APACHE II and scoring systems

Take home messages
- Scoring systems can be useful tools in guiding patient management
- Don't make decisions based on a single number
- The scoring system may not be calibrated to your specific cohort or patient type
- Scoring systems won't tell you whether admission to ICU is appropriate
Why have scoring systems?
Making decisions is difficult in general, and it's even harder on ICU when relatively small decisions can have profound consequences for a patient's resulting quality of life.
Back in the good old days, when doctors looked like this...
...you could get away with doing pretty much anything you wanted by just calling it medicine, regardless of whether it actually helped the patient or not. A lot of the time, it really didn't.
Drain some blood, stick on a few leeches, burn some herbs and if that doesn't work, just blame it on witchcraft
Then in 1863 along came Florence Nightingale who decided we should probably at least try and work out if what we're doing is working, and the era of outcomes, mortality ratings and severity scores began.
Since then there have been a number of scales, scores and calculators available to help you work out just how sick your patient is, and what you should do with them.



There are three types of scoring system:
- Severity scores - e.g. Sequential Organ Failure Assessment (SOFA)
- Outcome predictors - e.g. Acute Physiology and Chronic Health Evaluation (APACHE)
- Decision-support tools - e.g. National Early Warning Score (NEWS)
Some of these scores are used for comparing outcomes between different intensive care units, in order to assess quality of care provision.
APACHE II
Most of us can look at a patient and get a bit of a gut feeling for whether they're likely to pull through or not, but as you can imagine that's wildly variable and not exactly bulletproof when it comes to making important decisions with family members regarding their loved one's care.

While no scoring system is ever bulletproof either, it can add a fair bit of weight to your decision either way if you can reliably put a number on a patient's likely outcome, and that's where the APACHE II score aims to help.
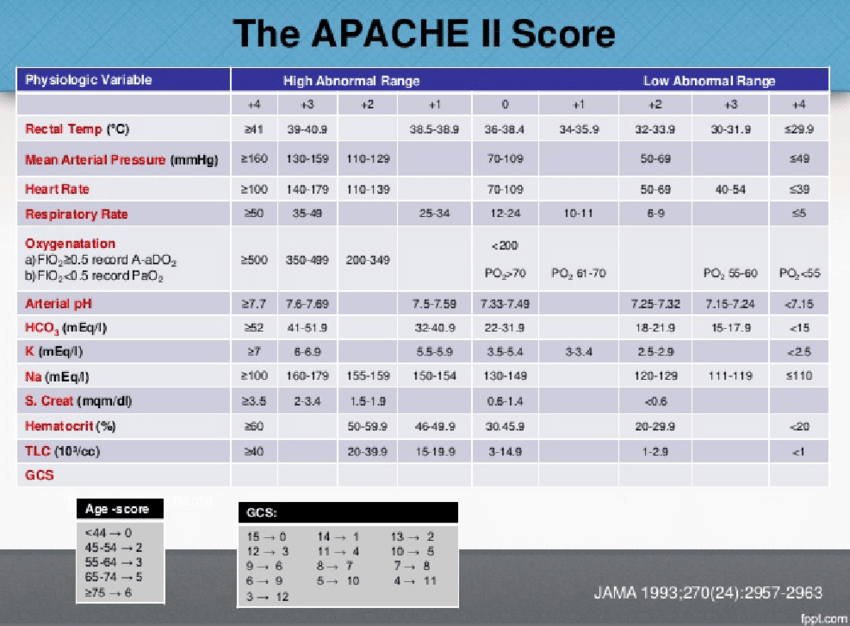
APACHE II
- Replaced APACHE I in 1985
- Acute physiology and chronic health evaluation
- Assesses severity of illness on admission to ICU
- 12 physiological variables + points for age + chronic health conditions
- (17 in total)
- There is now APACHE IV since 2006, but it measures 142 variables so isn't overly approachable in clinical practice
Physiological parameters assessed by APACHE II
Cardiovascular
- Temperature
- MAP
- Heart rate
Respiratory
- Respiratory rate
- Oxygenation*
Metabolic
- pH
- Sodium
- Potassium
- Creatinine
Haematological
- Haematocrit
- White cell count
*For oxygenation, use A-a gradient if FiO2 >50%, and PAO2 if FiO2 <50%
- Note that this score was derived from a general ICU population, and will not necessarily be accurate for specialist patients such as liver or neuro ICU
- Unlike decision support tools, the score doesn't affect management, it just gives an idea of likely outcome, which can be useful for assessing baseline risk when conducting research trials, and for determining likely prognosis when discussing treatment options and progress with family members
- Use the worst value from the last 24 hours
SOFA and q-SOFA
It's rather concerning that nobody really knows what sepsis is, and as a result the definition changes on a fairly regular basis.
The latest official definition is as follows:
Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection

