Carotid Endarterectomy
Take home messages
- Carotid endarterectomy is indicated where carotid artery stenosis exceeds 70%
- CEA should be performed within two weeks of TIA symptoms and ideally 48 hours
- Anaesthesia can be regional or general, with regional providing better cardiovascular stability
- Complications include cerebral hyperperfusion syndrome
Let it flow
It's not complicated - we like blood to flow - and so if there's a blocked vessel to an important organ such as - oh I don't know, the brain - then it's probably a sensible idea to unblock it.
A patient presenting with a TIA or minor stroke is at supremely high risk of doing the same again but worse in the very near future, (highest risk at 72h) hence we try to crack on and get CEAs done within two weeks of the original presentation, and within forty-eight hours where possible.
The UK sees more than 130 000 strokes per year, and CEA is intended as a preventative procedure to reduce this number as much as possible.
You really need at least 70% stenosis of the carotid artery before you will see a substantial benefit of prophylactic surgery over best medical management.
What are the medical management options to reduce the risk of stroke?
- Blood pressure control
- Antiplatelet agents
- Statins
- Diet improvement
- Stopping smoking
- Minimising alcohol intake
Standard stuff really. You can list these bullet points for any cardiovascular condition if you're in a pinch in a viva.
A spot of History
Meet Dr. Michael DeBakey, Lebanese-American cardiac and vascular surgeon extraordinaire.
