Cardioplegia
Take home messages
- A stationary heart is somewhat easier to work on
- The ischaemic insult is reduced by cardioplegia, hypothermia and other pharmacotherapy
- Pre- and post-conditioning is also important to reduce ischaemia-reperfusion injury
Podcast episode
“No surgeon who wished to preserve the respect of his colleagues would ever attempt to suture a wound of the heart”
Theodor Billroth (1881)
The heart is rather a busy muscle
If all goes to plan then it commences beating at around six weeks' gestational age and continues until, well... it doesn't anymore.
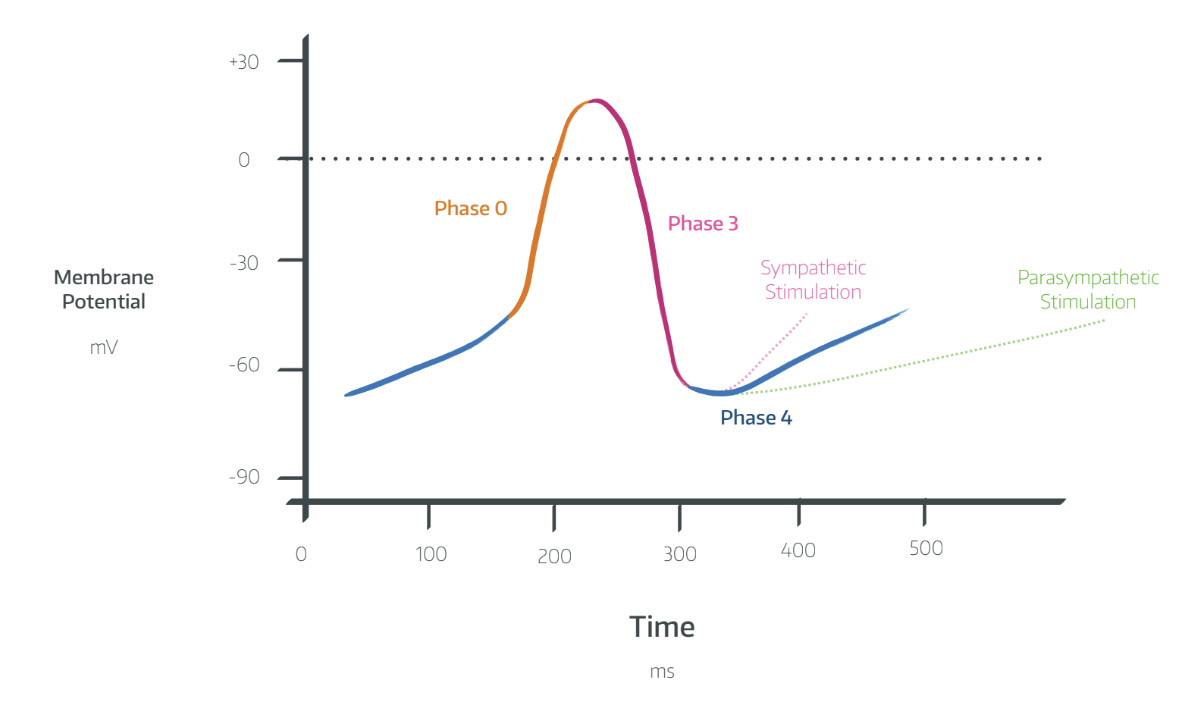
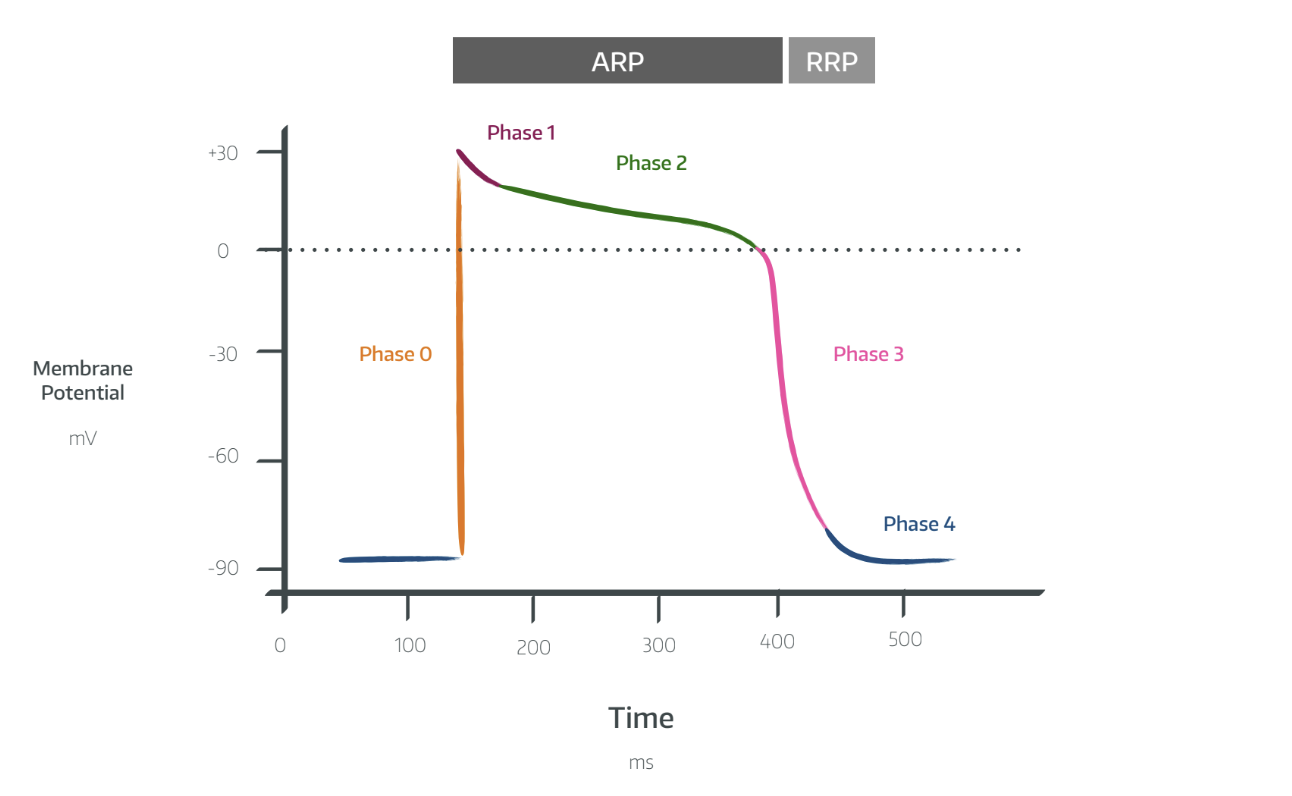
As you'll remember perfectly from medical school, it relies on ion concentration gradients and variable conduction across cell membranes to drive calcium release and myocyte contraction, all elegantly orchestrated by the conducting system with the sinoatrial node leading the way.
Sodium, calcium and potassium are the main players in this electrical dance of life and death, and the variations in their channel opening times and conduction velocities are what give the myocardial action potentials their distinctive patterns.
Hold still
The majority of the body politely stops moving once a patient is adequately anaesthetised, apart from the lungs, gut and heart.
Sure, the bowels can be a bit squirmy - and the lungs go up and down - but peristalsis isn't exactly rapid, and you have a spare lung so you can deflate if needed.
The heart, however, is really wriggly, meaning you have two options:
- Try and operate quickly and carefully with it bounding away in the pericardium (off pump surgery)
- Go onto cardiopulmonary bypass and stop the heart moving altogether to make operating easier (on pump)
