Guillain-Barré Syndrome

Take home messages
- GBS is an acute ascending polyneuropathy that often follows an infection
- Treatment is supportive, ventilation, IVIG and plasmapheresis
- Watch out for autonomic instability, and monitor FVC when deciding whether to intubate
What is it?
If there's one thing that you'd really appreciate as a patient after a vicious few days of florid diarrhoea with or without vomiting, it's the delightful progressive ascending paralysis of Guillain-Barré.
- An acute demyelinating peripheral polyneuropathy
- Usually autoimmune in nature
- Commonly following respiratory of GI infection, particularly Campylobacter Jejuni
Some stats:
- The incidence of GBS is around 2 per 100,000 per year in the Western hemisphere
- Bimodal distribution of young and elderly
- Slightly more men than women
- 10% mortality - But this is usually due to the complications of the disease
- 10% have long term neurological complications
- Associated with some conditions such as Systemic Lupus Erythematosus, Sarcoidosis, Lymphoma
A bit of history
Jean-Baptiste Landry first documented the condition in 1859 as he noted an 'ascending paralysis'.
Barré and Strohl then noticed weakness and areflexia in French soldiers during World War I, who were then found to have CSF changes as well, with increased protein levels but normal cell counts.
In the 1970s there were a whole bunch of cases associated with vaccinations for swine flu leading to specific diagnostic criteria being developed.
- Plasma exchange was first used in 1978
- Intravenous immunoglobulins in 1988

The classical presentation
Ascending limb weakness with areflexia is the most common way that Guillain-Barré syndrome presents, particularly in textbooks, however as with everything in medicine, there are always variations.
A completely sensory type has also been described.
Suspicion should be raised if the patient describes a recent viral or diarrhoeal illness.
What are the types of GBS?
There are four main subtypes of Guillain-Barré:
Acute inflammatory demyelinating polyradiculoneuropathy (AIDP)
- Commonest form (80-90%)
- Symmetrical ascending weakness
- Areflexia
- Inflammation of axon myelin sheaths
Acute motor axonal neuropathy (AMAN)
- More common in Asia and young people
- Associated with Campylobacter
- Reflexes may be intact
- Antibodies bind to ganglioside antigens on axon membrane, leading to macrophage infiltration and inflammation
Acute motor and sensory axonal neuropathy (AMSAN)
- Motor and sensory involvement
- More severe, with longer or incomplete recovery
- Antibody-mediated damage to axons
Miller Fisher Syndrome
- Ataxia, areflexia and ophthalmoplegia
- 25% develop weakness of limbs
- 90% have antibodies to GQ1b
What actually happens?
- Demyelination of peripheral nerves and spinal roots
- Axonal degeneration in more severe cases
- Wallerian degeneration
- Periaxonal macrophages
How do you actually diagnose it?
According to the American Medical Association:
To make a formal diagnosis of GBS, two clinical criteria are required—progressive weakness in more than one limb and areflexia (or distal areflexia with proximal hyporeflexia)
The clinical diagnosis of GBS needs to be confirmed by cerebrospinal fluid analysis and nerve conduction studies. Lumbar puncture is indicated in every case of suspected GBS.
What blood tests would you perform in suspected GBS?
- Full blood count - for signs of infection
- Electrolytes and urinary sodium - SIADH is associated with GBS
- Urea and creatinine
- Liver function tests
- Clotting
- Calcium
Plasmapheresis requires normal clotting, and may worsen hypocalcaemia
- Positive anti-CD3 titre for diagnosis
- Specific antibodies to infective organism can also be tested
- Inflammatory markers
How to clinch the diagnosis
- Positive anti-CD3 titre
- Raised protein in CSF
- Nerve conduction studies
What else could it be?
