Brainstem Death Testing

Take home messages
- There are two types of death - cardiorespiratory death, and death by neurological criteria
- There are strict requirements to confirm death by neurological criteria
- Brainstem death can have profound physiological effects that may need correcting if a patient is to undergo organ donation
Saved by the bell
Death is rather a tricky subject, but one we encounter a lot in our particular line of work.
It's quite important to know when someone is dead, because if you don't, you might end up burying them alive.
This sort of happened rather a lot in the 18th century, so they started burying people with a string attached to their wrist connected to a bell on the surface, alerting the world that they were in fact, still going strong, should they wake up in what is quite possibly, the worst place to be.
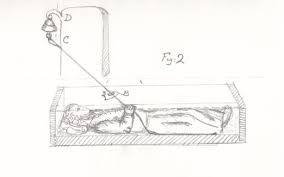
Hence we now have the terms 'saved by the bell' and 'graveyard shift'.
Death is weird when you think about it
The concept is fairly simple - the processes that made you 'alive' beforehand have clearly ceased to be, but defining exactly when that moment has occured is rather more nebulous.
What is the definition of death in the UK?
- The irreversible loss of capacity for consciousness
- The irreversible loss of capacity to breathe
The patient's heart has stopped, there are no breath sounds, no pupillary response or signs of life.
They're dead (by cardiorespiratory criteria).
But if you consider that person in terms of the cells that make up their body, presumably a very large number of their tissues are still metabolising, making proteins, consuming glucose, still very much living for a considerable amount of time after you've peered into their eyes and written in their notes for the last time.
And if you take into account the patient's gut bacteria, then in terms of number of cells, they're still like.... 99.9% alive...
Weird.
Ask any experienced ward nurse and they'll be able to tell you with confidence when their patient has 'passed', and is ready for the junior doctor to go through the motions of confirming said fact, just remember that technically you need at least five minutes of asystole.
However on the intensive care unit it gets a little more complicated, because we're then introduced to the concept of 'brainstem death', or more correctly 'death by neurological criteria'.
Death by neurological criteria
What are the three essential components of diagnosis of death by neurological criteria?
- Fulfilment of required preconditions for brainstem death testing
- Exclusion of potentially reversible pathology causing coma or apnoea
- Formal brainstem testing*
*To demonstrate coma, apnoea, and the absence of brainstem reflexes
Required preconditions for brainstem death testing
- Known pathology causing irreversible brain damage
- Comatose
- Apnoeic
- Mechanically ventilated
Things to exclude before testing can be done
- Hypothermia (needs to be above 34°C) (updated 2025 to 36°C)
- Exclude metabolic and endocrine derangement
- Patient must demonstrate cardiorespiratory stability
- Exclusion of sedatives or muscle relaxants as a contributing factor
Hypothermia is an important factor
Because below a core temperature of 34°C it's quite likely the patient will be unconscious, and below 28°C, their brainstem reflexes may well be absent, so as the old saying goes...
They're not dead until they're warm and dead
Electrolytes and metabolites should be corrected
Sodium, potassium, glucose, phosphate and magnesium should all be as normal as possible before testing to ensure there isn't a potentially reversible metabolic reason as to why the patient is profoundly unconscious and not breathing. Endocrine disturbance such as myxoedema coma or addisonian crisis should be corrected for the same reason.
Cardiorespiratory stability is a relatively recent addition to the exclusion criteria
The patient's mean arterial pressure should be at least 60mmHg, pH normalised without significant hypoxia or hypercapnoea, again to rule out possible reversible causes of coma. If these parameters are not achievable, then it's likely the patient will naturally progress to cardiorespiratory death, rendering brainstem death testing somewhat redundant.
Sedatives and muscle relaxants
Allow at least four elimination half lives to pass after administering any sedatives or paralysing agents, or give the necessary reversal agents and test plasma levels to ensure they're not circulating at clinically significant levels.
I'm hoping the reason for this is obvious by now.
There are two steps to brainstem death testing
- The cranial nerve tests
- The apnoea test
Which cranial nerves are we testing to assess the brainstem's integrity?
Pupillary reflexes
- Afferent limb is CN 2
- Efferent limb is CN 3
A bright light is shone into each eye, testing for absence of both direct and consensual reflexes
Corneal reflex
- Afferent limb is CN 5
