Pre-Eclampsia

Take home messages
- 25% of women with hypertension during pregnancy will develop pre-eclampsia
- The main aims of intervention are to prevent maternal intracranial haemorrhage and allow the pregnancy to continue to as close to term as possible
- The magic number to target is <135/85 mmHg
Pressure is bad
Well, too much pressure is bad - ideally we have just enough to perfuse all of the important bits, but not enough that they leak, occlude or explode.
- Hypertension in pregnancy is a risk factor for long term cardiovascular disease
- The uterus doesn't autoregulate
- We're trying to prevent intracranial haemorrhage in a patient with leaky blood vessels
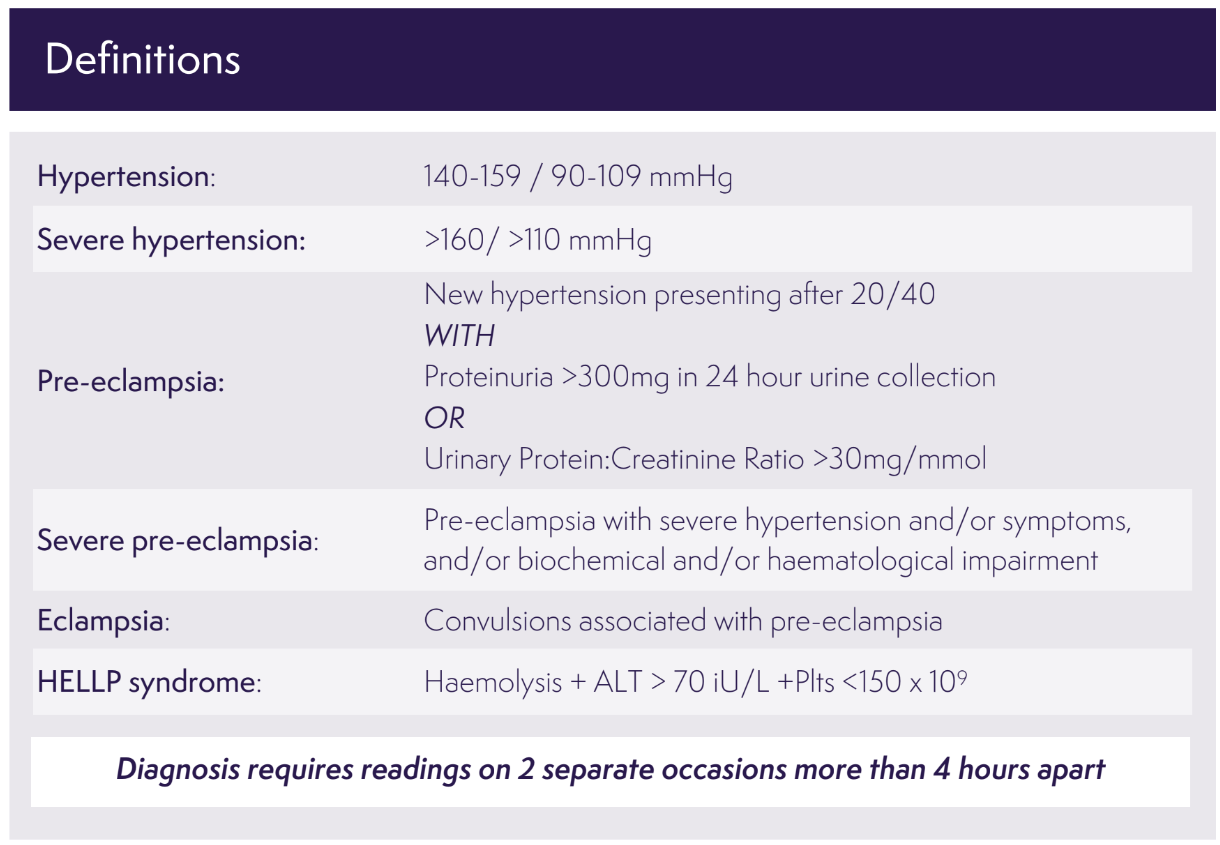
Some useful definitions
The key point in time to keep in mind is 20 weeks gestation - if hypertension is present before this, then it's not gestational, it's just hypertension. If it starts after 20 weeks, then it's gestational.