How to classify the disease
When thinking about neuromuscular disorders in general, it's nice to classify them in a vaguely sensible way. One particularly sensible way is to do as follows:
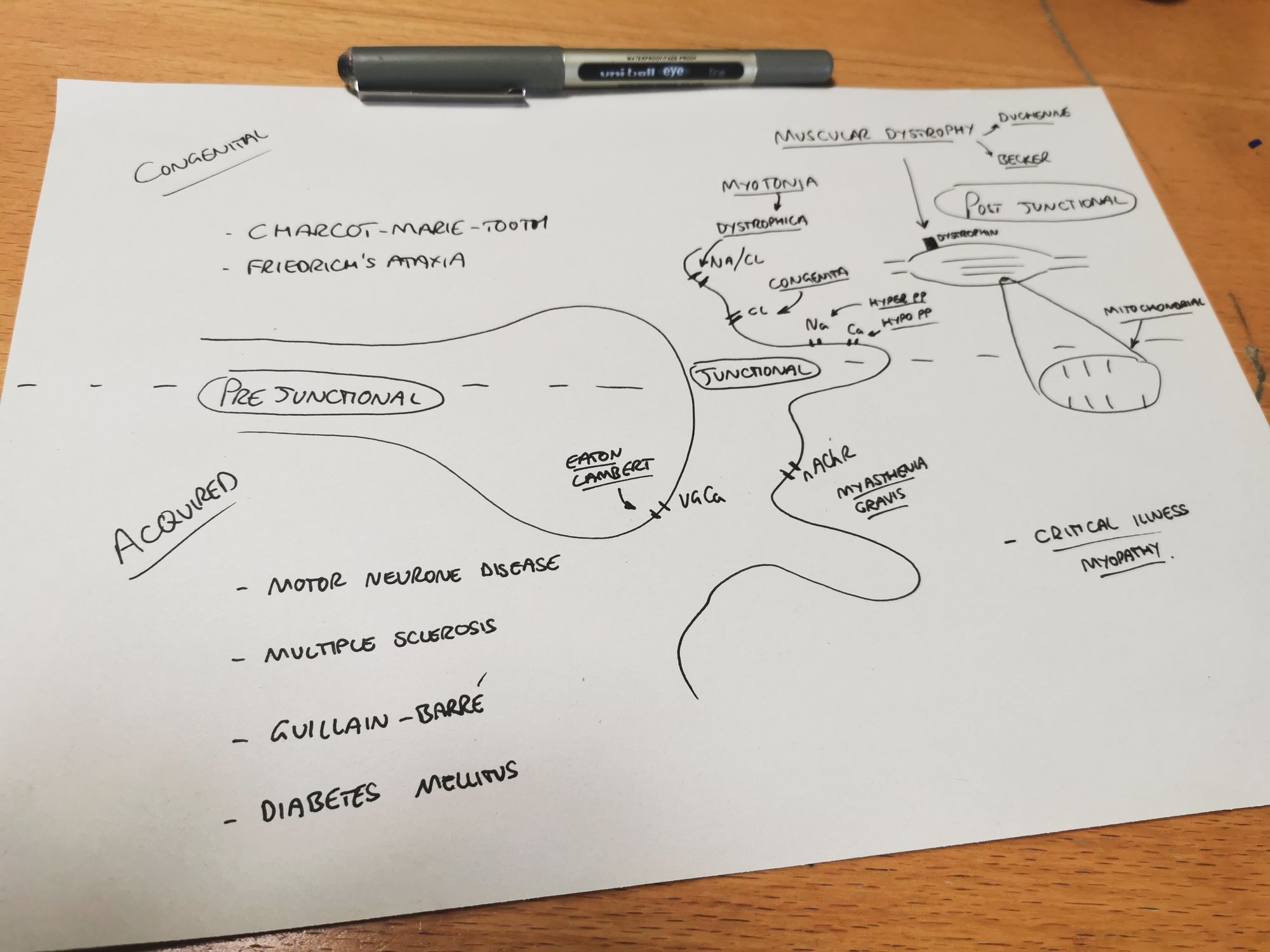
Acquired vs Congenital
Acquired
- Guillain-Barré
- Motorneurone disease
- Multiple sclerosis
- Diabetes Mellitus
- Critical illness neuropathy/myopathy
- Myasthenia Gravis
- Eaton-Lambert Syndrome
Congenital
- Charcot-Marie-Tooth
- Friedrich's ataxia
- Duchenne Muscular Dystrophy
- Becker's Muscular Dystrophy
- Myotonic Dystrophy
- Myotonia Congenita
- Hyperkalaemic Periodic Paralysis
- Hypokalaemic Periodic Paralysis
- Metabolic myopathy
- Mitochondrial dysfunction
Or alternatively, by location of the problem, be that pre-junctional, post-junctional, or at the neuromuscular junction itself (Junctional).