- Efferent limb is CN 7
The patient will not blink when the cornea is lightly touched
Vestibulo-ocular reflex
- Afferent limb CN 8
- Efferent limb CN 3, 4 and 6
Ice cold saline is poured onto the eardrum, and if the eyes do not move then the reflex is absent
Pain response
- Afferent limb CN 5
- Efferent limb CN 7
This is if the supraorbital notch is used as the site of a painful stimulus
Gag reflex
- Afferent limb CN 9
- Efferent limb CN 10
No gag response to touching the back of the pharynx
Cough reflex
- Afferent limb CN 10
- Efferent limb CN 10
No cough response to stimulation of the carina on deep suctioning with a suction catheter
Some things may still be present
The Final FRCA likes to try and catch you out by asking about other features, and whether they need to be absent as well for a brainstem death testing to be completed.
Note that:
- Spinal reflexes may still be present
- EEG not a required precondition for brainstem death testing, but can be used as an auxillary test if formal BSD testing isn't possible
- Absence of doll's eye (oculocephalic reflex) is not used as a precondition or part of the test
The apnoea test can only be performed once the above reflexes have been tested and demonstrated as absent.
The apnoea test tries to stimulate breathing by raising PaCO2 and therefore drop CSF pH sufficiently that even a profoundly unconscious and apnoeic patient would start showing respiratory effort if the pathology were meaningfully reversible.
The apnoea test
- Patient must be cardiovascularly stable
- Preoxygenate with FiO2 of 100%
- Reduce minute volume to increase PaCO2 above 6 kPa* (updated to 5.3)
- Disconnect patient from ventilator and observe for 5 minutes
Use end tidal CO2 monitoring and watch for respiratory effort. Ensure PaCO2 has increased by at least 0.5 kPa before reconnecting to the ventilator
Why test for brainstem death?
In legal terms, the patient is declared 'dead by neurological criteria' upon completion of the second set of tests.
Confirming that a patient is now legally dead allows for two things to happen:
- The patient's family can be informed with certainty that there is no possibility of recovery, and that by withdrawing life support, they are not 'killing' or 'giving up on' their relative, and prevents unnecessary prolongation of their grieving process
- It facilitates the donation of live organs rather than DCD or donation after circulatory death where the organs have a degree of 'warm ischaemia'
What are the contraindications to organ donation in brainstem dead patients?
- Active haematological malignancy
- Metastatic malignancy
- HIV
- CJD
- Melanoma
Also if the patient is known to have previously declined to donate in the event of their passing.
The specific criteria for organ donation, both for DCD and DBD are beyond the scope of this post, but we will write an organ donation post in due course!
The Rules have Changed
There have been recent updates to the criteria required for completion of brainstem death testing.
I doubt that you will be penalised in the exam for using the older criteria in the exam, for at least the next few years, but it's good to be aware - you know, for actually doing the job properly.
2025 Updates
Age:
- Under 37 weeks gestational age: DNC cannot be confidently made
- 37 weeks to 2 years: Criteria align with those for older children and adults, with certain caveats:
- A minimum observation period of 24 hours before testing
- A 24-hour interval between the first and second sets of tests
- No ancillary investigations are required
- 2 years and above: Same criteria as adults
Apnoea Testing:
- Start at PaCO2 ≥ 5.3 kPa
- End point is PacO2 ≥8.0 kPa, pH <7.3
- The PaCO2 needs to have risen by at least 2.7 kPa
- Wait for at least five minutes before taking the blood gas
Time of Death:
- Record at completion of second set of tests
- If waiting on further investigations, it's when the results are available to the two doctors performing the second set of tests
Minimum Temperature:
- Core temperature must be at least 36°C at time of testing
- If colder, you need to warm them to 36°C and then wait 24 hours before testing
Examining:
- You need to be able to access both ears and both eyes to examine
- If not then other testing will be needed
Related Posts


Useful Tweets
Brainstem Death testing: an emotive, difficult and sensitive topic, but vital knowledge for all Intensivists/Anaesthetists/Surgeons clinically and for the exams #TUGS @T4UGIS @ASiTofficial @TransplantJrnl @asgbi @HPBDublin @Transpl_Int @RCoANews @RCSnews @RCSEdYF @RCSEdFST pic.twitter.com/AgJGIY5Bv4
— The Roux Group (@roux_group) November 18, 2020
YouTube Demo
References and Further Reading



Primary FRCA Toolkit
Brainstem death testing is largely the remit of the Final FRCA exam, but the Final can catch you out with up to 20% of it covering Primary material. Check out our toolkit if you haven't already!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!