- Up to 1 in 20 parturients will already be hypertensive before pregnancy, and this number is increasing with increased rates of obesity and increasing average maternal age
- Around 6% of pregnancies will be affected by gestational hypertension
- The key in both of these cases is that there is no significant proteinuria - as soon as the kidneys start leaking protein, we're into pre-eclampsia territory
Gestational hypertension is diagnosed as new high blood pressure after 20 weeks of pregnancy. Therefore, if the blood pressure was there before (or they're already on antihypertensive meds), it's not gestational (aka Pregnancy induced hypertension PIH), rather it's simply chronic hypertension.
- In the UK between 2009 and 2012 it was the fourth most common cause of maternal death
Hypertension has a significant impact on the foetus
Increased risk of:
- Intra uterine foetal growth restriction
- Placental abruption
- Intrauterine death
- Preterm delivery
- Caesarean section
What do I do about it?
What can I use to bring blood pressure down?
- Labetalol - 100mg BD up to 500mg TDS
- Nifedipine - 10mg modified release BD up to 40mg BD
- Methyldopa - 250mg BD up to 1g TDS
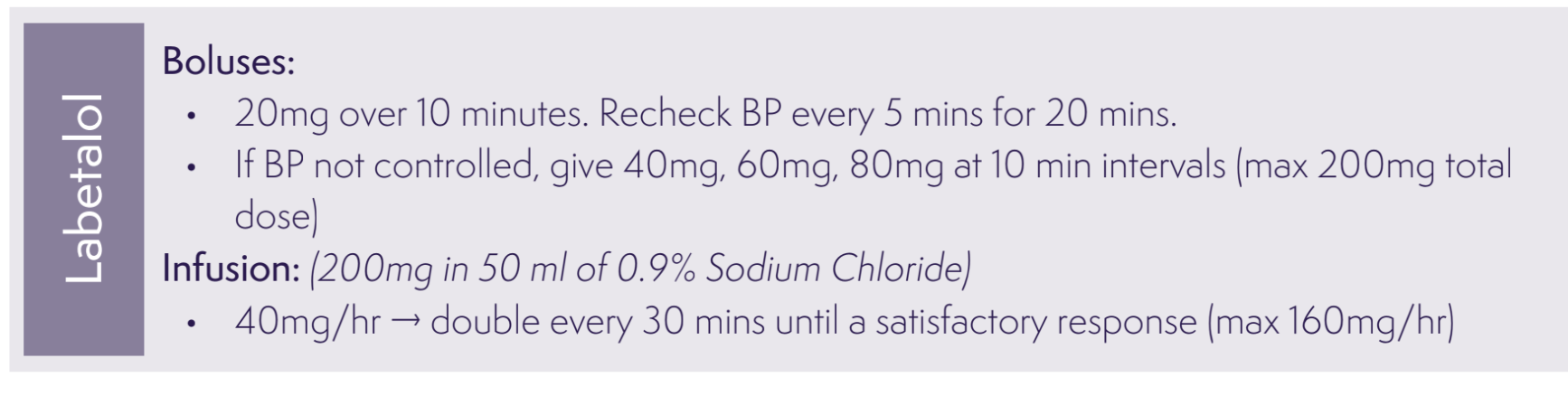
IV boluses
- Labetalol - 20mg IV over 10 minutes, repeated at 10 min intervals
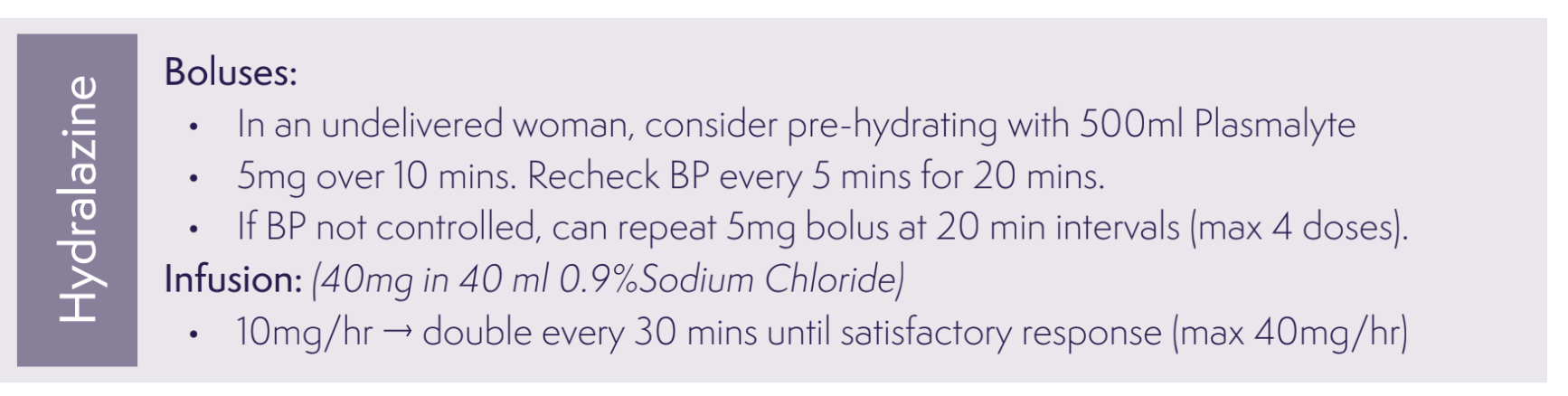
- Hydralazine - 5mg over 10 minutes, further 5mg at 20 mins
Infusions
- Labetalol - 40mg/hour up to 160mg/hour
- Hydralazine - 10mg/hour up to 40mg/hour
All are safe in breast feeding, just be cautious with labetalol and bad asthma - check how bad before giving them a beta blocker
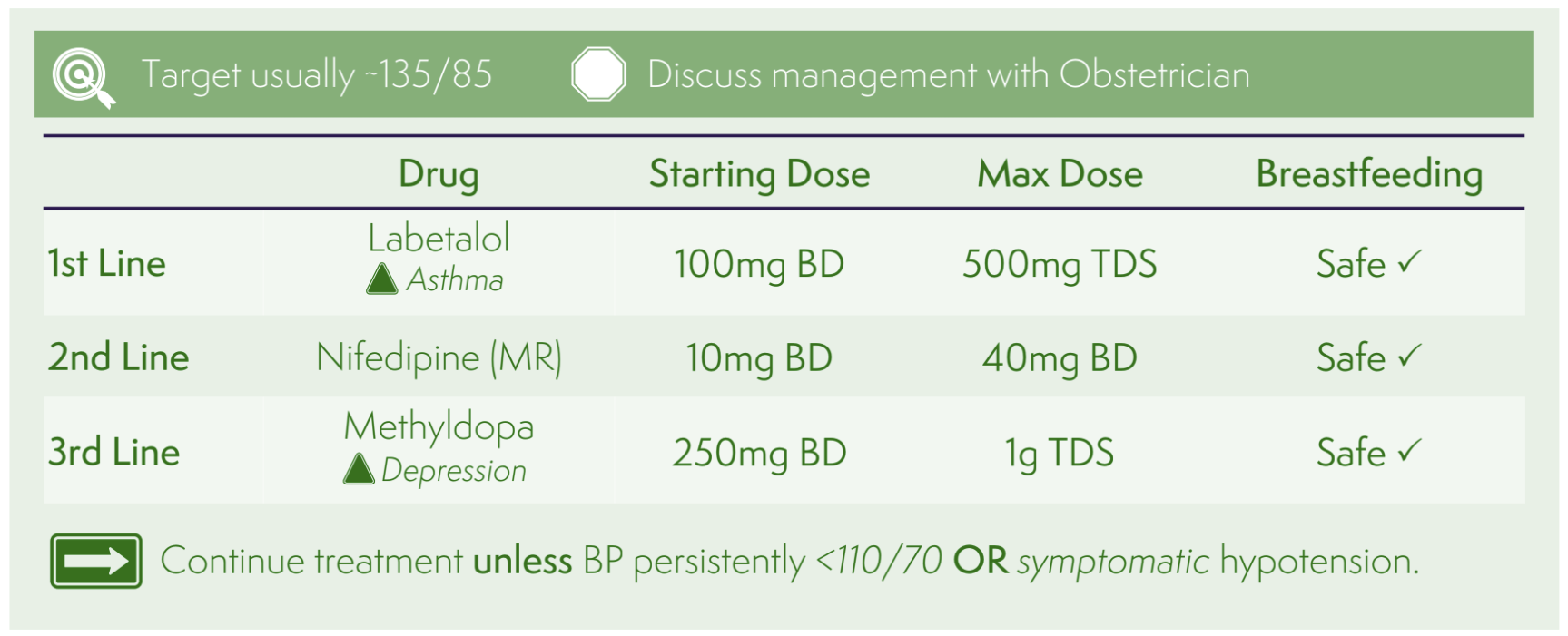
- But as with all things in physiology, try to avoid rapid changes in blood pressure, as this can do harm in equal measure - aim for around 1-2 mmHg per minute as a maximum rate of reduction
- Just be cautious if giving nifedipine and magnesium sulphate at the same time - the double whammy calcium antagonism can cause toxicity
- Hydralazine can cause sudden hypotension as well as a maternal tachycardia so a pre-emptive 500ml fluid bolus is usually a good idea
What is pre-eclampsia?