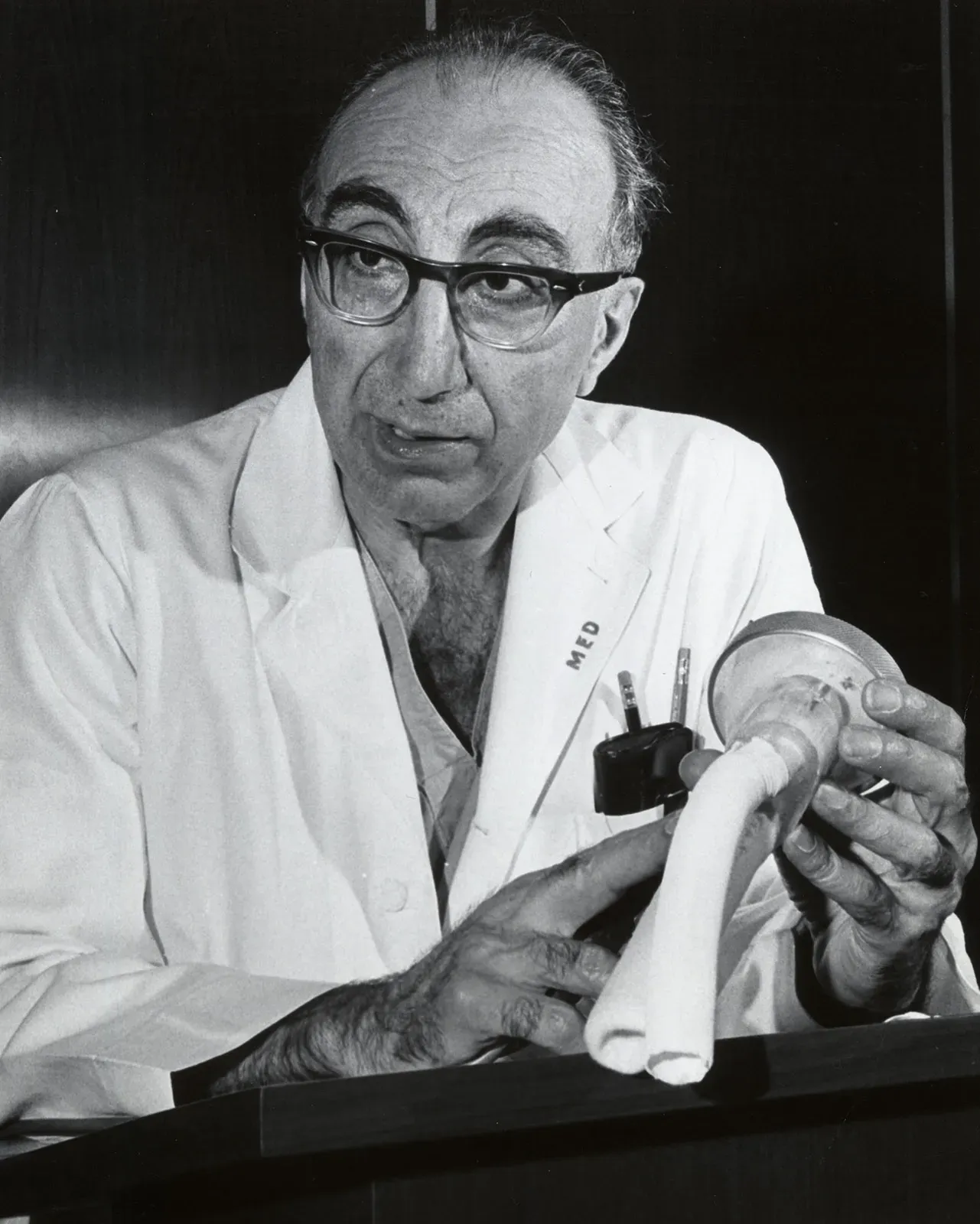
Amongst other minor and low-stress day to day activities such as aortic aneurysm repair, cardiac bypass operations and developing some of the first ventricular assist devices, he is also credited with having performed the first successful carotid endarterectomy in 1953.
Apparently he enjoyed his job so much he continued working until the age of 99 and in his more youthful years he enjoyed sewing, playing the saxaphone, reading and winning awards for growing vegetables in his garden.
Ironically he most likely would not have scored highly enough to secure a surgical training number in 2023.
What actually happens
There are many ways to skin a carotid.
The general steps:
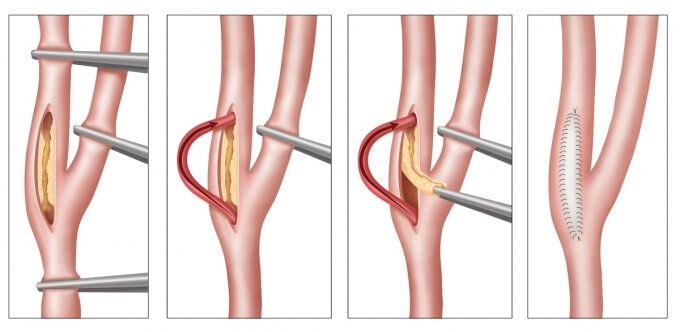
- Exposure and cross-clamping of the carotid artery proximal and distal to the offending stenotic area
- Longitudinal incision through diseased area and scrape out the bad bits
- Hopefully close it back up again, either with a patch (autologous or synthetic vein graft) or primary closure
- A patch usually reduces the likelihood of the stenosis reforming
- Sometimes they use a temporary shunt as shown in the image above
You might be thinking that clamping the main artery to the brain may cause some issues, and you'd be right, especially in someone whose brain has recently taken an ischaemic insult already.
Fortunately we have this little chap to keep us in business while the roadworks on the haematological highway are in progress.
