Antiemetics and PONV
Take home messages
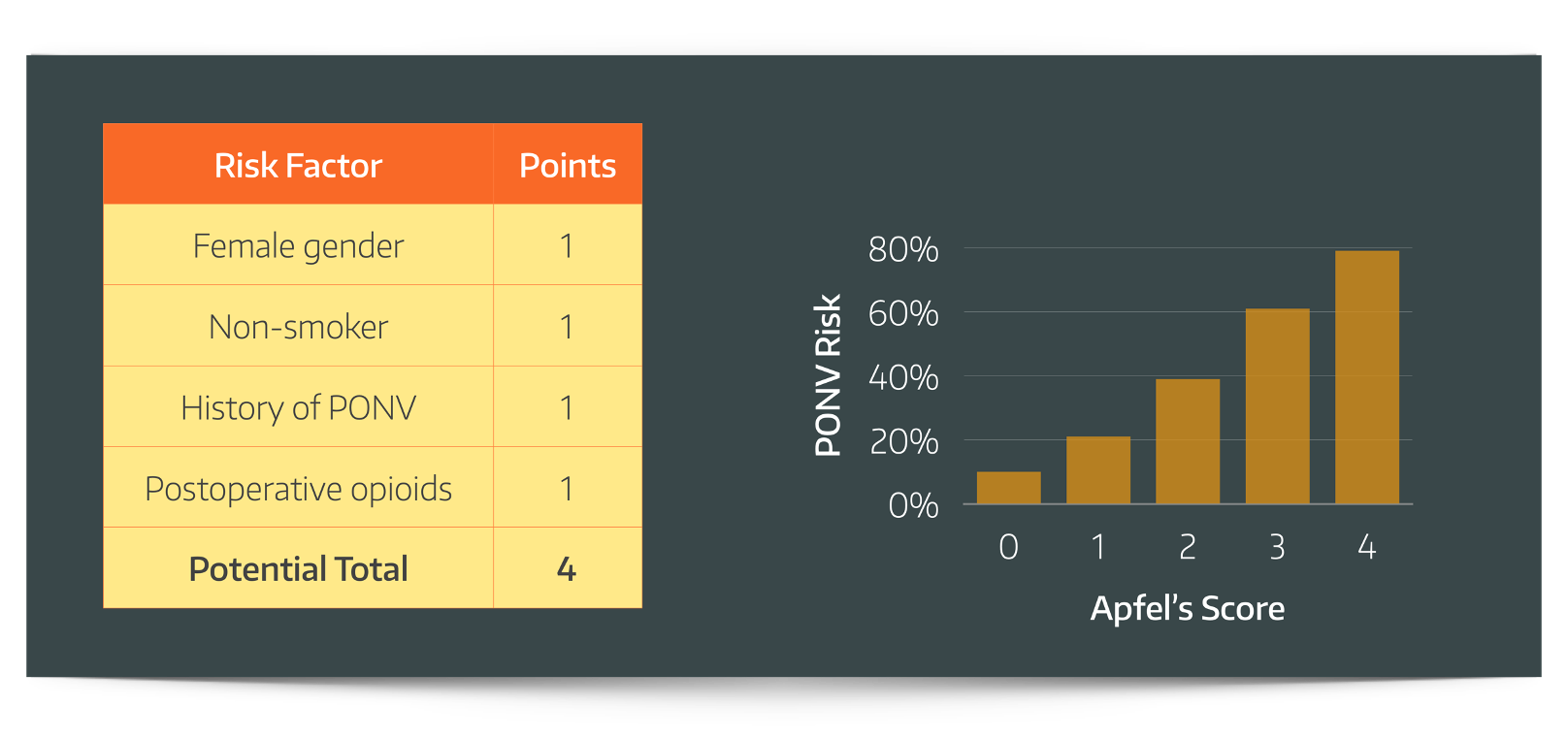
- Use the Apfel score
- Be generous with your antiemetics when required
- Choose your receptor - antihistamines work better for motion sickness
- Low-risk patients may not need them as the NNT is close to the number needed to harm (NNH)
Nausea sucks
And vomiting is even worse, especially on an empty stomach, and even more so if you've just had a four hour hiatus hernia repair.
What are the implications of post operative nausea and vomiting?
- Patient dissatisfaction
- Pain
- Wound dehiscence
- Bleeding
- Aspiration
- Dehydration
- Electrolyte disturbance
- Delayed discharge
- Slower recovery
Also angry surgeon.
Who tends to get it?
Of course anyone can feel nauseated after an operation, but as always there are risk factors that tend to make it more likely.
These can be categorised as anaesthetic, patient and surgical factors.