The generally accepted pathophysiological process goes a little something like this:
- Inadequate placental invastion of trophoblast cells of the spiral arteries, producing...
- High resistance blood vessels and compromised blood flow to the placenta, leading to...
- Abnormal placentation and endothelial dysfunction, vascular remodeling, therefore triggering...
- Activation of clotting cascade, microthrombi production and end organ dysfunction
Or something like that.
Essentially there is a microanatomical problem with the blood supply to the placenta, so it throws the toys out the pram and releases a whole host of spicy chemicals that cause endothelial dysfunction and organ damage.
And that's why you see proteniuria.
How much protein is proteinuria?
- Urine protein:creatinine ratio >30 mg/mmol or
- 24 hour urine collection of over 300mg protein
What is the definition of pre-eclampsia?
According to the International Society for the Study of Hypertension in Pregnancy (ISSHP)
- New onset hypertension > 140/90 (either or both)
Plus one or more of the following:
- Proteinuria*
- Other organ dysfunction:
- Liver, kidney, neurological
At or after 20 weeks gestation
*Defined as a urinary protein:creatinine ratio of >30mg/mmol or albumin:creatinine ratio >8 mg/mmol
Other organ dysfunction is defined by:
Renal dysfunction
- An increase in serum creatinine of >90 μmol/litre
Liver dysfunction
- Elevated AST or ALT >70 IU/litre
- or double upper limit of normal
Neurological dysfunction
- Seizures
- Severe headaches
- Scotoma or blindness
- Clonus
- Altered mental status
- Stroke
Haematological dysfunction
- Thrombocytopaenia (<150)
- Haemolysis
- Disseminated intravascular coagulation
