Dural Tap

Let it flow
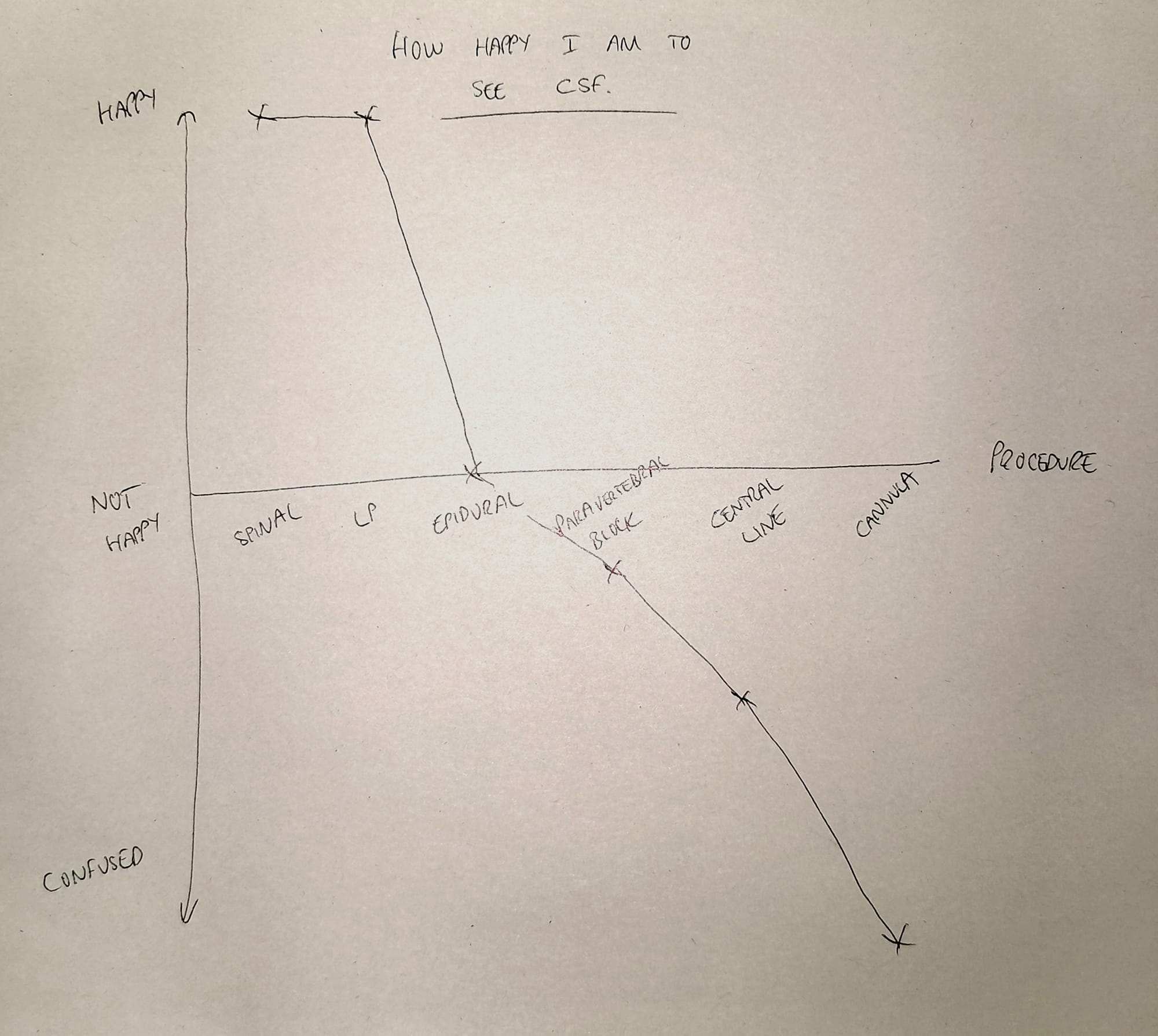
How one feels as an anaesthetist, upon witnessing the etherial gin-clear brain juice trickling from the end of one's needle, is highly variable depending on several factors:
- What procedure we were trying to do
- What needle we were using
- What the patient's actual problem is
For example
- Spinal, 25 gauge pencil point needle, knee replacement - elated
- Epidural, Tuohy, Labour - not so much
- Femoral vascath, introducer cannula, renal failure - confused
It happens
"If you haven't had a complication, you've not done the procedure enough."
