Bispectral Index (BIS) and depth of anaesthesia monitoring
Take home messages
- Awareness under general anaesthesia may be as high as 1:660 anaesthetics
- Use BIS for TIVA cases, and practice on volatile
- Learn the parameters that make the number unreliable
Sweet dreams
Given all of our general anaesthetic agents work in the brain, it's rather strange that we have no way of measuring exactly how much we're giving or if it's actually working.
Sure - we have clinical parameters to reassure ourselves the patient 'must be pretty comfortable' and can measure end tidal concentrations of vapours to tell us they've got 'enough on board', but in reality, we're still sort of guessing.
Now, a patient with no muscle relaxation on board will generally give clues that they're a smidge light well before awareness is likely to become an issue, because they will flinch or frown, and we can set about getting them deep enough again.
However a paralysed patient will not, (unless for some insane reason you've decided to employ the isolated forearm technique) and this is one of the reasons why neuromuscular relaxation is such a significant risk factor for awareness.
Sadly, we're still a while away from direct point of care brain-agent concentration monitoring, however we are one step closer with the advent of EEG monitoring.
Off to sleep
General anaesthesia is a (hopefully) temporary, or reversible, state of drug-induced loss of consciousness.
The patient - quite reasonably - expects to be unaware of everything from induction to recovery, and it is this awareness that we worry about, as it is generally avoidable and unsurprisingly very distressing.
"I remember going to sleep after your injection in my arm, and some time later I was awoken by the most excruciating pain in my tummy. It felt as if my whole inside were being pulled out; I wanted to cry out or otherwise indicate my suffering but I couldn't move any part of me.
I heard the doctors talking about the gall-bladder and about doing something with it to the small intestine. Then I went to sleep again and later on woke up here in bed."
E. H. Winterbottom's case report of awareness in 1950 in a young woman underoing laparotomy for partial pancreatectomy
Yikes.
NAP 5 set out to characterise just how much of a problem awareness is, and you can read all about it here.
How does EEG work?
Your brain, like your heart, runs on electricity and produces similar patterns of electrical waveforms depending on its level of activity.
By plonking electrodes all over the head, we can draw squiggly lines that represent cortical electrical activity, and then someone with the title of 'ultra highly specialised clinical electrophyiologist' or similar can read the magic squiggles and tell us whether the patient is alive, asleep, seizing or absent from the ward.
For now, we'll simplify things a bit.
When wide awake, it generally produces lower amplitude but higher frequency waves.
When fast asleep, higher amplitude but slower, more regular waveforms start to appear, as shown in this nice summary:
Nice diagram of EEG waveforms during stages of Anaesthesia. Useful for BIS/pEEG interpretation whilst TIVA-ing
— Chris Tomlinson (@tomlincr) December 5, 2019
Source: https://t.co/mWkaRNa3hL@SIVAnaesthesia pic.twitter.com/MzXkPYjjjO
It's a little more complex than that.
Your brain actually pumps out a whole chaotic variety of waveforms, and the more electrodes you stick on the person's head, the more waves you're going to see.
What then happens is a clever machine does clever things including a Fourier transformation (make sure you say those words in the exam) to produce four characteristic waves that we know as:
- beta - β - 13-30 Hz (fastest)
- alpha - α - 7-13 Hz
- theta - θ - 3.5-7 Hz
- delta - δ - 0.5-3.5 Hz (slowest)
In short beta = wide awake, while delta = fast asleep.
Okay but what is 'burst suppression'?
- By measuring the various waveforms and how they vary over time, the EEG monitor can generate a ratio of how much the electrical activity is suppressed for in a given unit of time
- A higher suppression ratio suggests deeper anaesthesia, hypoxia or brain damage (trauma or otherwise)
Okay, but what is frequency domain analysis?
- Take your raw EEG signal
- Do your Fourier analysis to get your alphas, thetas and whatnot
- Then draw a graph with the frequency on the x axis, and the amplitude* of that signal on the y axis
- You're essentially graphically representing which of your alphas, thetas etc have the biggest signal
*Technically it's the power plotted on the y axis, which is just amplitude squared.
Okay, so what is BIS?
- BIS is frequency domain analysis, plus a bit more
- It uses both power and phase information of the various component waveforms at 2 specific frequencies
- It then uses statistical analysis and churns out a number between 0 and 100 depending on how well these components seem to 'align'
- 100 = wide awake
- 0 = flat line badness
- 40-60 = surgical general anaesthesia
You definitely don't need to be able to explain much more than that.
What do the SQI and SR bits mean?
- SQI (signal quality index) - How good is the signal? - 100% = perfect signal quality and 0% = terrible
- SR (suppression ratio) - For what proportion of the preceding 63 seconds was the EEG activity isoelectric? - Bigger SR = more unconscious
How reliable is it?
Ah the million dollar question - can I trust it?
'Sort of' is the answer.
You've probably worked with consultants that quite happily run TIVA without any depth of anaesthesia monitoring, because that's how they did it for many years before BIS came along.
They know with next to 100% reliability that if you've pumped a certain amount of propofol and remifentanil into a person of a certain age and weight, and the cannula is visible and working, and they've got a heart rate and systolic that barely sum to 150 - then the patient is probably asleep enough.
This still applies if you're using BIS - you've just got an extra layer of reassurance if the BIS is 39.