Uteroplacental dysfunction
- Abnormal Dopplers
- Foetal growth restriction
- Stillbirth
How bad does it get?
2% of maternal deaths are attributable to eclampsia and pre-eclampsia
As with most disease processes it lies on a spectrum, depending on how high the blood pressure and the extent of end organ dysfunction.
Features of severe pre-eclampsia
- Systolic >160 mmHg
- Diastolic > 110 mmHg
- Pulmonary oedema
- New severe unexplained headache
- Visual disturbance
- Vomiting
- Subcostal pain
- Papilloedema
- Clonus of more than 3 beats
- Liver capsule tenderness
- Thrombocytopenia (defined as less than 100)
- Deranged ALT or AST (more than 70)
- Renal dysfunction
- Evidence of haemolysis
Who gets it?
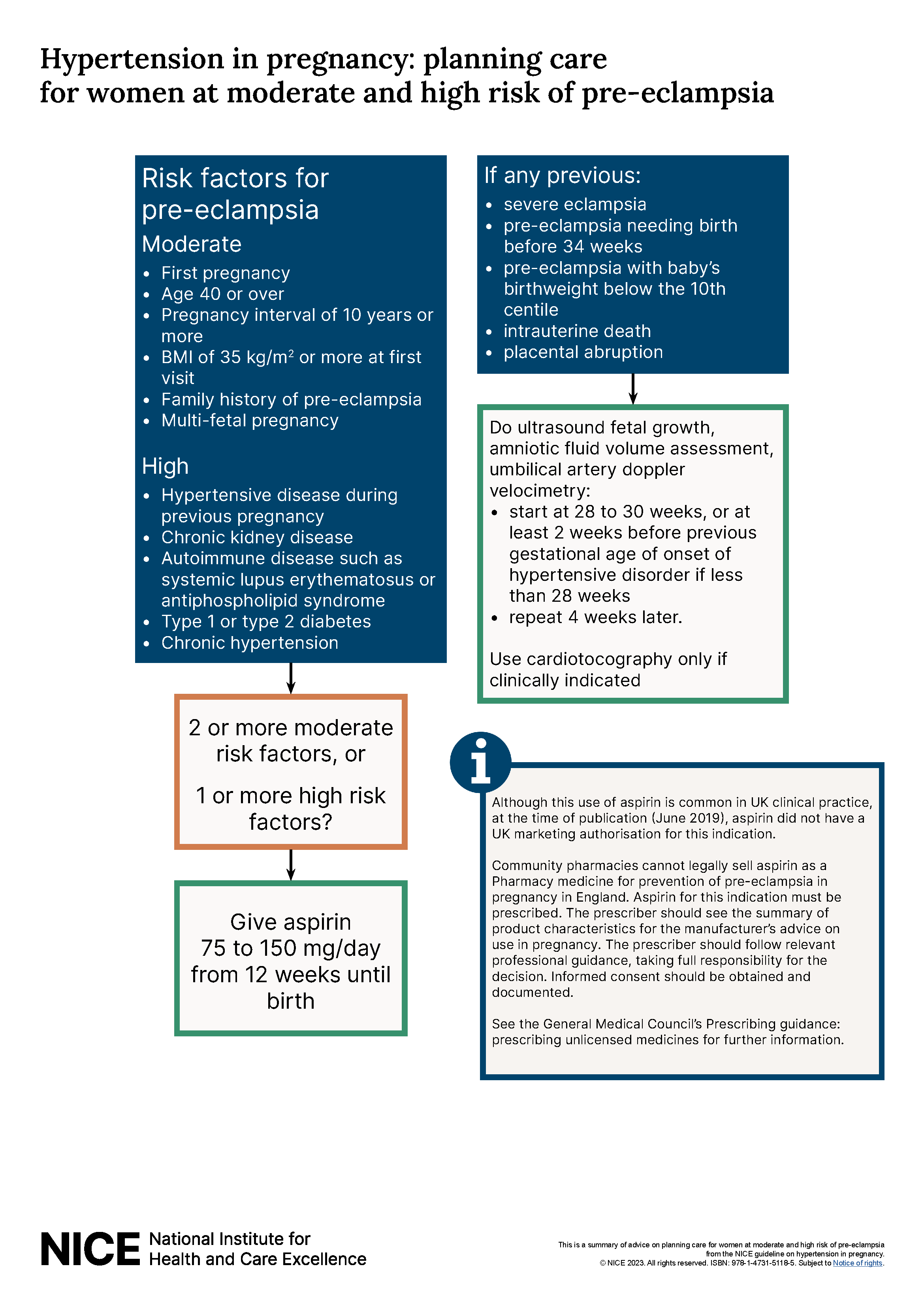
Risk factors for pre-eclampsia
Moderate risk factors:
- First baby, or first baby in ten years
- Multiple pregnancy
- Maternal age over 40
- BMI over 35
- Family history of pre-eclampsia
High risk factors:
- Previous pre-eclampsia*
- Diabetes
- Hypertension
- Renal disease
- Antiphospholipid syndrome
*This sounds like a cop-out answer but it will get you marks in the exam!
Can we test for it?
- Placental growth factor is produced by the placenta and peaks between 26 and 30 weeks
- Levels are thought to be lower in women with pre-eclampsia, and the lower the level, the more severe the case
- This can be detected before the onset of measurable hypertension or proteinuria
It's exciting, but there isn't sufficient RCT evidence to support its routine use in diagnosing pre-eclampsia just yet.
Timing of birth
If there are features of severe pre-eclampsia then a planned delivery before 37 weeks needs to be considered.
Why are they all on Aspirin?
