Asthma
Take home messages
- The triad of asthma is bronchoconstriction, airway inflammation, and mucus hypersecretion
- The key killers of intubated asthmatics are tension pneumothorax and dynamic hyperinflation
- Aim for a low respiratory rate, low PEEP and prolonged expiratory time
A case
The decision that scared me most (aside from Rule 10) while working as a core trainee anaesthetist was the 'when do I intubate asthma' conundrum.
- I'd seen some consultants and registrars intubate asthma
- I'd seen other consultants and registrars do everything in their power to avoid it
- I did not have a robust 'definitely intubate at this point' heuristic to comfort me on my lonely ITU night shifts
So when I was called by ED at one in the morning on a Sunday and asked to come and assess whether their tripodding asthma patient needed intubating, I rather bricked it a little.
Reluctantly, I let the ITU nurse in charge know that I was reviewing a possible admission, and dutifully wandered on down to resus.
"Hey thanks for coming, it's the guy in bed three..." the ED registrar at the nurses' station pointed vaguely towards resus while handing an ECG back to the nurse on his left, and picking up the ringing red phone on his left.
Hello bed 3
I took what in retrospect was an insensitively deep breath, and pulled back the curtain to bed 3, wondering whether I was going to have the knowledge and courage to make the correct decision myself, or whether my boss was to receive an unwelcome wake up call.
In front of me lay a slim, pale man in his thirties.
- He was lying flat on his back
- His eyes were closed
- His heart rate was 30
- His respiratory rate was 0
- His chest was silent
- The PaCO2 on the arterial blood gas the nurse handed to me was 20 kPa
- The look on the nurse's face suggested this was all rather recent
Decision made.
What we did
- Big fluid bolus while getting kit and drugs ready
- RSI with ketamine, alfentanil and rocuronium
- Dilute adrenaline (10mcg boluses) as a chaser
- Size 8.5 tube, MAC 3
- Confirmed EtCO2 trace
- Manual chest decompression
- Up to ITU
- Rocuronium and ketamine infusions
He was extubated two days later and discharged home the day after that.
What is it?
Asthma is a chronic, reversible, obstructive airways disease, characterised by chronic inflammation and hyper-responsiveness of the bronchial muscles and mucus hypersecretion.
What are the key features of the pathophysiology of asthma?
- Bronchoconstriction
- Hypersecretion of mucus
- Chronic airway remodeling
The inflammation
The less-than-helpful T helper 2 cells, along with mast cells and B cells all work together to trigger a cascade resulting in release of histamine, leukotrienes and prostaglandins.
What are the characteristic lung function test findings in asthma?
- Obstructive pattern
- Reduced FEV1 and reduced FEV1/FVC ratio (<0.7)
- Reversibility with bronchodilators
- Variable peak flow reading
- Positive direct bronchial challenge test
Who gets it?
Risk factors
- Allergic phenotype (atopic)
- Obesity
- Reflux
- Pollution
- Viral respiratory tract infections
- NSAID use
- Beta blocker use
- Smoking
- Damp or mould
- Pet exposure
Some history
Asthma comes from the Greek ἆσθμα (ásthma), meaning "panting" or "breathlessness."
Hippocrates is thought to have described asthma in around 400 BC as a condition caused by the environment, linking it to dust and city living.
Oh and we also used to think 'asthma cigarettes' where a good idea.
Some actual treatments
Isoprenaline - the first β agonist - was introduced in the 1940s and formulated into an inhaler.
These were revolutionary, to the point where they were overused so much that they started increase mortality again (via their cardiovascular effects) until the slightly more selective salbutamol came along in 1966.
How bad is it?
What medications should be used for acute asthma?
- Oxygen to aim for sats >94%
- Back to back salbutamol nebulisers 2.5 - 5 mg
- Ipratropium nebulisers 500 mcg
- Magnesium sulphate IV 2g over 20 minutes
- Hydrocortisone 100 - 200mg IV or Prednisolone 50mg PO
- Aminophylline 5mg/kg at 25mg/min
- Consider IM adrenaline 0.5mg
When do I get involved?
The anaesthetist isn't called when the patient starts wheezing, they're called when the patient stops wheezing.
This is when you're headed into 'life-threatening' territory, and the patient is exhausted.
You can find the full BTS guidance on how to categorise the severity of an asthma attack here, but for now we'll focus on what's most relevant to us.
What are the features of life-threatening asthma?
