Burns

Take home messages
- Burns patients are at risk of significant evaporative fluid loss, and should be resuscitated with crystalloid fluid according to the Parkland formula
- Anticipating future airway compromise is a key part of the anaesthetist's role
- A patient with hypovolaemic shock soon after a burn is likely to be caused by something else, such as bleeding or infection
- Significant burns require specialist management in a burns unit
What is it?
An enormous topic to start with, so here we'll focus on the crucial points that tend to get examined.
A burn occurs when thermal, electrical, chemical or mechanical energy causes coagulative damage to the skin.
A major burn occurs when more than 15% of the body's surface area is affected.
Who is affected?
Clearly anyone can be burned for any number of reasons, but there are some persistent risk factors:
- Low socioeconomic status
- Overcrowding
- Anywhere young girls work in the home in a domestic role
- Using kerosene cookers
- Poor background health
- Poor safety infrastructure
Anaesthetic concerns in a burns patient
- Airway compromise
- Hypothermia
- Blood loss
- Overactive metabolism
- Severe pain
- Changes in pharmacokinetics and drug handling
- Monitoring difficulties
Risk factors for increased mortality
- Elderly patients
- More significant burns
- Airway compromise
- Significant comorbidities
The revised Baux score is used to calculate mortality, incorporating three main factors:
- Age
- Surface area affected
- Presence of inhalational burn
What are the most common causes of death in major burns?
- Multiple organ failure
- Sepsis
- Burn shock
- Inhalational injury
It's not just the skin
As soon as you start burning more than just an isolated patch of skin, you start getting other organ systems invovled as well.
Cardiovascular
- Hypovolaemia
- Direct myocardial depression (burns shock) for up to 48 hours
- Increased capillary permeability
- Oedema and hypoalbuminaemia
Respiratory
- Direct inhalational injury
- Bronchospasm
- ARDS
- Pulmonary oedema (after IV fluids)
Renal, endo and GI
- AKI
- Increased RAAS
- HPA activation
- Ileus
- Stress ulceration (Curling ulcers)
- Abdominal compartment syndrome (after IV fluids)
The hypermetabolic phase
This starts after around 48 hours and can last up to a year.
- Increased O2 consumption
- Catecholamine production
- Excessive glucagon and cortisol release
- Increased catabolism (glycogenolysis, lipolysis etc)
- Hyperthermia
- Weight loss
- Immunosuppression
- Poor wound healing
- Weakness
Airway management in burns
As an anaesthetist, you're usually only getting involved in burns management if there is a concern about airway or inhalational injury.
All burns patients should be given 100% oxygen, to act both as pre-oxygenation in the case of rapid deterioration and need for intubation, but also to help treat carbon monoxide poisoning.
Any immediate airway concerns are usually related to trauma or a low GCS, rather than inhalational injury, which becomes an issue later as tissues become inflamed and swell.
What are the features of the history that might indicate an airway burn?
- Explosions
- Fires in an enclosed space
- Exposure to steam
- Fires involving solvent agents
- Ingestion of caustic or corrosive substance
- Laryngeal laser surgery
What are the clinical features of an airway burn?
- Stridor
- Hoarseness
- Cough
- Shortness of breath
- Burned skin on face
- Singed nasal hairs
- Soot in mouth, nose or sputum
- Hypoxia
- Confusion or drowsiness
What are the indications for early intubation in a burns patient?
- GCS less than 8 or airway reflexes not intact
- Added sounds such as snoring or stridor
- Inadequate oxygenation with hypoxaemia
- Inadequate ventilation with hypercapnoea
- Deep facial or neck burns
- Any evidence of swelling of the oropharynx
What muscle relaxant should be used in a burns patient?
- The one you are most confident with!
- Rocuronium is safe in burns patients
- Suxamethonium is safe in the first 24 hours after the burn injury
- Between 24 hours and 1 year after the injury, the upregulation of extra-junctional receptors gives a greater risk of potentially fatal hyperkalaemia
Inhalational airway injury
What are the three components of inhalational airway injury?
- Upper airway thermal injury
- Lower airway thermal injury
- Noxious gas poisoning
Upper airway thermal injury
The mouth, tongue, pharynx and epiglottis can receive a huge amount of thermal energy by the inhalation of superheated fumes, causing them to swell significantly, leading to the following clinical signs:
- Stridor
- Hoarse voice
- Swollen Uvula
Lower airway thermal injury
This is caused less by the direct heating that is seen in the upper airway, and more by the inhaltion of material that is still burning. This strips the epithelium of the trachea and large airways, stimulating production of mucus and release of inflammatory mediators.