I experienced my first accidental dural puncture on my fourth ever epidural, clocking up an impressive (and fortunately temporary) 25% tap rate.
And of course it had to happen on a day when I'd also already failed every spinal and cannula up until that point.
Sigh.
My learning points from this experience
- These things happen, you're not immediately a terrible anaesthetist
- It's generally very obvious when you've put a Tuohy needle into the subarachnoid space
- A dural puncture doesn't guarantee a headache
- Make sure you occlude the needle while you figure out what to do next
The physics
The CSF that supports and nourishes the brain, produced at a rate of around 150ml per day, will leak out if you stab a hole in the dura and arachnoid mater that contain it in the spinal canal.
No surprises there.
If enough fluid drains out - faster than it can be replaced by the choroid plexus - then the intracranial pressure drops, the weight of the brain starts to sag downwards, and pull on the meninges attaching it to the periosteum in the skull.
This can then lead to a rather stonking positional headache, which you can read all about here:
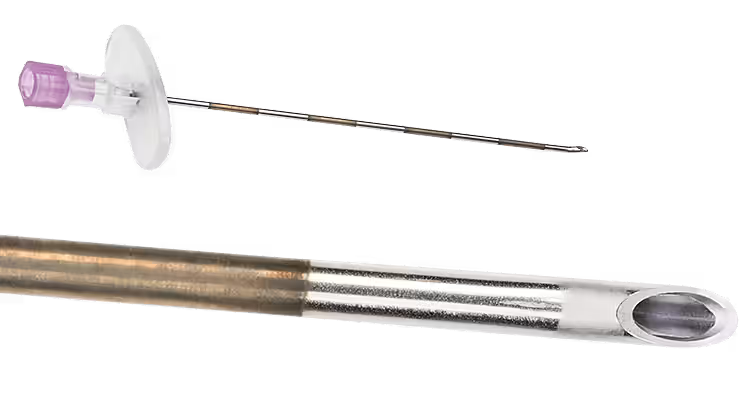
This can be achieved with:
- A spinal needle (deliberately)
- A Tuohy needle (accidentally)
- An epidural catheter (also accidentally)
When spinal anaesthesia is performed with a non-cutting, small gauge spinal needle, the hole is usually occluded fairly effectively by the dural fibres returning to their original position, and a headache avoided.
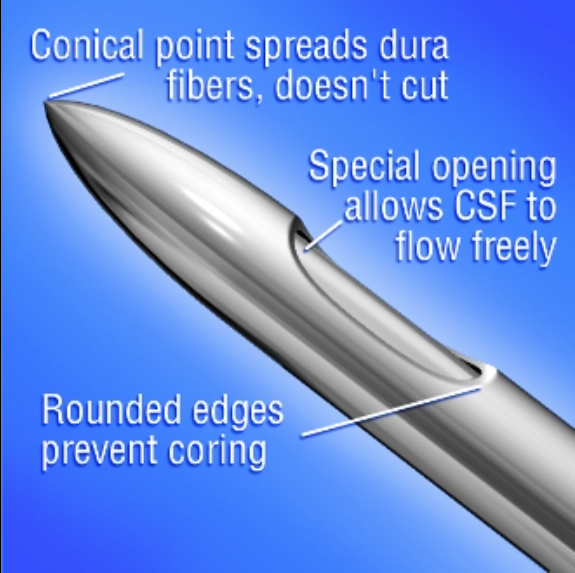
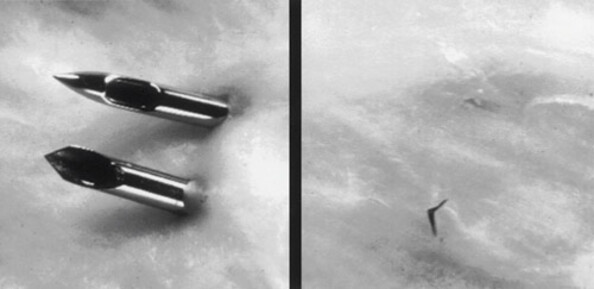
However a cutting needle, or a larger implement (such as a 16G Tuohy or epidural catheter) will usually leave a magnificently persistent hole that then permits continued leakage of fluid for the next few days, especially in an upright position.