If you choose the former, then good luck to you, but for the latter, you're going to need some cardioplegia solution.
A Spot of History

Meet Sidney Ringer - British doctor and pharmacologist - who in 1883 demonstrated that if you administer vast quantities of potassium to a frog's heart, the frog doesn't last very long.
The potassium induced a state of diastolic arrest.
Fast forward to 1957 and Lam starts tentatively introducing this as a splendid way to stop human hearts beating, hopefully on a temporary basis, during cardiac surgery, although there was a predictably high mortality rate due to high incidences of intractable ventricular fibrillation after the operations.
Dr Melrose and colleagues thought it was the chloride bit of KCl that was causing the problem, and used potassium citrate instead, but found similar effects and it was deemed that it was in fact the potassium doing the dirty work.
Since then the solutions used to induce reversible diastolic arrest have been tweaked and updated, such that now we can fairly reliably stop a heart completely for surgery, and start it up again a little while later.
How it works
The potassium brings the resting membrane potential up from -90mV to around -50mV. This prevents adequate repolarisation, and therefore inhibits the fast voltage gated sodium channels responsible for the initial depolarisation process.
The aim is to induce a state of diastolic arrest, with the heart relaxed and empty, achieving two main things:
- Optimising surgical access
- Hugely reducing oxygen consumption of the myocardium
So you have a nice, stationary heart that can deal with the ischaemic insult of having zero blood flow for the duration of... oh I don't know - major cardiac surgery.