- PEFR <33% predicted
- Silent chest
- Normal or raised PaCO2
- Bradycardia
- Arrhythmia
- Hypotension
- Exhaustion
- Confusion or reduced GCS
To tube or not?
This is the tricky bit - making the decision to intubate - because you know that once that tube is in, the real challenge is going to be trying to ventilate.
Imagine ventilating a brick. One that doesn't want to be ventilated. That's what ventilating a good going asthmatic lung feels like.
There are essentially two schools of thought:
- An exhausted asthmatic needs a rest, so intubate them before they get too tired
- Intubation and ventilation is horrific and should be avoided until all other options have been exhausted
The true correct answer is probably somewhere in between. Either way, when you do get your scope and tube out, you need to have a plan.
RSI vs DSI
Nobody is going to criticise you for executing a smooth standard or modified RSI for a life-threatening asthma attack.
They might say something like 'sux releases histamine' but in reality you've done a good job.
But you might want to pause and consider the benefits of a delayed sequence induction with ketamine in asthma.
What are the benefits of ketamine in asthma?
- Bronchodilation via NMDA antagonism
- Maintains cardiovascular stability
- Preserves respiratory drive
- Allows a DSI approach to facilitate monitoring and preoxygenation
My asthma recipe
This is just my way of doing things, once I've identified a patient is in the throes of a life-threatening asthma attack with a rising PaCO2.
It is not the only way to do things, nor is it necessarily the best.
- Ensure big IV access and give at least 500ml fluid bolus
- Give 100 mcg IV salbutamol, if HR <180
- Get everything ready for DSI
- Start BiPAP and give 30-50mg ketamine (bronchodilation, anxiolysis and cooperation)
- Position, apply monitoring and preoxygenate with the BiPAP on 100% FiO2 for 2 minutes
- See if the salbutamol and ketamine have significantly improved the patient's condition and re-assess need for intubation
- Continue to intubation if no improvement
- If substantial improvement then monitor for another ten minutes to see if trajectory continues
The key is constant reassessment, being ready to intubate at a moment's notice, and not getting complacent.
Other bits of interest
- Pulsus paradoxus is a difference of more than 10mmHg between inspiratory and expiratory blood pressures, and it correlates with severity of asthma attack
- The majority of acute asthmatic attacks are viral or allergic in origin and do not require routine antibiotics
- High dose rocuronium (1.2 mg/kg) may help prevent bronchospasm from airway stimulation
- Avoid thiopental as it can induce histamine release and cardiovascular depression
Don't blow it
Ventilating asthma is hard.
The reduced airway calibre massively increases resistance and contributes to gas trapping, while mucus hypersecretion causes plugging and desaturation.
The biggest killer in ventilated asthma patients is dynamic hyperinflation, which is discussed beautifully in the video at the bottom of this post.
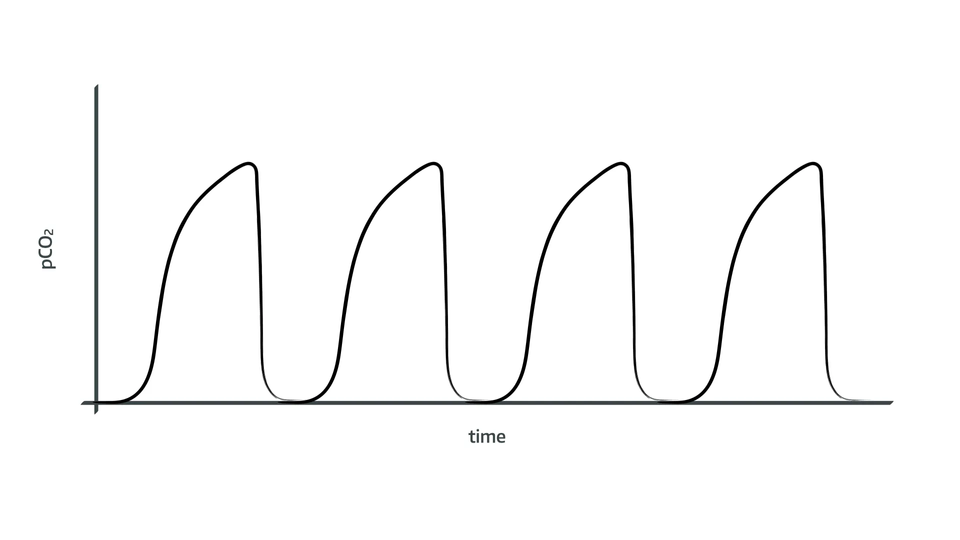
What's dynamic hyperinflation?