BIS should be an 'extra check' rather than your primary monitoring end point.
It is not a definitive 'yes that's enough' in the way that MAC is commonly used. They're more of a 'if the heart rate and blood pressure are chilled, then you're probably fine' kind of vibe.
BIS is good for TIVA
Largely because we don't have any other option, but mostly because BIS correlates pretty reliably with plasma concentrations of propofol when we actually measure them.
If you apply the electrodes properly, avoid ketamine and nitrous, use propofol and tell your BIS monitor to alarm if it wanders outside the range of 40-60, then it seems to work as well at avoiding awareness as if you use vapour and tell it to alarm outside of a MAC of 0.7-1.3.
One of the key things to appreciate is whether there is anything else going on that might make your reading unreliable.
Which physiological parameters will influence the BIS reading?
- Hypothermia
- Hepatic encephalopathy
- Hypovolaemia
- Hypotension
- Hypoglycaemia
- Also if the patient is physiologically asleep
What anaesthetic factors can affect BIS monitoring?
- Electrode misplacement
- Facial muscle activity
- Electrical interference - diathermy, pacemaker, other monitoring*
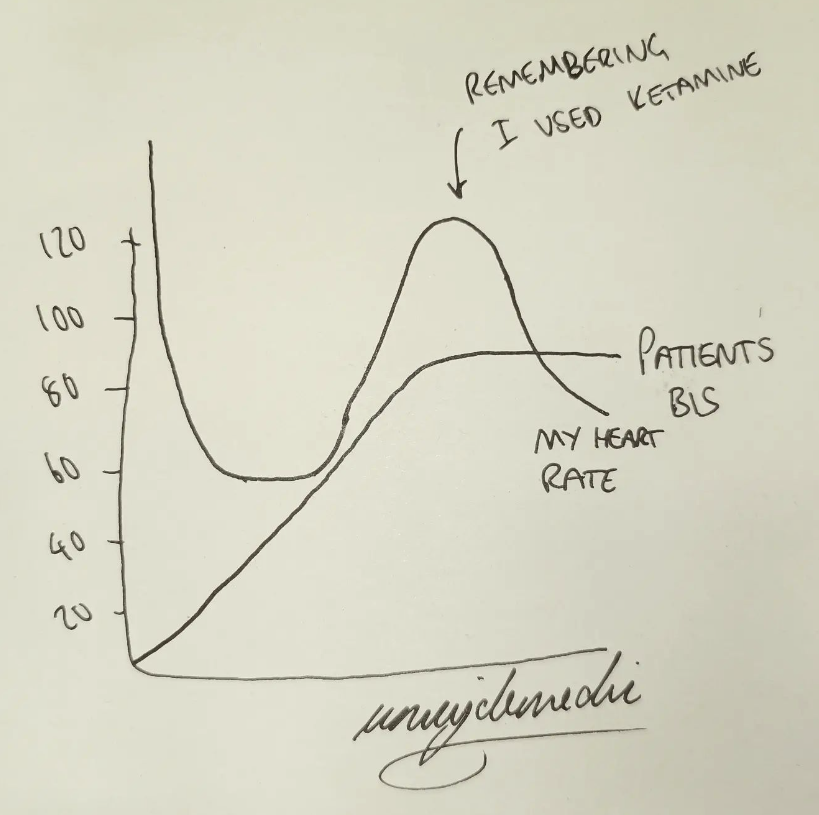
- Muscle relaxants can lower the BIS number without making the patient more unconscious
- Nitrous oxide - preserves alpha waves and suppresses delta waves, so even though the patient is asleep, their BIS number will be higher
- Ketamine also gives a falsely high reading
*I once managed to pick up a patient's ECG waveform on the BIS monitor.
I called it heartifact.
Any other benefits?
Yes, actually, BIS helps save money and the environment, because if you use it properly, patients tend to use up less anaesthetic and wake up quicker (because you've not overanaesthetised them unnecessarily).
Unsurprisingly they also have fewer side effects such as nausea and vomiting and cognitive dysfunction.
So should I use it?
Yes.
Practice with it on vapour cases, learn to incorporate it into your anaesthetic management and definitely use it for relaxed TIVA cases.
Just remember it's another number on the screen, and not the be all and end all of your anaesthesia.
A final top tip
- Use a validated TCI model, and watch at what estimated plasma concentration that patient actually falls asleep - then use this as a reference point to ensure your patient doesn't risk waking up during surgery
Useful Tweets
🔐This new #FreeForADay RCT shows that rapid reversal of deep neuromuscular blockade with sugammadex was associated with increases in BIS values and clinical signs of awakening in 27% of patients, despite maintenance of general anaesthesia.
— 𝘈𝘯𝘢𝘦𝘴𝘵𝘩𝘦𝘴𝘪𝘢 (@Anaes_Journal) April 30, 2020
🔗https://t.co/36FdcqyfRa pic.twitter.com/cRKilduSG6
#ATOTW 416: Bispectral index (BIS) monitoring and intraoperative awareness.
— WFSA (@wfsaorg) December 31, 2019
This tutorial summarises the data & controversies of using the BIS™ & provides recommendations regarding its appropriate use in general #anaesthesia to prevent awareness. https://t.co/dWAai2nYU1#WFSA pic.twitter.com/RWPKTKYGOm
References and Further Reading
Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.