The steps
- The ascending aorta is clamped, just above the coronary ostia
- The aortic cannula is inserted distal to the clamp
- The cardioplegia solution is injected into the aortic root (anterograde)
- The solution flows through the coronary circulation and induces diastolic arrest in the myocardium
- The solution can be delivered continuously or intermittently every 15 - 30 minutes
What's in the bottle
- Potassium, and lots of it (usually at least 20 mmol/litre)
The other ingredients vary, but usually involve at least a few of the following:
- Calcium - to maintain myocyte membrane integrity
- Magnesium - to prevent calcium overload and stabilise membrane
- Bicarbonate - to buffer against large pH changes and acidaemia
- Procaine - to reduce electrical excitability
- Aspartate and glutamate - to encourage oxidative metabolism
- Nicorandil - to open potassium channels and reduce energy expenditure needed to correct membrane ionic gradients
Via which routes can cardioplegia be administered?
- Anterograde - into the aortic root or coronary ostium
- Retrograde - into the right coronary sinus
- A lil' bit of both
Anterograde administration requires a competent aortic valve to ensure forward flow through the coronaries to the ventricles.
Retrograde administration is used if there is any significant occlusion of the coronary arteries, or aortic regurgitation.
Retrograde does not guarantee protection of the right ventricle however.
Cardioplegia temperature
When it comes to deciding on the temperature at which to administer your cardioplegia, there are three options:
- Cold (5–10°C)
- Tepid (27–30°C)
- Warm (37–38°C)
There are many competing ideas about which of these is best and why, but the general consensus appears to be that tepid is most protective.
Let it flow
Unsuprisingly, the majority of morbidity and mortality after high-risk cardiac surgery generally occurs as a result of the profound ischaemia and reperfusion injury sustained from the heart being stood still for quite so long.
After all, the conditions required for a happy surgeon are the exact opposite of those required for a happy heart.
So the heart is fixed, and it's time to open the flood gates and let the blood pour back into the empty and presumably rather hungry chambers.
But what actually happens during reperfusion?
Any substantial period of ischaemia is undoubtedly going to result in some degree of cell damage and death, no matter how effective your cardioprotection and preconditioning.
However if you reperfuse soon enough, then much of this damage can be recoverable, and instead of apoptosis and necrosis, you might see the much friendlier-sounding terms stunning or hibernation instead.
Stunning vs Hibernation
Cells that haven't died that become reperfused can either be stunned or go into hibernation.
- Stunning is post-myocardial impairment after blood flow is fully restored
- Hibernation is a state of persistantly impaired function at rest due to reduced coronary flow
Stunning lasts from hours to days and you can give inotropes and calcium to your heart's content.
Hibernation is thought to be due to repeated episodes of stunning, and is an adaptive response by the heart in which it essentially powers its activity down to a level where it can perform aerobic metabolism with the available blood supply.
It can be corrected by either increasing supply or reducing demand, or both.
How can we protect the heart?
By 'protecting the heart' we mean doing all we can to help it withstand the ischaemic insult that comes with being in chemically induced cardiac arrest for a protracted period of time.
There are four broad categories of protection at your disposal
- Cardioplegia
- Hypothermia
- Conditioning
- Pharmacotherapy
The cardioplegia option is the most obvious - the heart isn't doing anything, so it doesn't consume so much oxygen, so the ischaemic injury isn't so bad.
It is also by far and away the most effective protective mechanism, but the other three are still very helpful.
Cool it
It's probably not news to you that hypothermia is protective against ischaemia during cardiac arrest, and this holds true whether you're having bypass surgery or you're an unfortunate skier being dragged from an icy river.
What's not completely clear, however, is whether the benefits of hypothermia during cardioplegic bypass warrant all of the harmful side effects, given the vast majority of the ischaemic protection is provided by the cardioplegia.
As a result, many cardiac surgeons opt for normothermic bypass during their procedures.
But you need to know about it for the exam.
How does hypothermia protect the myocardium?
- Reduces oxygen consumption
- Inhibits apoptosis
- Inhibits electrical activity
At 37°C, the heart consumes 80ml oxygen/100g/minute.
At 22°C, the heart consumes 0.3 ml/100g/minute.
What is the Q10 effect?
This refers to the temperature coefficient
- A drop of core temperature by 10°C will substantially slow down metabolic processes and protect organs from ischaemic damage
- The temperature coefficient is simply a measure of how much metabolic suppression occurs for a ten degree drop in temperature
- The temperature coefficient is around 2.5 in adults and 3.65 in neonates infants and children
- Generally a temperature of 18°C is used for 'deep hypothermia'
There's also another Q10 effect in that taking coenzyme Q10 may also improve recovery after bypass surgery.
Work it
If you decided to pop out and run a marathon tomorrow, without any training, there's a moderate-to-fair chance you'll get injured and/or die.
The same applies to a heart that's about to have its blood supply cut off for an extended period of time.
This is the idea behind conditioning, of which there are two types - ischaemic, and anaesthetic.
What is ischaemic preconditioning?