This can lead to bronchospasm and mucus plugging, with airway obstruction and alveolar collapse.
Signs and symptoms include:
- Very productive cough
- Wheeze
- Shortness of breath
- Mucosal hyperaemia and ulceration
Noxious gas poisoning
What are the symptoms of carbon monoxide poisoning?
- Headache
- Nausea and vomiting
- Reduced consciousness
- Collapse
- Convulsions
What effects does carbon monoxide have on tissue oxygenation?
- Left shift in the oxyhaemoglobin dissociation curve, reducing haemoglobin's ability to deliver oxygen to the tissues
- Uncoupling of oxidative phosphorylation, producing a histotoxic hypoxia
- A persistent lactataemia in a patient that has received adequate fluid resuscitation should make you think of cyanide poisoning
What effect does 100% oxygen have on carbon monoxide?
- 100% oxygen will reduce the elimination half life of carbon monoxide from four hours to less than an hour
- If you can give the patient hyperbaric oxygen, this reduces even further to less than thirty minutes
- This is only really used for patients failing to respond to treatment
- If HbCO level is greater than 25% then the patient should probably be intubated and mechanically ventilated
Talk me through the Parkland Formula
- Fluid resuscitation in burns should be calculated according to body weight and % body surface area affected
- If more than 15% body surface area, or 10%+smoke inhalation, then fluids are required
- Parkland formula = 4 ml kg−1 (%surface area)−1
- Give half before 8 hours since injury
- Give the other half over the subsequent 16 hours
- Ideally give Ringer's Lactate (Hartmann's) as this has the best evidence base
- Plasmalyte may also work, but there's not enough evidence yet to suggest it's as effective as Hartmann's
- Severe hypovolaemic shock immediately after a burn is more likely to be due to bleeding than the burn itself, so don't be distracted by a severe burn
Burn patients are often trauma patients too.
How bad is it?
Often you can look at a burn and get a fairly decent idea of 'how bad' the burn is, but they can equally be deceptively severe, especially if they're so deep as to render them relatively painless.
All burns need formally assessing for severity.
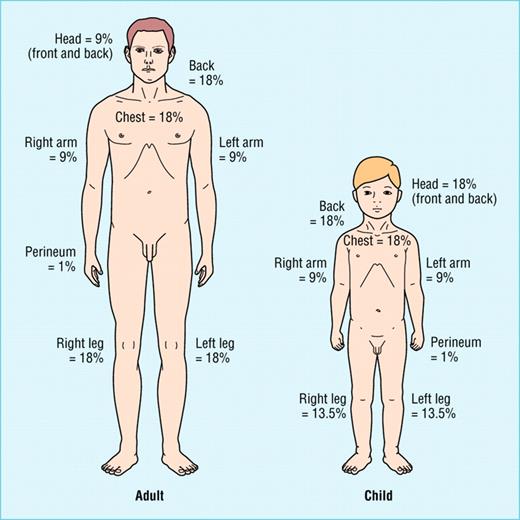
How can you assess the severity of a burn injury?
- Total body surface area
- Depth
- Lund and Browder Chart
- Rule of Nines in adults
How are burns categorised in terms of severity?
- Superficial - Red, dry and painful
- Partial thickness - Wet, blistering, red and painful
- Full thickness - White, painless, no bleeding
What are the indications for escharotomy?
- Stiff, full thickness burns
- Impairing ventilation in the thorax
- Impairing ventilation or contributing to abdominal compartment syndrome
- Impairing limb perfusion
How to look after them
We'll start with our favourite buzzphrase - multidisciplinary team input.
Surgeons
- Early excision of eschar to improve survival and reduce complications
- Grafting and reconstruction may be required
Operating theatre should be around 28-33°C
Haematology
- Monitoring and control of coagulopathy
- Management of blood loss
ICU
- Thermoregulation
- Nutrition - hugely increased basal metabolic rate*
- Fluid resuscitation - Parkland formula titrated to individual response
- Consider albumin
- Analgesia
- Psychological support
- Physiotherapy
- Occupational therapy
*Starting enteral feeding within 12 hours improves outcomes - they need 1.5 to 2 g/kg/day protein.
Microbiology
- Hugely immunosuppressed patient with loss of epithelial barrier
- Staph aureus
- Pseudomonas aeruginosa
- Candida
Useful Tweets and Resources
Intubating a patient with upper airway inhalation burns @protectedairway #Medtwitter #MedEd pic.twitter.com/q6TCqJGfYw
— Journal of Brown Hospital Medicine (@BrownJHM) January 5, 2023
References and Further Reading
Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.