Location of problem
Pre-Junctional
- Charcot-Marie-Tooth
- Friedrich's ataxia
- Guillain-Barré
- Diabetes Mellitus
- Motor neurone disease
- Multiple sclerosis
Junctional
- Myasthenia Gravis
- Eaton-Lambert Syndrome
Note that there aren't any congenital junctional disorders (that you need to know about)
Post-Junctional
- All the muscular dystrophies
- Metabolic and mitochondrial disorders
- Critical illness myopathy
Differential diagnosis for acute weakness
This is clearly going to be broad, and can be categorised by system:
Neurological
- Myasthenia gravis
- Eaton-Lambert (myasthenic) syndrome
- Multiple sclerosis
- Transverse myelitis
Metabolic
- Hypokalaemic periodic paralysis
- Hypermagnesaemia
- Hypophosphataemia
- Acute intermittent porphyria
Infective
- Post diphtheria neuropathy
- Polio
- Botulism
- Tick paralysis
Drugs / toxins
- Heavy metal poisoning (e.g. lead)
- Biological toxins (including snake and scorpion toxins)
- Drugs (including stavudine, nitrofurantoin and aminoglycosides)
Other
- Acute polymyositis
- Critical illness myopathy
This is the suggested differential diagnosis as listed in the Tutorial of the Week - see below
How can we treat it?
Generally speaking, GBS is a self-limiting disease, and in itself doesn't usually cause all that much damage - it's the complications that cause the patient problems, including pressure sores, infections and respiratory failure.
The main priorities for treatement are:
- Supportive care and ventilation
- Physiotherapy
- Intravenous immunoglobulin (IVIG)
- Plasma exchange
- Corticosteroids should not be used as a therapy in GBS
What are the indications for IVIG or plasmapheresis?
- Patient unable to walk
- Respiratory failure
IVIG should be given as 0.4mg/kg once a day for 5-6 days, within 2 weeks of symptom onset
- Patients are often debilitated and hospitalised for many months
- Supportive therapy should take the form of a multidisciplinary approach involving medical and nursing staff, physiotherapists and occupational therapists.
- Because of the incidence of depression associated with GBS, psychiatric support and counselling services may be required for both patients and their families.
- 10% will not be able to walk unaided one year into their illness
- 25% will require ventilatory support
When should I intubate them?
What are the indications for intubation in GBS?
- Vital capacity less than 20ml per kilogram or decrease of >30%
- Maximal inspiratory pressure less than 30cmH2O
- Maximal expiratory pressure less than 40cmH2O
Autonomic dysfunction, facial and bulbar involvement and rapid progression of weakness make intubation more likely
Generally non invasive ventilation is avoided as it doesn't help clear secretions, and patients tend rapidly progress to needing intubation anyway.
Patients on the intensive care unit should be regularly re-assessed to ensure their weakness isn't progressing
Anaesthetic considerations
- Early elective intubation if evidence of rapidly worsening ascending muscle weakness
- Invasive blood pressure monitoring due to autonomic instability
- Avoid depolarising muscle relaxants
- Reduced dose of non-depolarising agents may be required
- Epidural anaesthesia can be useful to reduce opioid use if performing an operation
Don't forget the autonomics
It's not just skeletal muscle and sensory innervation that is affected in GBS. There can be profound autonomic symptoms that may cause you trouble as an anaesthetist.
What autonomic features can be seen in GBS?
- Labile blood pressure
- Tachycardia
- Arrhythmias
- Sweating
- Urinary retention
- Constipation
What ECG changes may be seen in GBS?
- Arrhythmias
- ST depression
- T wave inversion
- Prolonged QT interval
Why the 10% mortality?
As mentioned earlier, the main issues occur from the complications that develop as a result of GBS, rather than the disease process itself.
The commonest causes of death in patients suffering from GBS are:
- Sepsis
- ARDS
- Respiratory failure
- Pulmonary embolism
- Cardiac arrest due to arrhythmia or autonomic dysfunction
What are the complications associated with GBS?
- Pressure sores
- Contractures
- Peripheral nerve palsy
- Pneumonia
- Aspiration pneumonitis
- Psychological impact
- Neuropathic pain
- Venous thromboembolism
Useful Tweets and Resources
References and Further Reading


Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!