What to do
When you notice the brain juice glubbing forth from the end of your Tuohy needle, it is entirely normal to feel a sense of impending doom trickle down your spine.
The deed is done, the key is what to do next.
- Don't panic
- Occlude the needle
- Consider giving a few mls of saline to replace the lost CSF
- Decide on your next step
- Talk to the patient, midwife and your assistant if you have one
Your options
- Give up (on the procedure, or on your career in general)
- Re-site the epidural a space higher*
- Insert an intrathecal catheter**
*Generally a good idea to avoid going a space lower, because your needle's Huber tip will direct the catheter upwards, towards the hole you've just made.
**Same catheter as epidural, just in a different place.
Intrathecal catheter?
One of your options when your Tuohy has gone swimming is to insert an intrathecal catheter.
This is not as crazy as it may seem, and is a widely-practised technique in other institutions around the world with spectacular success.
It's just not done very often for analgesia on labour ward.
Yes, that is a nasogastric tube in the spinal cord pic.twitter.com/Guo4KSmkSX
— Medlife Crisis (DEFUNCT) (@MedCrisis) June 22, 2019
While technically this is an intrathecal catheter, it's not the route we would advise.
When deciding to insert an intrathecal catheter
- Consider whether it's going to cause you more anxiety than benefit
- Is labour ward so busy that having this extra cognitive burden is going make life difficult?
- Have you got multiple other epidurals running, that might make you forget which one is the spinal catheter in a category 1 emergency?
- Are you near the end of your shift?
- Will you have time to keep coming back and regularly providing small top up doses during labour?
- How difficult is it going to be to just try another epidural instead?
- If the epidural felt easy enough, but the catheter just happened to find its way into the CSF, it's almost certainly a better plan to resite the epidural, because you don't know how many of the epidural catheter holes are within the subarachnoid space
Inserting an intrathecal catheter does not decrease the incidence of PDPH but does decrease the need for epidural blood patch.
If you do site an intrathecal catheter
- Warn the woman they will get a sharp shooting sensation when you insert the catheter
- Leave around 2-3cm of catheter in the spinal canal
- Do not connect to an epidural pump
- Do tape it up in a different way to normal, to give yourself a reminder that this one is different
- Do not let anyone else touch it
- Do not forget which of the seven epidurals you've sited this shift is actually a spinal catheter
- There is no benefit in terms of headaches and complications to leaving the catheter in for 24 hours after delivery
- In patients with an intrathecal catheter, injection of intrathecal saline prior to removal decreases the incidence of PDPH and the need for epidural blood patch
In theory you now have guaranteed spinal access in the case of an emergency caesarean section.
This will allow you to confirm there is (or is not) CSF aspirating back into your syringe, and may be the last slice of human factor cheese that prevents you plunging 20 mls of ropivacaine into the medulla.
What to give for surgery
The time has come, your patient needs a Caesarean section or removal of placenta, and you have put in an intrathecal catheter.
What to do?
- If you have time, give incremental doses of 0.2-0.5 ml 0.5% bupivacaine (or equivalent) through the catheter*
- Check the sensory level and continue topping up until you reach the desired level
- This can take up to 10 minutes, so be patient
- In a category 1 emergency, a larger dose of 1 - 1.5 ml can be given as an initial bolus
- Then you can give your opioid dose as usual
- Don't give a total dose of more than you would give as a spinal dose
All being well, the beauty of this set up is that you can give top up doses during surgery if it's not quite enough.
*Note that the dead space of the catheter is approximately 0.6 - 1ml.
Human factors
The disaster scenario that you're trying to avoid here is a labouring mother being given an epidural dose of local anaesthetic through a spinal catheter.
No matter how careful you are as an individual, there are numerous factors at play that make this possibility more likely:
- General unfamiliarity of anaesthetists with intrathecal catheters
- Muscle memory of administering epidural drugs in an emergency
- Cognitive load of a sudden requirement for emergency anaesthesia in a labouring mother
- Institutional muscle memory of using epidural pumps
- The catheter looks exactly the same from the outside
- The connectors are the same, so having NRFit or equivalent won't save you
Our take
This bit is not advice or instruction, and should not be used to guide your clinical decision making in a professional capacity - it remains you and your team's responsibility to determine whether or not the patient in front of you would benefit from an intrathecal catheter, or trying another epidural, or something else.