- NICE recommends that women at high risk of developing pre-eclampsia be given aspirin 75–150 mg daily from 12 weeks until the birth of the baby (50% relative risk reduction in high risk women)
- Women with two or more moderate risk factors should also be offered aspirin
- Aspirin alone does not contraindicate neuraxial blockade
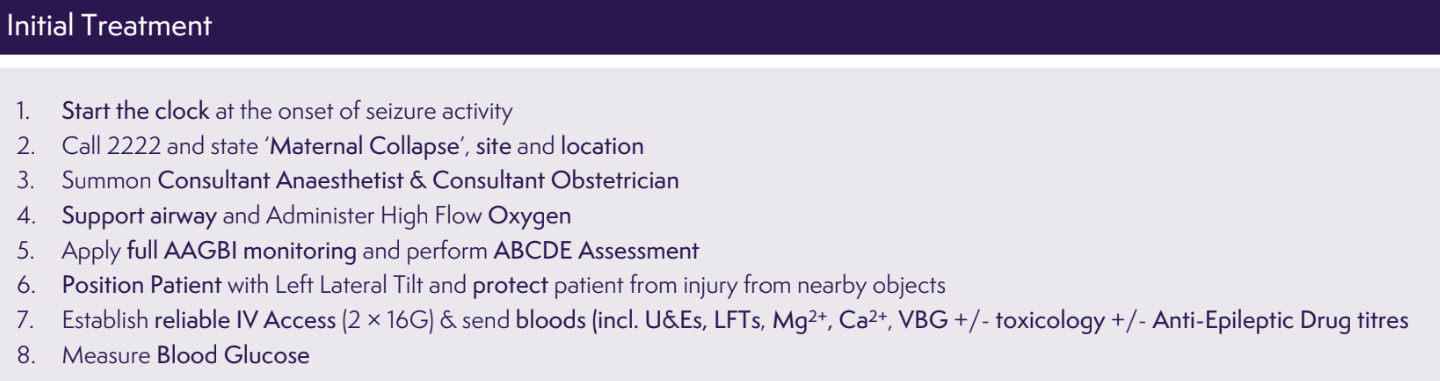
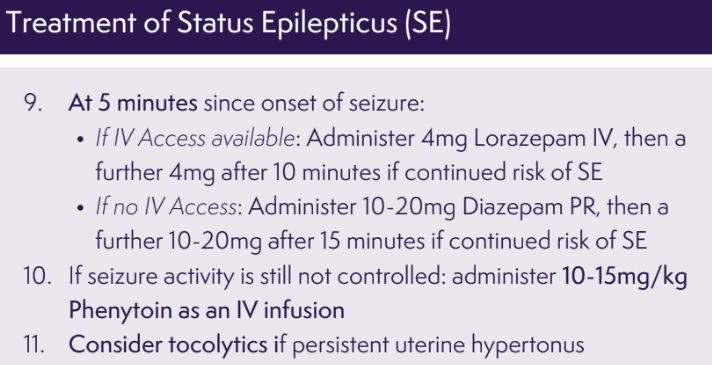
If they seize
It's now eclampsia, which carries risk of cardiac arrest and intracerebral haemorrhage.
Seizures are ridiculously terrifying for a pathology that usually doesn't do much harm and self resolves in a matter of minutes. Eclamptic seizures are the same, but remember that during the seizure there is a risk of aspiration due to an unprotected airway, as well as a surge in blood pressure in a patient already at high risk of stroke.
Once you go from pre-eclampsia to eclampsia the risk of stroke increases tenfold.
- Between 1 and 2% of pre-eclamptic mothers will have a seizure and therefore develop eclampsia
- The seizures are throught to be caused by cerebral vasospasm
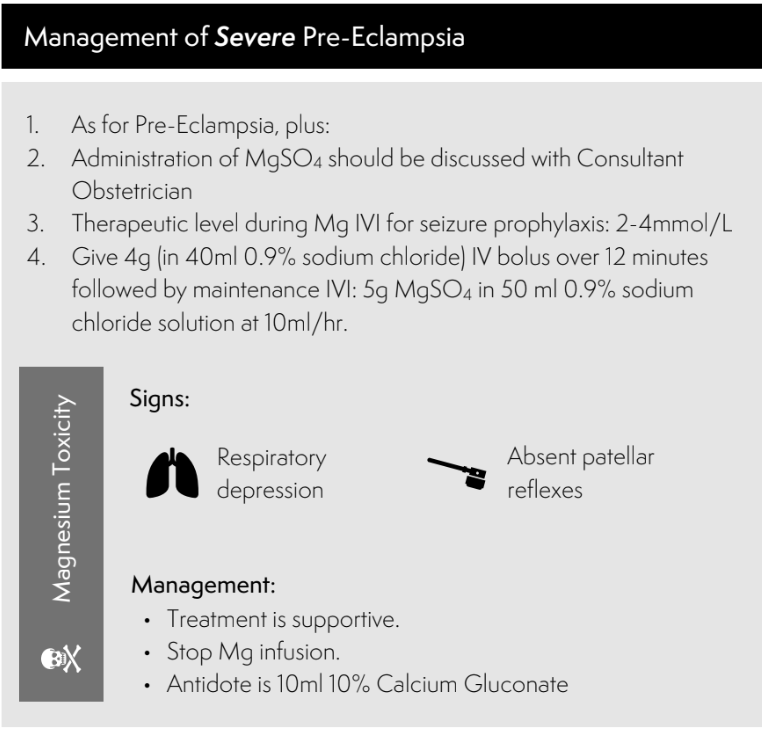
- Magnesium is believed to induce cerebral vasodilatation and therefore prevent seizures from occurring
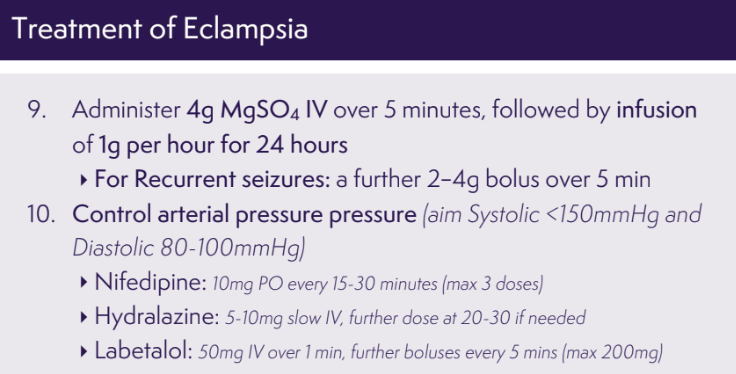
Magnesium sulphate is both treatment and prevention of seizures in eclampsia
4 g over 5 min
followed by an infusion of 1 g per hour for 24 h
If they seize again, then further 2g magnesium boluses can help.
