Beta blocker overdose

Take home messages
- ABCDE and opening ToxBase is all you really need to know
- The clinical presentation is bradycardia, hypotension and shock
- Pay particular attention to sotalol and propranolol
The solution to pollution is dilution
Let's be honest, the vast majority of toxicology is ABCDE, fluids and supportive care.
Occasionally there's an antidote.
Can you name any specific antidotes?
- Benzodiazepines - Flumazenil
- Ethylene glycol and methanol - Fomepizole and ethanol 10% IV
- Organophosphates - Atropine
- Warfarin - Factor II, VII, IX, X concentrate
- Cyanide - Dicobalt edetate and hydroxycobalamin
- Digoxin - Digibind
- β-Blockers - Glucagon
- Methaemoglobinaemia - Methylene blue
- Paracetamol - N-acetylcysteine
- Opioids - Naloxone
But for beta blockers, there isn't, so guess what - it's supportive care.
Things to watch out for
- Mixed overdose
- Interaction with other medications (especially antihypertensives)
- Elderly patients
- Cardiovascularly frail patients
- Sotalol and Propranolol are the most lethal beta blockers in overdose
Every patient suspected of having taken an overdose needs a paracetamol level checking.
What actually happens
Your patient intentionally or accidentally takes an enormous quantity of beta blocker.
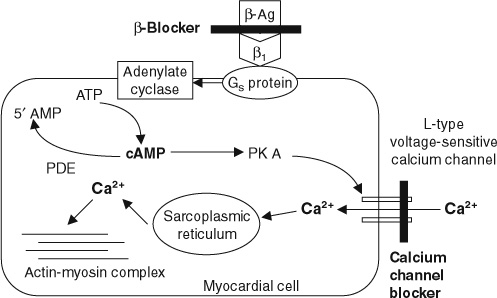
- These start blocking β1 and β2 receptors with varying avidity and selectivity
- Reduced intracellular cAMP production in a variety of target tissues, particularly the heart
- Reduced calcium movement into cardiac myocytes, as well as other muscles
- This therefore has the opposite effect of the body's own catecholamines, dropping blood pressure by reducing force of contraction (inotropy) and heart rate (chronotropy) by slowing down the conduction speed of the conducting pathways (dromotropy)
- If left unchecked this leads to cardiogenic shock and heart failure
What receptors are where?
These are Gs category G-protein coupled receptors.
β1
- Heart
- Kidneys
β2
- Lungs
- Muscle
- Blood vessels
It depends a bit on the drug itself
Beta blockers have different affinity for each type of beta receptor, and so the clinical presentation will depend a bit on which drug they've taken:
- Cardioselective agents will cause profound bradycardia and hypotension
- Fat soluble drugs (propranolol) cause CNS symptoms
- Peripheral vasodilators will mainly cause hypotension
Why is propranolol special?
- Causes blockade of sodium channels
- The QRS widens and there's a risk of ventricular arrhythmia
- It also crosses the blood brain barrier with direct toxic effects on the brain and spinal cord
Why is sotalol special?
- Causes blockade of potassium efflux
- This prolongs the QT and risks Torsades de pointes
- Often presents in asystole
- Can have delayed effects up to 24 hours after ingestion
Tell me stuff I don't need to know
Gladly.
- Sotalol comes as a racemate of the l-isomer and d-isomer
- The l-sotalol is the beta blocker, and not a very selective one at that
- The d-sotalol is a class III antiarrhythmic (potassium) and is responsible for the Torsades bit by blocking the delayed rectifier channel that permits timely repolarisation of the myocardium
Pharmacokinetics and dynamics
Let's assume - fairly reasonably one would hope - that the overdose is oral, and the patient hasn't ground up their blood pressure meds and injected them IV/PR/intra-ocularly* for some reason.
- Gastric absorption depends on the formulation (MR vs IR) but is generally fairly quick
- Peak blood concentration usually around 2 - 3 hours after ingestion
- Elimination half lives are vary variable
*I have seen all three of these.
Propranolol
Gets its own box because it's the most dangerous agent, largely because of its ability to cross the blood brain barrier, and its propensity to block sodium channels as well.
It's also one of the most commonly overdosed beta blockers.
- More than 1 or 2 grams is bad news
- Toxic effects will generally be seen within six hours
What it looks like
- Hypotension
- Bradycardia
- AV block
- PR prolongation
- Heart failure
- Cardiac arrest