Consider the following scenario:
- I am at the beginning of my shift
- I'm the only obstetric-competent anaesthetist on site
- There are a full complement of experienced midwives
- And no other epidurals running
- I've just spent an hour trying and failing to find the epidural space
- In a very high BMI mallampati 3 parturient having her second baby
- Who is in agony at 7-8 cm
I finally feel that delicious loss of resistance, but remove the syringe to see CSF trickling back at me.
This is one time I would consider an intrathecal catheter.
My logic
In an ideal world, this scenario shouldn't happen, because ideally we're encouraging high risk BMI patients toward an early epidural, precisely to avoid this issue.
However, here we are, and so here's my thought process:
- I most likely don't have time to call a colleague to come in and have a go at an epidural
- If this woman goes for an emergency section, I really don't want to have to do a GA
- I've proven to myself that I will struggle to find the spinal space in an emergency
- The risk of me puncturing her dura again if I try another epidural is rather high
- It's the start of my shift, and this woman is likely to progress fairly quickly, meaning I shouldn't be needing to hand over the catheter to my colleague at the end of my shift
- There are no other epidurals running, so I'm able to focus my attention on the new kid on the block
- I have experienced midwifery colleagues who can help me manage the catheter safely
For me, the benefit of having what is hopefully guaranteed spinal access would likely outweigh the stress of having to manage an intrathecal catheter in this scenario.
What people really think
I asked around my colleagues (in a few busy DGHs, not a specialist obstetrics unit) what their thoughts were:
- "It's an infrastructure problem - if the midwives aren't used to it, then it's messy and risky"
- "I'd just resite it mate, you've found the epidural space once, you can do it again"
- "It's very labour (lol) intensive - you're constantly being asked to go back and top their block up"
- "It didn't top up how you'd expect - I ended up having to take it out and just do a spinal again anyway"
- "You probably just want to do it on a case-by-case basis. If it was super tricky to get in, and you think you'd really struggle to get a spinal or another epidural in, then it might be worthwhile"
- "It causes you a lot of anxiety, you just spend the whole shift worrying about it"
- "I've only done one and it worked, so I'd certainly consider it again in the right scenario"
What not to do
In summary
- Intrathecal catheters are not a completely insane idea
- You need to choose your patient cohort very carefully
- The infrastructure of where you are working will weigh heavily into your decision
- Decide if the anxiety is outweighed by the benefit of having semi-guaranteed spinal access
Related posts and references
Accidental dural puncture
— 𝘈𝘯𝘢𝘦𝘴𝘵𝘩𝘦𝘴𝘪𝘢 (@Anaes_Journal) September 30, 2024
• Inserting an intrathecal catheter does not decrease the incidence of PDPH but does decrease the need for epidural blood patch.
• There is no benefit in leaving the catheter in for 24 h postpartum.
• In patients with an intrathecal catheter,… pic.twitter.com/OJ37FRczI0
🔐Intrathecal catheter use after accidental dural puncture in obstetric patients: literature review and clinical management recommendations.
— 𝘈𝘯𝘢𝘦𝘴𝘵𝘩𝘦𝘴𝘪𝘢 (@Anaes_Journal) July 20, 2021
This great new narrative review is essential reading for all and #FreeForAWeek!
🔗https://t.co/NrPJi1ibkS pic.twitter.com/dFEPWj3E0g

Unrelated but interesting
It took this metal hook 23 years to make its way through the dura resulting in a CSF leak with intractable orthostatic headaches and brain sagging @isscl @spinalCSFleak @SRS_org pic.twitter.com/6mMjQIkMdz
— WouterSchievink (@WouterSchievink) March 7, 2025
Conus medullaris and cauda equina delicate structures of neurosurgical emergencies - ventral view.
— Neurosurgical Anatomy (@NeurosurgA) August 16, 2022
Supplied by the artery of Adamkiewicz - visible not injected on the left.#spine #caudaequina #spinalcord #neurosurgery pic.twitter.com/y5kzBwlb1t
Coffee?