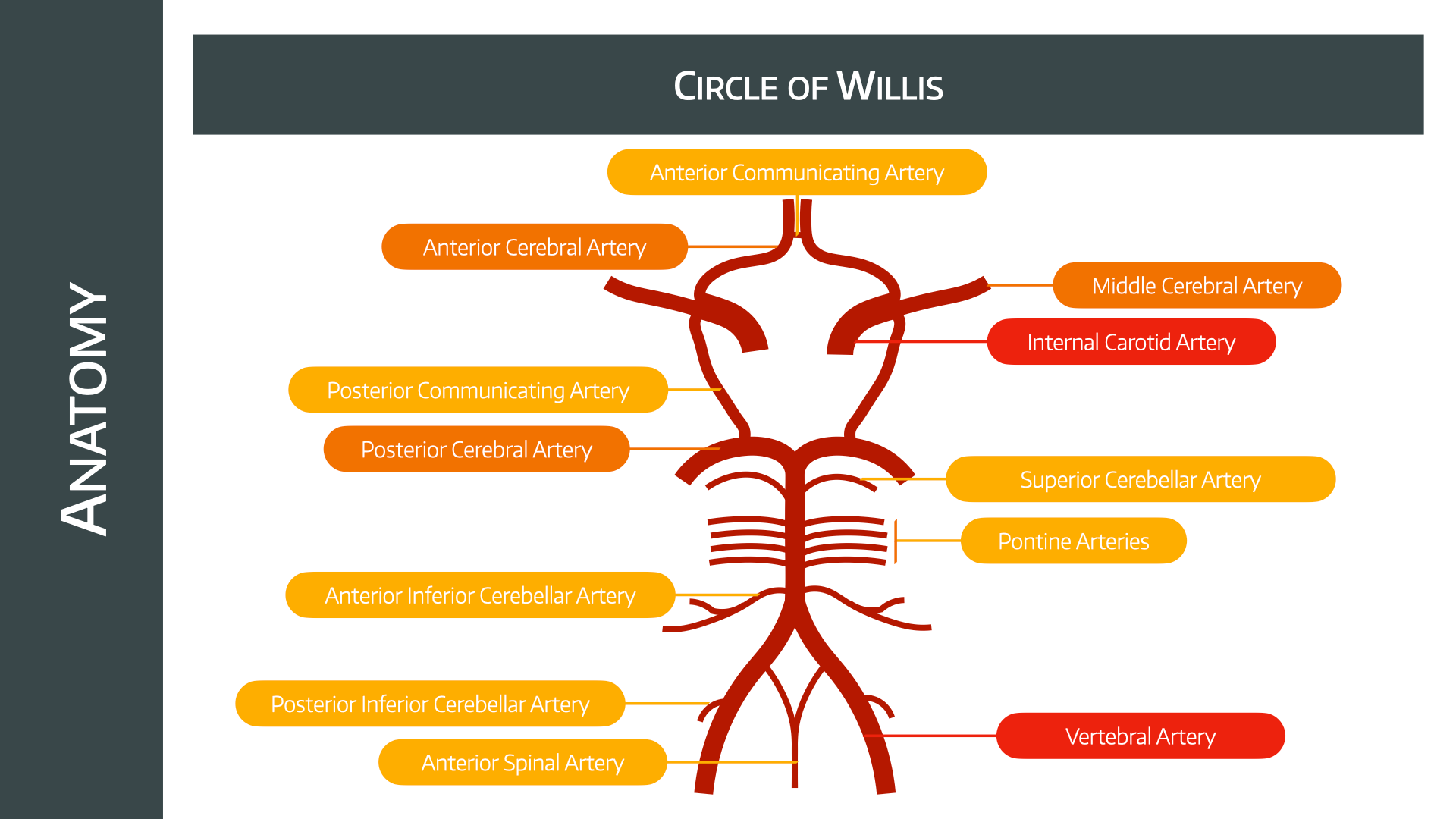
Clearly the efficiency of this collateral flow is going to vary between patients, however it is possible to install a temporary shunt to bypass the operative site when necessary.
This is not without risk, however, with scary words like 'bubble embolisation' and 'arterial wall dissection kinking' but fortunately this largely remains the remit of our surgical colleagues, and doesn't affect our plans as anaesthetists all that much.
There's also the option of an 'Eversion CEA' - the internal carotid is transected obliquely and everted to remove the plaque before reimplantation onto the common carotid. It's faster and doesn't require shunting or patching, but there isn't much difference in outcome.
What are the major complications of CEA?
- Intraoperative stroke
- Postoperative stroke
- Myocardial infarction
- Death
Bit of a theme there.
Your job
As always, keep 'em alive and keep 'em comfy - and it doesn't seem to matter all that much how you achieve this.
The patient who needs the CEA the most is also likely to be the trickiest to anaesthetise.
These are unwell patients, who have had a very recent stroke or TIA, and have had little-to-no preoperative optimisation time, so naturally they present a challenge for the anaesthetist.