- Bronchospasm
- Hypoglycaemia - reduced gluconeogenesis
- Hyperkalaemia - reduced insulin
- Drowsy or coma
Sometimes propranolol can look like a sodium channel blocker, because it is.
- Wide QRS
- Arrhythmias
- Seizures - directly enters the CNS and lowers seizure threshold
What to do
It's not particularly tricky really.
Consider activated charcoal if you're looking at the patient within 2 hours of ingestion. You can even cleanse the whole gut with polyethylene glycol if you think they've taken loads of slow-release formulation and you reckon you can flush it out that way.
Airway
- As you would normally - if they can't protect their own airway, do it for them
- If you take enough of anything you can drop your GCS low enough to need a tube
- If you can safely avoid a tube, it allows you to monitor their neurological status more effectively
- Be cautious when intubating - these patients are cardiovascularly delicate
Breathing
- If they have inadequate ventilatory effort - do it for them
err... that's it really
Circulation
- IV access
- Fluid bolus (unless in frank pulmonary oedema)
For bradycardia:
- Atropine (most likely won't do much)
- Adrenaline 10-20 mcg bolus +/- infusion
- Isoprenaline up to 10 mcg/min infusion*
- Pacing - transcutaneous or temporary wire
For hypotension
- Fluid bolus
- Adrenaline as above if hypotensive and bradycardic
- Noradrenaline if primarily vasoplegic
- Insulin and dextrose (see below)
- Calcium as an inotrope
For Torsades
- Magnesium 10 mmol IV over 15 - 20 minutes
- Isoprenaline or pacing to maintain heart rate above 100
For QRS broadening and ventricular arrhythmias
- Sodium bicarbonate 2 mmol/kg IV
- Consider lidocaine
- Do not give amiodarone
Do an ECHO to determine whether the main issue is pump failure or vasodilatation and hypovolaemic shock.
*It's helpful to know what agent was ingested here - if they've had a load of selective B1 blocker, then giving isoprenaline (B2 agonist) for bradycardia is likely to worsen hypotension
Specific treatments
The reflex answer of any savvy exam candidate when asked about beta blocker overdose is 'glucagon', however it's not quite as clear cut as the mark schemes may lead you to believe.
It's still worth mentioning in an exam however.
The truth about glucagon
We don't really know if it does anything useful, but the theory goes as follows:
- Glucagon triggers adenylate cyclase
- This increases cAMP production in cardiac myocytes
- This is essentially the same as activating all the blocked beta receptors
- Hey presto your heart rate, hypotension and lack of gluconeogenesis all magically improve
You give it as an infusion of up to 10 mg/hour IV.
High dose insulin euglycaemic therapy
This is becoming increasingly popular but we don't really know how it works.
- Insulin is a positive inotrope when you give lots of it, probably via its downstream effects on calcium
- It also helps supply sugar to the unhappy cardiac myocytes
- It sensitises everything to catecholamines
- It induces a bit of vasodilatation to help myocardial oxygen supply
The dose is anywhere from 0.5 to 10 unit/kg/hr.
How to do it:
- Bolus of 1 unit per kilogram IV
- If blood sugar <11 mmol/L then give 25g IV glucose at the same time
- Start IV infusion of 0.5 - 1 units/kg/hour
- Increase by 0.5 every 15 minutes until satisfactory response
- At the same time give 0.5 mg/kg/h glucose IV (10-20%) and titrate to keep blood sugar between 6 and 12 mmol/L
Monitor sodium, potassium, acid-base balance and glucose every 15 - 30 minutes until adequate response.
Useful Tweets and Resources
Here's our post on BRASH syndrome

Beta-Blocker Overdose/toxicity:
— Satyendra Dhar, MD SFHM (@DharSaty) January 31, 2024
👉Bradycardia & hypotension (most common).
👉Myocardial depression & cardiogenic shock (severe overdoses).
👉Ventricular dysrhythmias (Common with propranolol & acebutolol).
👉Others (mental status change, seizure, hypoglycemia, & bronchospasm).… pic.twitter.com/Of7ELNv7uR
References and Further Reading



Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.
Anaestheasier® is a registered trademark.