- The bronchoconstriction reduces airway diameter
- This increases resistance to airflow
- This makes inspiration harder
- It also makes expiration much slower, leading to gas trapping when the ventilator delivers the next breath too soon
- You can see this on your ventilator flow diagram, as the flow doesn't return to zero before the next breath is delivered
- This needs a much smaller I:E ratio (such as 1:4 or 1.5) to allow that gas to escape
What are the risks?
- Rising intrathoracic pressure → reduced venous return → hypotension and cardiac arrest
- Barotrauma → pneumothorax
- Worsening gas exchange → hypercapnia and hypoxia
What do I do about it?
- Reduce respiratory rate
- Increase expiratory time
- Lower tidal volumes
- Monitor for auto-PEEP
So what settings should I use?
Some sensible numbers to start with are:
- PEEP <5cmH2O
- Resp rate 8 - 10
- I:E ratio at least 1:4 up to 1:8
- Pmax <35cmH2O
- 6 ml/kg IBW Tidal volume
- Permissive hypercapnia
Remember you're aiming to deliver a tidal volume as your priority, even if this requires rather scary pressures.
The pressure is due to airway resistance, rather than poor alveolar compliance, so remember the peak pressures are not what the alveoli are 'feeling', but what the muscular bronchi are pushing back with.
The airway pressures are high and the blood pressure is crashing
You're probably either looking at a tension pneumothorax or dynamic hyperinflation.
- Have a listen both sides and look at the chest expansion
- Look with ultrasound if immediately available and you have the requisite skillset
- If one side quieter and more inflated, consider needle decompression
- If bilaterally hyperinflated then consider detaching from the vent and manually decompressing with firm steady pressure over the anterior chest wall
Either way a fluid bolus is probably a good idea too.
Nothing is working, what do I do now?
Hopefully you called for help a while ago, because assuming you've got everything right up until this point, you really only have four options left:
- IV ketamine +/- rocuronium infusion
- Isoflurane
- Heliox
- ECMO
Can I use BiPAP?
Non-invasive ventilation is weirdly controversial in asthma, given how useful it can be.
This is largely because there isn't much evidence floating around to back up its use, rather than it being actively harmful.
Why use it?
- Assists ventilation without intubation
- Help delivery of nebulised drugs to bronchial muscles
- Preoxygenation prior to intubation
- After extubation to prevent the need for re-intubation*
*Extubating onto high flow nasal oxygen is also a good option.
When should I consider NIV?
- No contraindications to NIV
- Patient not needing immediate intubation
- Respiratory rate >25
- Heart rate >110
- Increased work of breathing
- Increased oxygen requirement
- FEV1 <50% predicted
What settings should I use?
This is clearly going to vary massively between patients, however a sensible starting point might look like:
- iPAP 8 - 16 cmH2O
- PEEP 4 cmH2O
- Low I:E ratio (1:4)
- Increased expiratory time
You're aiming to supplement their work of breathing, achieve a reasonable tidal volume of 6 - 10 ml/kg and a low enough respiratory rate that they can actually exhale some gas.
When should I avoid NIV?
- Low GCS
- Vomiting
- Claustrophobic
- Agitated
- Lots of secretions
- Cardiovascularly unstable
These patients generally just need intubating.
The Verdict
Consider BiPAP to buy time and preoxygenate while you get ready to intubate, but don't rely on it as a definitive strategy by itself, and don't let it delay intubation.
Here's an awesome LITFL video
Video link if the embed doesn't work.
Useful Tweets
A 17-year-old boy was rushed to the ER by his brothers struggling to breathe...
— Sam Ghali, M.D. (@EM_RESUS) November 10, 2019
[thread]
This is what vocal cord dysfunction looks like in a 25 year old female w/severe #asthma & multiple #intubations! (Thnx @KapwingApp for editing help)#FOAMed #FOAMcc #MedEd #medtwitter #Glidescope@airwaycam @emcrit @EM_RESUS @EMSwami @CriticalCareNow @emresidents @AnesthCritCare pic.twitter.com/NvG0rEvfqf
— Mark Ramzy, DO, EMT-P (@MRamzyDO) January 18, 2019
Asthma - IBCC chapter & cast (by @PulmCrit & @adamdavidthomas) https://t.co/zjg9P25JT9 pic.twitter.com/y9aXBuH1Y3
— the EMCrit Crew (@emcrit) October 8, 2019
References and Further Reading



Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!