The main thing is blood pressure
The most crucial aspect of your management is ensuring adequate perfusion of the brain.
While this is the case for every anaesthetic we do, you can probably appreciate it's even more important when the patient's primary pathology is inadequate perfusion of the brain, and the proposed treatment involves clamping the main artery to the brain.
Furthermore - and unsurprisingly - blood pressure is significantly more wobbly in the two weeks immediately following a stroke which can make your work as the anaesthetist in theatre a smidge more tricky.
It's vital the patient's blood pressure be controlled before the operation, as hypertension is the single biggest risk factor for developing a stroke, however it's also important to consider the risk of hypotension in a patient whose brain is dependent on a high pressure, high resistance arterial circuit prior to operating.
Why is blood pressure labile during CEA?
- Blood pressure autoregulation is impaired after a stroke
- Baroreceptor sensitivy is decreased due to atherosclerosis
- The surgery itself can trigger the carotid baroreceptors
- The anaesthesia affects autoregulation and cardiac output as well as systemic vascular resistance
- The patient often has comorbidities such as diabetes, hypertension or cardiac disease
Intraoperative hypotension can also cause stroke, but most perioperative strokes are thought to be embolic in nature.
What should I monitor?
Clearly all the usuals are a good start - ECG, blood pressure (NIBP is fine if blood pressure relatively stable up until the operation), saturations, ETCO2 etc...
We want to measure cerebral blood flow
This can be done in several ways:
- The gold standard is keeping the patient awake during surgery using regional anaesthesia, because it becomes obvious very quickly if there are any issues
Other options if using general anaesthesia include:
- Transcranial Doppler (can also spot micro emboli)
- Stump pressure measurement
- EEG
- SSEPs
- Near-infrared spectroscopy
Cerebral autoregulation is messed up more by general anaesthesia than regional, so in significant contralateral stenosis, maybe regional is better, but as always - use the technique you're good at.
Don't give too much fluid, largely because bladder distension is uncomfortable and can increase blood pressure, and don't give anything with glucose because it can harm critically ischaemic areas of the brain.
Anticoagulation
"Hi, could you give 5000 units of heparin just before I slice this dude's carotid open?"
This is normal.
The biggest risk in CEA is thromboembolism, so have a syringe of heparin ready to administer immediately prior to cross clamping.
How to anaesthetise them
Same as pretty much anything really - regional or general.
In 2004 a Cochrane review looking at 33 different studies suggested that regional is probably a good idea but there isn't enough evidence to strongly advise in preference to general anaesthesia.
The GALA trial was then conducted to answer this question, and concluded two things:
- RA and GA are both fine
- CEA is safer than it used to be
So as always seems to be the case in anaesthesia - "There's no one right answer, so choose the technique you're good at."
Another review in 2021 agreed.
What are the benefits of general anaesthesia?
- Secure airway
- Comfortable patient
- Absolute immobility
- Easier blood pressure control
- Anaesthetic agents are theoretically neuroprotective (although no real clinical evidence of benefit in CEA)
Nitrous is thought to be best avoided for many reasons, one of which is the risk of air embolism as well as its tendencey to increase cerebral metabolic rate.
What are the advantages and disadvantages of regional anaesthesia for CEA?
"Regional anaesthesia can be given as local infiltration, superficial or deep cervical plexus blockade - with or without ultrasound or a nerve stimulator."
Advantages
- Real-time, gold standard neurological monitoring
- Avoids risks of GA and airway management
- Less likely to cough and damage anastomosis or wound
- Lower shunt rate
- Shorter hospital stay
- Easier to obtain normal blood pressure at closure
- Cerebral autoregulation less affected
- RA is associated with a significant reduction in postoperative wound haemorrhage
Disadvantages
- Inherent risks of cervical plexus blocks while awake
- Pain and stress can cause myocardial ischaemia
- Risk of need to convert to GA and reduced airway access
- Not appropriate for all patients, needs to be able to lie flat
- Sedation wipes out the benefit of real-time neurological monitoring
This is a big one. If you see a patient in recovery who has just had a CEA and they're mildly agitated, confused or just a bit 'off', then you're much more likely to consider surgical complications rather than assume it's just the anaesthesia wearing off if they've had the procedure done under regional.
