Bone Cement Implantation Syndrome

Take home messages
- It's not very well understood, but BCIS can be fatal, so it's not to sniffed at
- If your patient is very old and frail, probably best to avoid cement
- Learn to start optimising blood pressure and oxygenation as soon as you smell the cement cooking
"Cement going in"
Welcome back, dear reader, and join us as we wander into the mysterious world of bone cement implantation syndrome, the haunting condition that has the anaesthetist putting their crossword down and drawing up some good-luck ephedrine as that all-too familiar smell wafts over the blood brain barrier.
Hopefully, when the surgeon yells this while wielding the cement gun like a sterile blue Rambo, you've already smelled what is to come and checked your patient is as cardiovascularly stable as possible to tolerate the impending insult to the femur, heart and lungs.
In general, young and cardiovascularly healthy people can tolerate a full gun of cement to the femoral canal without too much trouble, but unfortunately young and cardiovascularly healthy people rarely need a hip replacement.
60 000 hip replacements are done per year in the UK, usually for arthritis, and at least 14% are ASA 3 or worse.
A hip can be uncemented, cemented or hybrid, which for you as the anaesthetist means cemented.
Around 70% of total hip replacements are cemented.
So what does BCIS look like?
The cement ploughs down the freshly reamed femur and any or all of the following can occur within seconds to minutes:
- Hypotension
- Hypoxia
- Arrhythmias
- Loss of consciousness
- Pulmonary hypertension
- Cardiac arrest
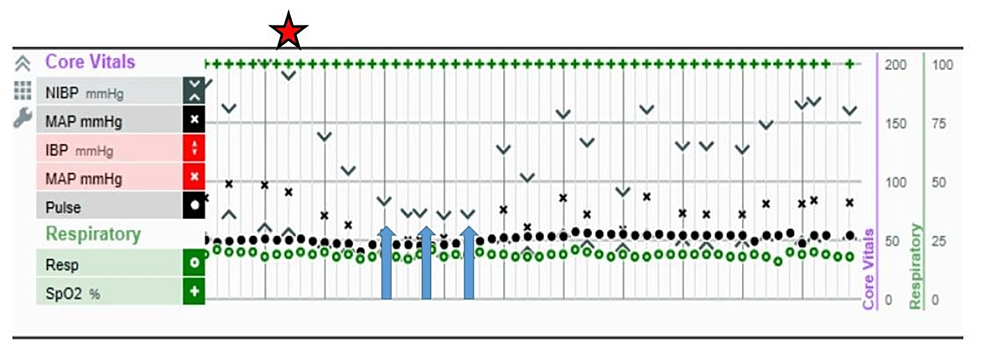
Now we don't routinely monitor for pulmonary hypertension, and often these patients have at least a bit of sedation on board, so your first clue (if you don't have an arterial line) is likely to be a drop in oxygen saturations, or hypotension when the NIBP cuff next decides to inflate.
What actually happens?
We don't really know for sure, but if we start with what we do know, and try to join the dots, we end up with a couple of logical theories.
What we know
- Cement is forced under pressure into the hollow femoral medullary canal, where it gets very hot and expands, exerting substantial pressure on the inside of the femur to encourage a decent bond between prosthesis and patient
- The clinical syndrome is one of hypoxia, hypotension, increased pulmonary vascular resistance and peripheral vasodilatation (looks a bit like a PE)
What we see in bad cases of BCIS is a catastrophic increase in pulmonary vascular resistance with the resultant increase in pulmonary artery pressure. This not only produces enormous afterload for the rather feeble right ventricle, but also plays havoc with the delicate V/Q matching process in the alveolar bed.
Once the right ventricle fails to pump the blood forward and begins to dilate, the interventricular septum naturally deviates left, and both of these factors then reduce the diastolic filling of the left ventricle.
This leads to hugely reduced end diastolic volume and cardiac output.
What we can logically deduce
The high pressure in the medullary canal might be forcing embolic material into the blood (fat, clot, cement, air, bone) into the circulation, whereupon it travels to the lungs and starts causing problems.
The two theories
This question is prime CRQ and SOE fodder, so just memorise these two points:
- The monomer model
- The embolic model
The monomer model suggests that individual methylmethacrylate monomers leach across into the circulation and trigger a hypersensitivity-esque reaction within the pulmonary vasculature.
