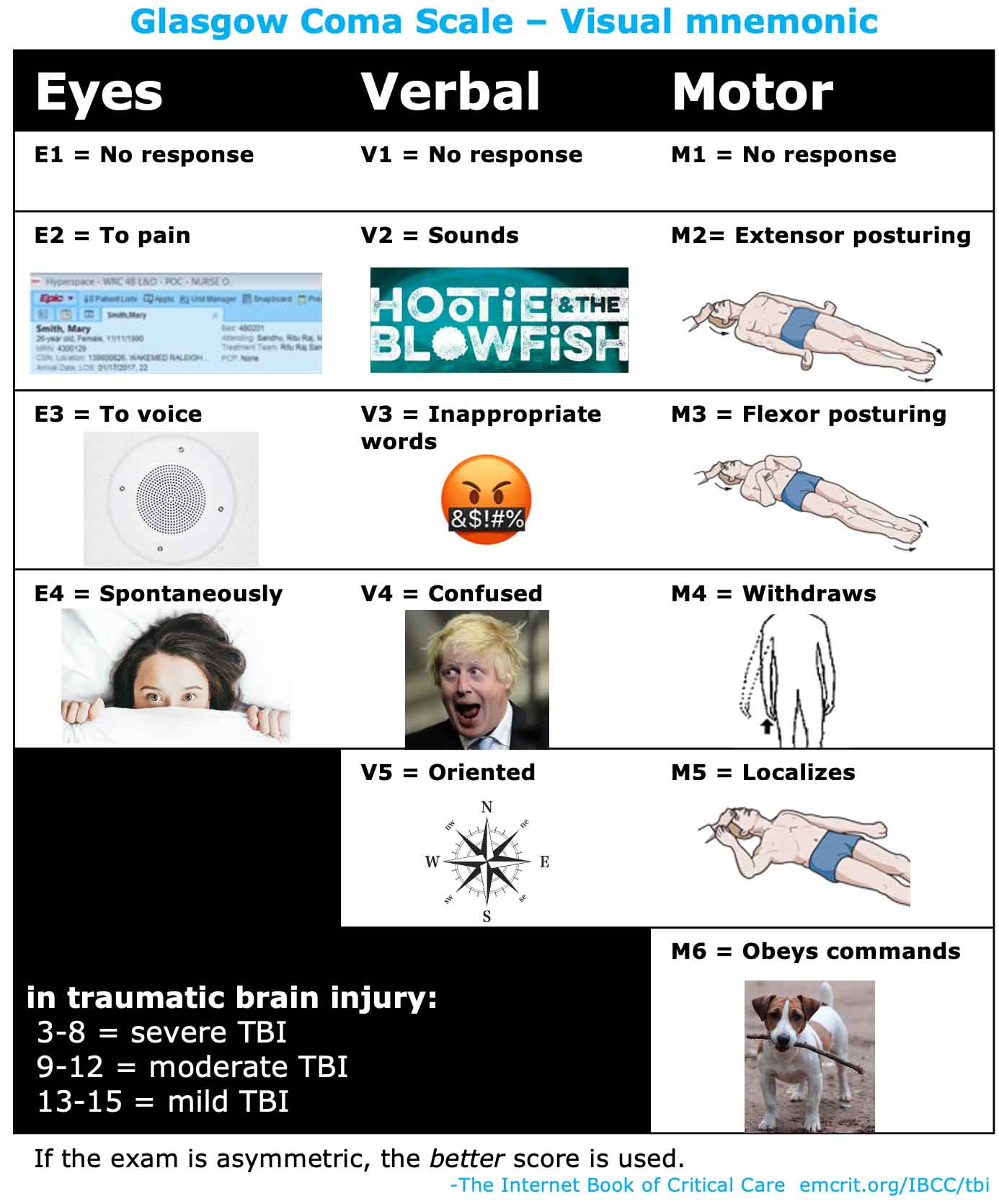
Determining the severity of traumatic head injury is the only time we're actually supposed to use GCS.
In 1974, two surgeons in Glasgow, Graham Teasdale and Bryan Jennett, decided we needed a standardised way of assessing how bad a patient's head injury is.
Because 'stuporous' and 'obtunded' are somewhat ambiguous.
Apparently the score is so good, we use it (completely inappropriately) every time anyone is even remotely sleepy.
- GCS >14 = mild
- 9 - 13 = moderate
- <8 = severe
It's fairly reliably predictive of how bad the badness inside the skull is:
- GCS 15 - 10% will have something to see on CT, and 0.5% will need surgery
- GCS 13 - those numbers increase to 25% on CT and 1.3% will need surgery
What is diffuse axonal injury?
- A shearing insult as a result of rapid changes in velocity - usually deceleration
- Multiple tiny punctate haemorrhages
- Bad outcome
Subdural haemorrhage in a young healthy trauma patient is bad news - a lot of force has been imparted to the head and there is likely significant diffuse axonal injury as well.
The sudden drop
Not infrequently one may be called back to resus to re-review the patient that was an uneventful trauma call earlier in the shift.
A young, otherwise well patient had an unfortunate interaction with a car, pavement or weapon and was brought in by the paramedics with a GCS that warranted a scan but no immediate anaesthetic input.
However since then his GCS has plunged and he now requires airway protection and ventilatory support.
What you can do to help
As is often the case in our line of work, the definitive management is going to be done by somebody else, but we can at least do a fair bit to assist.
Here is the comprehensive list of all the things you can help with
- Swelling and raised intracranial pressure.