Regional anaesthetic techniques
The words 'cervical epidural' might send shivers down your spine - as might the procedure - but it is a legitimate technique employed in a variety of countries for CEA, but not so much in the UK.
You need to block C2, 3 and 4 if you would like a happy awake patient, and you might want to think about the trigeminal nerve to the submandibular area as well, as this bit often gets rather painfully retracted during the operation.
Furthermore, the carotid sheath itself needs its own dose of local anaesthetic as it is supplied by the glossopharyngeal nerve that your regional anaesthesia isn't likely to cover.
- Deep cervical block is never done by itself
- A combination of deep and superficial is used 70% of the time
- Local infiltration is given 10% of the time when a superficial block is already in place and 20% without
- Around half of cervical plexus blocks needed supplementing with local infiltration by the surgeon
Pain despite a decent block can occur via two mechanisms:
- crossover innervation from the other side
- visceral pain transmission via the vagus
Deep cervical plexus block
The cervical plexus is formed from the anterior rami of C2 to C4 and can be found between the middle scalene and sternocleidomastoid muscles, over the anterior aspect of the upper four cervical vertebrae.
Generally a lateral approach is taken.
The mastoid corresponds to C1, and a line is drawn to the transverse process of C5 along the sternocleidomastoid muscle.
- Moore's three needle technique
- Winnie et al's single injection method
You essentially slowly and gently advance perpendicular to the skin until your needle contacts the transverse process, then withdraw by a millimetre or two and inject (after aspirating first as always).
- Don't advance further in than 2.5cm
- Aim the needle slightly towards the feet, to reduce the chances of poking the spinal cord
You can either do multiple injections at several levels, or one bigger injection around C3.
Superficial cervical plexus block
The superficial block is becoming more popular as it is safer and doesn't seem to be any less good than the deep block.
Here's a splendid video on the cervical plexus and superficial block
- Needle inserted along the posterior border of sternocleidomastoid
- Fan needle cranially, caudally and in the middle
- Around 10-15 ml of local anaesthetic (5ml in each direction)
- You can top up with a subcutaneous injection in the midline from thyroid cartilage to sternal notch to prevent any crossover pain
You're trying to block the four main branches of the superficial plexus
- Lesser occipital nerve
- Greater auricular nerve
- Transverse cervical nerves
- Supraclavicular nerves
Cerebral hyperperfusion syndrome
This is thought to represent a form of ischaemic-reperfusion insult - worsened further by disrupted cerebral autoregulation - where previously under-perfused areas of the brain are now flooded with high pressure arterial supply that they can't handle.
You don't need to monitor them for a week.
It is essentially a form of hypertensive encephalopathy that can present with:
- Severe headache
- Seizures
- Hypertension
- A variety of waxing and waning neurological signs
The main risks are oedema and cerebral haemorrhage, with nearly 70% mortality.
The treatment is as you'd probably expect - preventative and tight blood pressure control.
Useful Tweets and Resources
Carotid endarterectomy (CEA) is a surgical procedure used to reduce the risk of #stroke from #carotid #artery stenosis (narrowing the internal carotid artery). During #endarterectomy, the #surgeon opens the artery and removes the plaque. @scientissimum pic.twitter.com/wHPs2T38fO
— The Innovation | Medicine (@Innov_Medicine) November 3, 2022
🔓Aortic dissection, aortic rupture, end-vascular treatment, open treatment, carotid endarterectomy, acute ischaemic limb, acute mesenteric ischaemia and their peri-operative complications.
— 𝘈𝘯𝘢𝘦𝘴𝘵𝘩𝘦𝘴𝘪𝘢 (@Anaes_Journal) February 2, 2023
This new review has it all!@asadmirghassemi @LizmilllerLiz
🔗https://t.co/kzAspIQTBJ pic.twitter.com/qEVPPoam0e
Here's everything you could ever want to know about cervical plexus blockade from the legends at NYSORA

References and Further Reading

Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.