Furthermore, sepsis should now be diagnosed in conjuction with SOFA assessment
SOFA score
- Assesses dysfunction of 6 organ systems
- Each can score between 0 and 4 points
- Max score 24
- Worst value over 24 hours used
- Includes a treatment variable (vasopressor dose)
- An increase in SOFA score of 2 or more carries a 10% increased mortality risk
Systems assessed by SOFA
- Respiratory
- Cardiovascular
- Coagulation
- Liver
- CNS
- Renal
q-SOFA is a more user-friendly version with only three criteria
q-SOFA variables
- Respiratory rate 22/min or higher
- Altered mentation
- Systolic BP 100mHg or less
Patients with two or three of these criteria have higher risk of worse outcome
This system actually works pretty well, and is probably more specific than relying on SIRS criteria that could easily be due to autoimmune or other non-infectious pathologies.
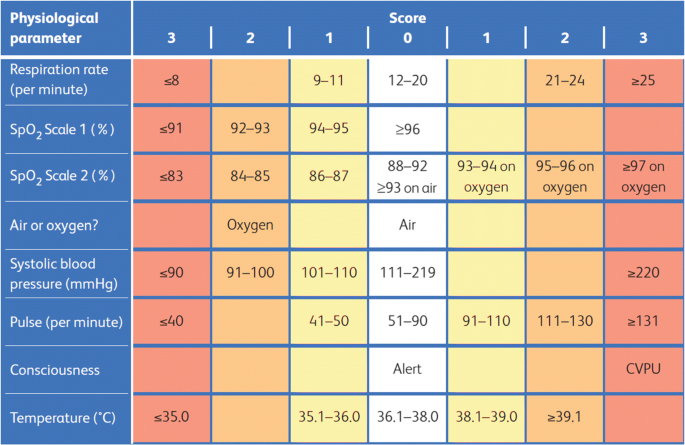
NEWs Score
Love it or hate it, the NEWs score has been widely implemented throughout hospitals in the UK, and to be fair, it works pretty well for a lot of patients.
The benefits are that it provides or at least suggests a standardised response that any staff member can being instigating, in the event of a patient's deterioration.
While it won't get it right all the time, it's very good at highlighting which patients need the on call F1, and which ones the ICU registrar should probably take a look at.
One of the key downsides is that it doesn't account for underlying illness, so patients on home oxygen with a respiratory rate of 30 at baseline end up receiving an inordinate amount of blood pressure readings overnight.

To sum up
- Scoring systems are helpful, but only as tools used in conjunction with your clinical judgement and experience
- As populations change, scoring systems need to adapt
- Our population is becoming increasingly elderly and more frail
- As more and more data becomes available, with more computing power, we can use more complicated and comprehensive scoring systems to provide more accurate predictions
Useful Tweets
“An updated “norepinephrine equivalent” score in intensive care as a marker of shock severity.” #FOAMcc #FOAMed #EMCCM #MedEd #Vasopressors #Shock #Norepinephrine #ICU #Pharmacotherapy #pharmacology
— Syed Shahrul Naz (@drshahrul80) January 21, 2023
🔗 https://t.co/GfNU5E7GXP pic.twitter.com/RDcCyFzvLf
qSOFA = H A T
— Suman Biswas ♬ 🐀 (@amateursuman) February 23, 2016
1) Hypotension (SBP≤100),
2) Altered mental state (GCS≤13)
3)Tachpnoea (RR≥22)
Sepsis = infection + qSOFA score of 2 or 3
References and Further Reading