- Loss of cerebral autoregulation
- Hypoxia
- Hypercapnoea and spontaneous hyperventilation
- Seizures
- Fever
- Vasospasm
How to help
- Really thorough, structured resuscitation as per usual
- Prevent secondary injury - avoiding hypotension, hypothermia, hypoxia, hypercarbia
- Especially during intubation
- Don't intubate through the nose
- Reduce cerebral oxygen demand by preventing and treating seizures and anaesthetising the patient
- Reverse warfarin and deal with coagulopathy as required
- Tranexamic acid within 3 hours - à la Crash 2
- Effective and efficient communication with the relevant teams - ICU, neurosurgery, major trauma centre - depending on your institution's set up
When should I get a neurosurgeon involved?
Neurosurgical involvement is indicated if:
- Persistent GCS <8 or worsening GCS
- Unexplained confusion for more than 4 hours
- Status epilepticus
- Penetrating head injury
- CSF leak
- Surgically significant pathology on scan - eg >5mm midline shift or an enormous bleed
What should I do for penetrating head injury?
- Leave the weapon/artifact where it is
- CT head
- Anticonvulsants (1g Phenytoin or 20-30mg/kg Keppra)
- Broad spectrum antibiotics
- Get a neurosurgeon involved ASAP
- They need to do some ICP monitoring
Signs of raised intracranial pressure
- Bradycardia
- Hypertension
- Apnoea or irregular breathing
This is the dreaded Cushing's reflex and is bad news - urgent decompression or at least hypertonic saline is needed.
What are the indications for intubation in traumatic brain injury?
- Loss of airway reflexes
- Facial trauma with threatened airway (bilateral mandibular fractures)
- Hypoxia
- Hypercapnoea
- Hypocapnoea due to spontaneous hyperventilation
- Deteriorating GCS >2 point drop
- Ongoing seizure activity
Specific targets
- PO2 - 10 - 13 kPa
- PCO2 - 4.5 - 5 kPa
- EtCO2 - 4.0 - 4.5 kPa
- MAP - >90 mmHg
- CPP - >60 mmHg
- Na - 145 - 155 mmol/L
- Glucose - 6 - 10 mmol/L
- Avoid fever and avoid hypothermia
Airway concerns
- C-spine trauma (consider MILS)
- Avoid flexing and extending the neck wherever possible
- Facial trauma, bleeding and potentially soiled airway (blood, teeth)
- Skull fractures that may be worsened by manipulating the head
Breathing concerns
- Spontaneous hyperventilation
- Apnoea
- Concomittant chest trauma and traumatic pneumothorax
Circulatory concerns
- Major haemorrhage with or without DIC
- Huge catecholamine surge can cause myocardial ischaemia
- Hypertensive and tachycardic response to laryngoscopy can increase intracranial pressure
*Ketamine's slight increase in intracranial pressure is counteracted by the helpfulness of its ability to maintain cardiac output, so we use it in head trauma.
Here's why you don't use albumin.
In the ambulance
As the CT1 newly indoctrinated onto the on-call rota, one of your staple jobs is hopping into the back of the truck and accompanying your patient up to wherever the nearest neurosurgeon can be found.
Things to consider
You will not be able to intubate, cannulate or do anything useful sideways at 70 mph.
- Ensure your tube is taped and taped again
- Have enough access, with enough extensions, and enough flushes, so you can give drugs from your seat
- Have 3% hypertonic saline connected and ready to go, in case Cushing pays a visit on the motorway
A normal hospital bed isn't hopping over speedbumps, or flinging around roundabouts at questionably efficient speeds.
- Ambulances have terrible acceleration but fabulous brakes
- A sudden deceleration will send an enormous rush of blood into your patient's delicate head
- Ask the driver to prioritise being smooth over speedy and avoid heavy braking where possible
Remember the ultimate aim here - get to the neurosurgeon - when considering whether an unexpected emergency warrants pulling over or diverting to the nearest emergency deparment.
- If the patient's tube falls out 5 minutes from the destination, shove an IGEL in and crack on
- If they blow a tension pneumothorax an hour away, pull over and decompress with an orange cannula - if it improves, crack on, if not, head to the nearest ED
Keep your consultant's number handy for advice and remember:
"You are not responsible for the outcome, you are only responsible for your actions."
Trials and guidelines to be aware of
- CRASH-1 - steroids
- CRASH-2 - tranexamic acid
- NICE Guidelines CG 176
- DECRA Trial (2011)/ RESCUEicp Trial (2016) - decompressive craniectomy for refractory ICP
- SAFE-TBI Subgroup Analysis (2007) - albumin vs saline in severe TBI
- POLAR Trial (2018) - prophylactic hypothermia in severe TBI
- BEST-TRIP Trial (2012) - ICP monitoring guided therapy vs imaging/clinical
- APEX-TBI Study (Ongoing) - ketamine in TBI
- SYNAPSE Trial (2014) - ICP monitoring
- ROCKET Trial (2020) - tranexamic acid in TBI
- CONTROL Trial (2022) - early coagulopathy correction with fibrinogen and PCC
Useful Tweets and Resources
Jame Cory-Wright presents his poster titled: The hypotensive-response in patients with traumatic
— prehospitalcare (@FPHCEd) March 18, 2020
brain injury who underwent pre-hospital emergency anaesthesia by a Helicopter EmergencyMedical Service.
PHEA is a key component of early traumatic brain injury management. pic.twitter.com/o9oi3ALiL2
References and Further Reading
Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.