The embolic model meanwhile suggests that a bunch of medullary content (fat, cement, bone etc) gets forced into the venous system and causes a pulmonary embolism-type of picture.
The embolic model is probably correct
It's still not 100% clear, but it's increasingly thought to be due to a mixture of bone cement, air and medullary fat being slammed into the blood stream by our enthusiastic colleagues-of-carpentry, leading to a rather ruthless blend of:
- Physical pulmonary vessel obstruction
- Histamine release
- Complement activation
Imagine all the worst bits of a pulmonary embolism, and anaphylaxis, and smush them together in a frail osteoporotic patient with cardiopulmonary disease and you can understand why the mortality of BCIS is rather high at around 9% across all severities.
Some very clever people have managed to increase the available evidence for an embolic phenomenon by using trans-oesophageal ultrasound during the cementing process, demonstrating a 'snow flurry' appearance of emboli in the right atrium and ventricle.
Bone cement implantation syndrome #POCUS #anesthesia #EchoFirst . Occurs in 20% patients undergoing cemented prosthesis for hip fracture repair; in 2,5% cases with cardiovascular collapse requiring CPR, like this case in our hospital https://t.co/uDEuXJtpdt pic.twitter.com/QUlykghvnC
— Anestesia 🏥 12 de Octubre (@AnestesiaH12O) March 11, 2021
As well as inducing a mechanical obstruction of the pulmonary vasculature, it is thought that embolic material then causes release of vasoactive and pro-inflammatory mediators including thrombin and tissue thromboplastin that induce pulmonary vasoconstriction and peripheral vasodilatation - thereby worsening the strain on the right ventricle and reducing the effective afterload for an underfilled left ventricle.
Bad news.
So how bad does it tend to be?
The majority of the time, your patient may demonstrate a slight, and brief, dip in oxygen saturations, and maybe a bit of hypotension, and nothing else. Often this goes completely unnoticed, hence there's difficulty in working out just how common it actually is.
Alternatively they might be a bit more confused than expected in recovery.
To give a more concrete (pun intended) scale of severity, Donaldson et al. in 2009 came up with the following scale:
How is bone cement implantation syndrome graded?
Grade 1
- Sats <94%
- Greater than 20% reduction in systolic blood pressure
- No change in GCS
Grade 2
- Sats <88%
- Greater than 40% reduction in systolic blood pressure
- Loss of consciousness
Grade 3
- Cardiovascular collapse
- Requiring cardiopulmonary resuscitation
You tend to notice grades 2 and 3.
Who gets it?
The cruel twist of fate here is that the most likely people to suffer from significant BCIS are also those who are also the least able to cope with it.
As always there are anaesthetic, patient and surgical risk factors.
With regards to anaesthetic risk factors, it doesn't really seem to matter how the patient is anaesthetised, but it very much does matter how cardiovascularly robust they are at the time of cementing.
- There's not any strong evidence to demonstrate an impact of anaesthetic technique on susceptibility to, or severity of, BCIS, however there is flimsy evidence in animal studies to suggest that volatile agents might make it worse, but this was comparing isoflurane vs benzo + fentanyl, which isn't a widely used technique in humans to say the least
- So probably ignore these bullet points
Hypotension, hypoxia and hypovolaemia are all going to worsening the clinical picture should BCIS rear its ugly head.
What are the patient risk factors for BCIS?
- Hypertension
- Significant cardiovascular or respiratory comorbidity
- ASA 3 or 4
- Pulmonary Hypertension
- Osteoporosis
- Male sex
- COPD
- Use of diuretics and warfarin*
*Presumably because patients on diuretics and warfarin tend to have significant cardiovascular or respiratory comorbidities, but apparently it scores a point on its own.
Surgical risk factors for BCIS
- Intertrochanteric fracture
- Pathological fracture*
- Long stem arthroplasty
*This is unsurprising given the cohort of patients that tend to get pathalogical fractures, but it does get you a point in the exam.
What do I do about it?
Ideally avoid it in the first place.
The harsh reality is that as the anaesthetist there's not a whole lot you can do to reduce the risk of BCIS, but there is one thing you can do:
Have a discussion with the surgeon about whether cement is a good idea beforehand.