HELLP
Haemolysis, elevated liver enzymes and low platelets.
This is pre-eclampsia-gone-bad and carries substantial morbidity and mortality for the mother and baby, affecting around 1 in every 10 000 pregnancies
- AST or ALT or GGT >70
- Platelets <100
- Lactate dehydrogenase >600 or bilirubin >20
What conditions are associated with HELLP syndrome?
- Placental abruption
- Hepatic haemorrhage or infarction
But note that if the clotting is deranged or the platelet count is rapidly falling then you might find yourself avoiding the spine altogether, and don't forget the magnesium.
How should I anaesthestise a woman with pre-eclampsia?
Carefully, and ideally with some sort of neuraxial blockade to help lower blood pressure, allow neurological monitoring to continue and avoid the issues with general anaesthesia.
Regional is plan A
Most of the time in the world of obstetric anaesthesia, the safest and preferred way to proceed is with some sort of regional - usually neuraxial - blockade.
The same applies in hypertension and pre-eclampsia.
There are several benefits to regional anaesthesia in the pre-eclamptic parturient, aside from the boring answer of 'avoids risks associated with GA':
- Better pain control
- Reduces blood pressure
- Allows ongoing monitoring of neurological status
- Avoids potentially dangerous hypertensive response to laryngoscopy
Women with high blood pressure in labour are generally advised to at least consider epidural analgesia, for all of its wonderful analgesic and antihypertensive properties, as well has having an anaesthetic option in place already should you need to go to theatre.
Reasons to go for GA
- Patient refusal of regional anaesthesia
- Regional anaesthesia contraindicated
- Low GCS
- Pulmonary oedema and hypoxia
- Recurrent or uncontrolled seizures
Things to think about when performing general anaesthesia
- Unfasted patient - omeprazole, metoclopramide, citrate
- Difficult intubation - videoscope, THRIVE
- Higher risk of aspiration - ramped position, oxford pillow, cricoid if you like it
- Need to maintain steady blood pressure - pressors and labetalol at the ready
- Need to minimise laryngeal stress response to laryngoscopy
Probably best to avoid NSAIDs given potential renal and platelet issues. Paracetamol is very unlikely to cause any issues but may be witheld in the case of severely deranged liver function.
General anaesthesia carries its risks of airway issues with an oedematous larynx, hypertensive response to laryngoscopy and therefore risk of intracranial haemorrhage.
If you have to do a GA, then use a smaller tube than usual and remember you'll likely need to use hefty doses of rapid-acting opioids to suppress the response to the laryngoscope, such as:
- Alfentanil 25 microgram/kg
- Remifentanil 1 microgram/kg
And you may need esmolol 500 microgram/kg or labetalol 0.25mg/kg as well to help keep the pressure under wraps.
Try and keep the MAP below 65 and 110 mmHg and continue the magnesium infusion if its already running.
The treatment for magnesium toxicity is 10 ml 10% calcium gluconate.
If a patient's blood pressure is already of concern and they're receiving infusions of magnesium or labetalol, then an arterial line is probably a good idea.