Ischaemic preconditioning is deliberate exposure of the heart to brief periods of reperfusion and then more ischaemia prior to the 'real' reperfusion, to allow it to better tolerate the stress of the operation.
This weird phenomenon also explains why patients with frequent angina generally suffer from smaller infarcts than those without.
Interestingly - you can also achieve this effect after the ischaemic insult, in a process called postconditioning.
How preconditioning works
- It stresses the myocardium without killing it
- The myocardial cells express stress response genes and upregulate transcription of cardioprotective proteins*
- This armours the cell against the negative effects of ischaemia and means there's far less apoptosis and necrosis when crunch time comes
*Examples of these proteins are:
- Inducible nitric oxide synthase
- Cyclooxygenase 2
- Superoxide dismutase
- Heat shock proteins
What is anaesthetic preconditioning?
Strangely enough, ischaemic myocardium appears to enjoy huffing upon the vapours of etheric goodness.
Basically, a few decades ago, someone decided it would be entirely logical to do an ECG on a dog, while the dog was anaesthetised, and also receiving some sort of ischaemic challenge to its heart.
Well thank heavens they did, because it demonstrated substantially less ST elevation in those sent to oblivion with halothane than those who weren't.
Myocardium that is exposed to 1.5-2 MAC of halogenated vapour seems to reduce the impact of ischaemic-reperfusion injury.
Other organs appear to enjoy this as well, including:
- Brain
- Liver
- Kidneys
It's thought to reduce calcium overload and production of reactive oxygen free radicals - the main problem in myocardial reperfusion injury.
Other agents that can help with preconditioning
- Adenosine
- Nicorandil
- Xenon
- Noradrenaline
- Volatile anaesthetic agents
- Morphine (via delta receptor, so other opioids don't have the same effect)
As you might suspect, diabetes, old age and hypercholesterolaemia make any preconditioning less effective.
Steal vs cardioprotection
I know exactly what you're thinking at this point dear reader, it's obviously:
"But Anaestheasier, what about the harmful effects of coronary steal in ischaemic tissue seen with halogenated agents such as isoflurane?"
Don't you worry - after much deliberation and chin-scratching the authorities have concluded that all volatile agents are cardioprotective, and you don't need to worry about coronary steal at all.
I hadn't even heard of coronary steal and now you're scaring me
- Me neither
- The theory goes that if you have a normal blood vessel and a diseased vessel, and you administer a vasodilating agent, then the normal vessel will be much better at dilating than the diseased one
- As a result, when you dilate both of them, all the blood will rush down the normal vessel, 'stealing' it away from the diseased one that desperately needs it and the whole situation gets rather worse
- Steal syndrome is definitely a real thing (cerebrovascular and subclavian for example), but apparently we don't really need to worry about it here
Other Pharmacological options
- Interestingly, potassium-insulin-glucose infusions seem to reduce myocardial damage and requirements for inotropes in non-diabetic patients
- Propofol TIVA might be helpful, with some suggestion of reduced inotropes and myocardial damage when compared with isoflurane
- Morphine seems to have cardioprotective effects, independent of its oxygen-sparing haemodynamic effects
- α2-agonists such as clonidine also help improve mortality, especially in high risk vascular patients
- In a mindblowing twist of events, statins may also be helpful in cardiovascular patients - who'd have thought it.
All of these options are nice, but absolutely pale in comparison to the protective effect of cardioplegia, which is why it gets a whole post named after it.
Here's our article on off-pump bypass surgery

Useful Tweets and Resources
Here's a free CRQ from FRCArevision.com
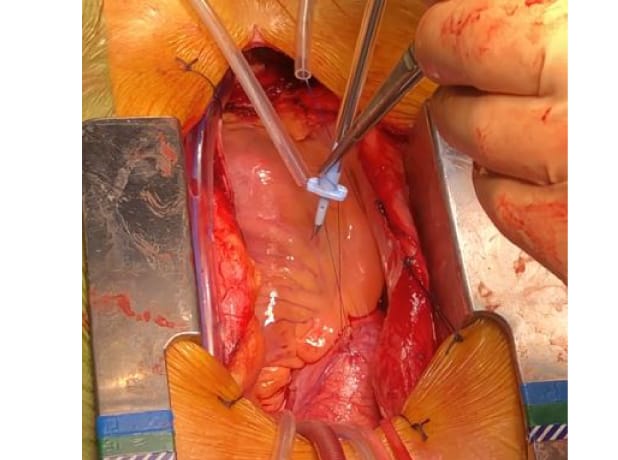
Despite significant open thrombectomy, it took a while to re-establish flow. Note opening the LAD at the apex. Note: good case to use retrograde cardioplegia pic.twitter.com/dYPmlYNv0O
— Ashraf Abou el ela (@abouelela_a) September 3, 2023
References and Further Reading



Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.