This sounds ridiculously simple but in retrospective analysis it was found that very rarely do the surgical and anaesthetic teams actually proactively discuss whether cement is too risky for the patient at hand.
By identifying these patients and avoiding cement where advisable, the risk can be dramatically reduced in your highest risk cohort, and it's one of the biggest patient advocacy marks you can score as their anaesthetist.
How can risk of BCIS be reduced?
- Not using cement in the first place
- Washing femoral canal prior to cementing*
- Depressurising the medullary canal with a venting hole
- Using a bone-vacuum cementing technique
- Retrograde insertion of cement
- Low viscosity cement
*They like the phrase 'pulsatile lavage' if you're interested.
If you can't avoid it, then spot it as early as possible
As with all patients and all anaesthetics that you've ever done, the same rule applies - the more concerned you are, the more monitoring you should add.
If you have an arterial line in situ, then your first clue of BCIS might be a drop in blood pressure, otherwise you'll probably notice a dip in oxygen saturations before the NIBP cuff next kicks in.
The key is to be alert and expect it as soon as you smell the cement being mixed.
You might even have to stand up.
What is the immediate management of BCIS?
Inform the whole theatre of the issue, and then add the following in order as required:
- 100% oxygen and secure the airway if required
- Intravenous fluid challenge
- Vasopressors
- CPR if complete cardiovascular collapse
- Pulmonary vasodilators if available and feasible
- Inotropes
- Invasive monitoring
Pulmonary pressures usually normalise within 24 hours.
Some institutions have implemented a 'cement curfew' protocol, to highlight the importance of the cementing procedure and ensure that the whole theatre team is vigilant to bone cement syndrome during the critical period of time when the cement is inserted.
First up for our group is how to mix bone cement, delivered by Vicky (thank you) a training video first followed by a demonstration then getting hands on 🦴 also learning about our Bone Cement Curfew. @DePuySynthes @UHMBT #theatres #ortho pic.twitter.com/JFaTwmzM8m
— We are FGH Theatres (@FghTheatres) May 12, 2022
Hit 'em hard and hit 'em early
Resuscitating BCIS is fairly simple on paper - it's the B and C bit of your ABC.
Oxygen, fluids, pressors and inotropes - just get the blood full of oxygen and pumping round and round, even if you have to do it manually in the case of Grade 3 BCIS.
There's not much more to it than that - oh, and ICU afterwards if they're unwell.
Mercifully BCIS seems to be a short-lived phenomenon, with pulmonary arterial pressures normalising within 24 hours in the vast majority of cases.
After stabilising the patient
The vast majority of the time, the clinical presentation of BCIS is mild and transient, but as with any critical incident or resuscitation, if you have any ongoing concerns about the patient, then have a low threshold for admission to HDU for close post-operative monitoring.
Why bother using cement?
It sounds a bit like using cement is a recipe for disaster, so one would be forgiven for asking why we even bother in the first place.
Well apart from 'the orthopods like it', there are in fact several advantages to using the stinky green death mousse after all:
- The joint lasts longer
- An osteoporotic joint becomes stronger (so the joint lasts longer)
- You can swill antibiotics into the cement (so the joint lasts longer)
- Once the cement is set you can test and be sure that the joint is stable (so the joint lasts longer)
NICE recommend that primary hip replacements should be done with cemented prostheses where possible. They're more cost effective (£5305 vs £5901 as of 2008*), but because the joints tend to last longer, rather than being cheaper to do at the time.
(*so like, £5000000000000000000 in 2023)
TLDR
- Expect bone cement syndrome
- Give oxygen, fluid and pressors early
Useful Tweets
#AnaesthesiaWorld #Infographics #OSCE BONE CEMENT IMPLANTATION SYNDROME (BICS)
— Shiv Kumar Singh (@ShivRoyal) January 14, 2022
Important for both #Anaesthetists and #Orthopaedics #Orthopedics pic.twitter.com/9NsGnIGPVM
Review Question of the Day for today: Bone cement implantation syndrome. Test yourself: https://t.co/MRbAM1wYeP
— OpenAnesthesia® (@openanesthesia) June 17, 2016
References and Further Reading


Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!