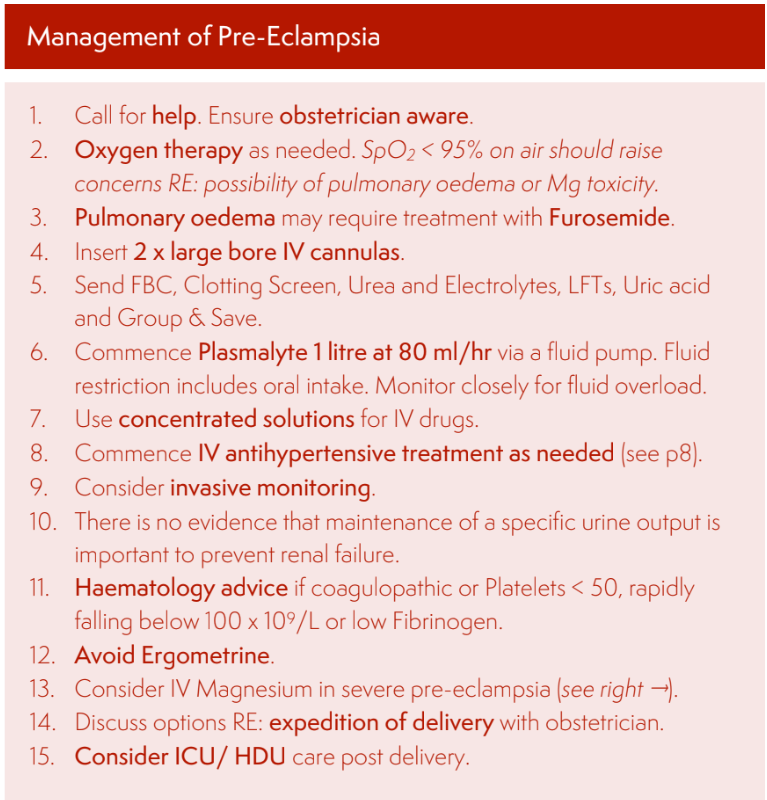
If in doubt, dry them out
Be very cautious with maintenance fluids in patients with pre-eclampsia.
Why fluids are tricky business:
- The patient is often hugely vasoconstricted as part of the underlying pathology, meaning they can tank their blood pressure the minute you give them an antihypertensive
- They then have increasingly leaky capillaries and hypoalbuminaemia, producing a higher tendency towards pulmonary oedema
- Thankfully, while transient AKI is rather common, long term renal impairment is very rare
If you have a severely pre-eclamptic patient, then the risk of pulmonary oedema and its associated complications are more likely to cause problems than short-term dehydration.
You can always give a fluid bolus if required later.
Why do we fluid restric pre-eclamptic patients?
- Up to 3% will get pulmonary oedema, usually after delivery of the baby
- 80 ml/hour is fairly standard as a total fluid allowance
- Furosemide boluses can be given if you are suspecting fluid overload
- GTN can also be considered in severe cases
Once baby is out
It's generally accepted, and usually the case, that hypertensive disorders of pregnancy resolve fairly rapidly after the baby and placenta are no longer in situ to cause the problem, however this shouldn't be taken as a given.
- Up to 44% of women with severe pre-eclampsia are at risk of post partum seizures
- Fluid balance, blood pressure management and normal biochemical parameters should all be diligently observed and corrected especially in the first 24 hours
- Pre-eclampsia is an independent risk factor for post partum haemorrhage so keep your wits about you
A Free Final FRCA CRQ
Our wonderful colleagues over at FRCA-revision.com have put together a whole host of high yield and syllabus-mapped CRQs, free of charge. We highly recommend you check out their site and interactive MCQ quiz!
The link below will take you straight to their high-yield question on pre-eclampsia
Final FRCA CRQ: Pre-Eclampsia
Useful Tweets and Resources

1/
— Casey Albin, MD (@caseyalbin) October 2, 2023
A 21 yo G1P0 reports a severe headache 3 days after delivery.
BP 182/100😱
While waiting to be admitted, she vomits & has a generalized tonic clonic seizure.
She is sedated and intubated for eclampsia.
The next morning, she has blown pupils.
A #continuumcase. @LyellJ pic.twitter.com/K8r2hMFzh8
#Esrasunny23 Platelet count for epidural placement in pre-eclampsia .. 70 is the new 80! @SOAPHQ Guidelines @DevroeSarah pic.twitter.com/feVkIUm8NX
— John Loughrey (@LoughreyJPR) October 5, 2023
References and Further Reading


Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.