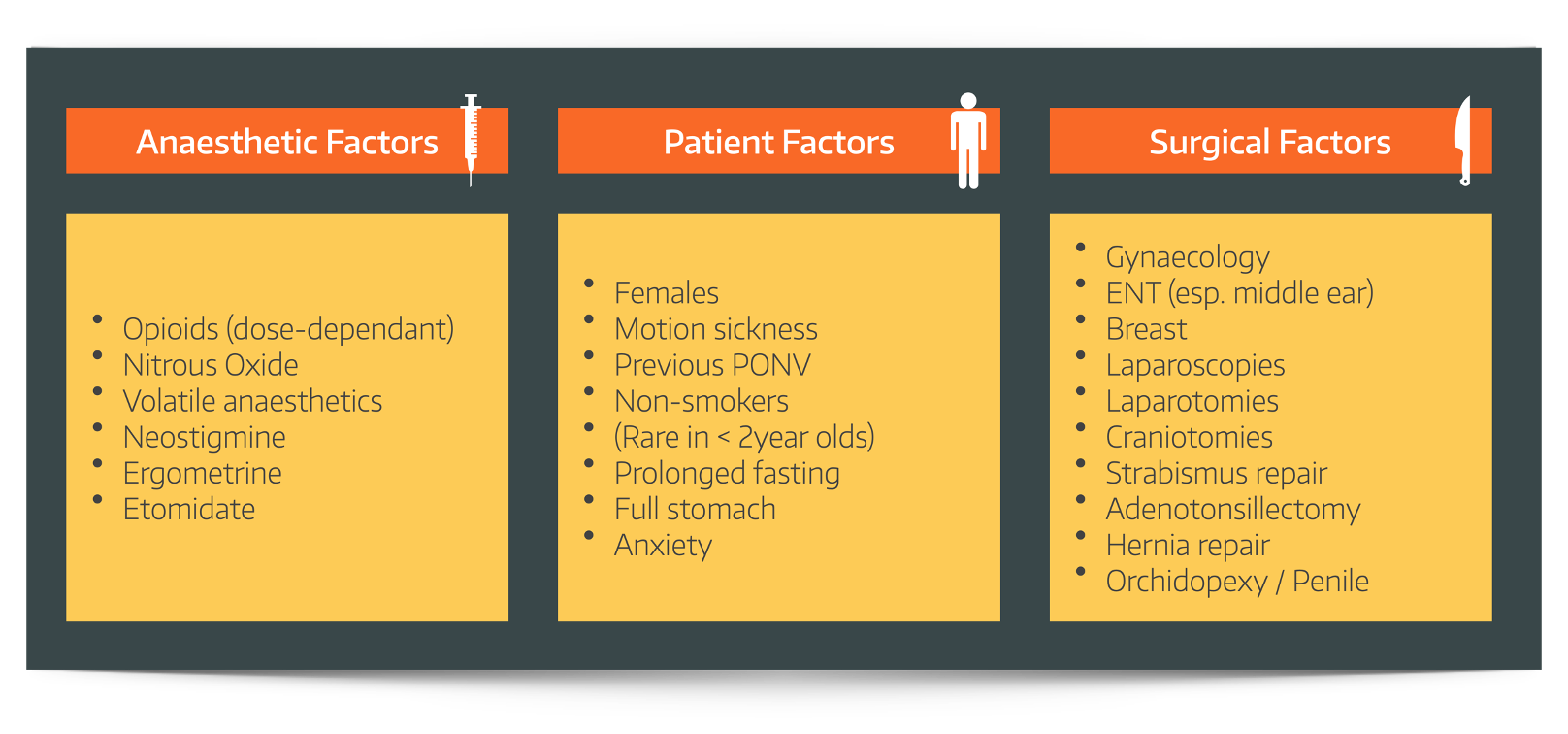
There a few risk factors in particular that are so reliable they have been collated into their own APFEL score:
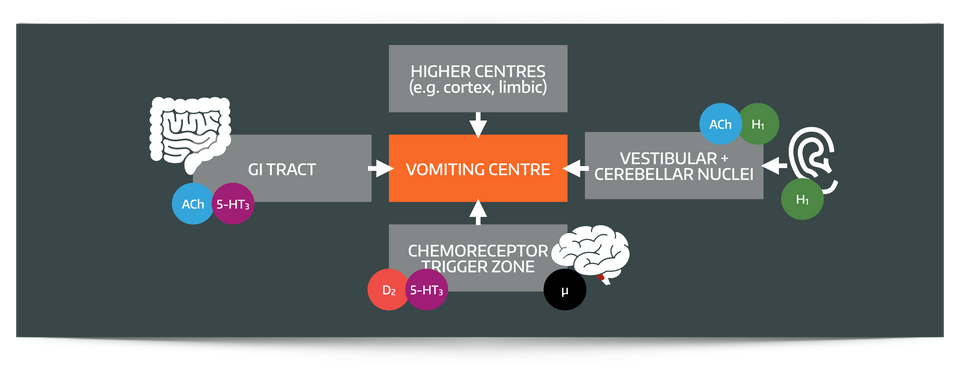
What is the vomiting centre?
- The vomiting centre is the neurological control centre for the vomiting reflex, which is located in the medulla
- It is thought to be a distributed group of neurons forming a central pattern generator rather than a distinct anatomical site
What are the main inputs to the vomiting centre?
The vomiting centre has four main inputs
- The chemoreceptor trigger zone (most triggers)
- Cerebellum and vestibular system (motion sickness)
- Higher centres (fear, disgust, anxiety)
- Solitary tract nucleus (GI tract toxins and distension)
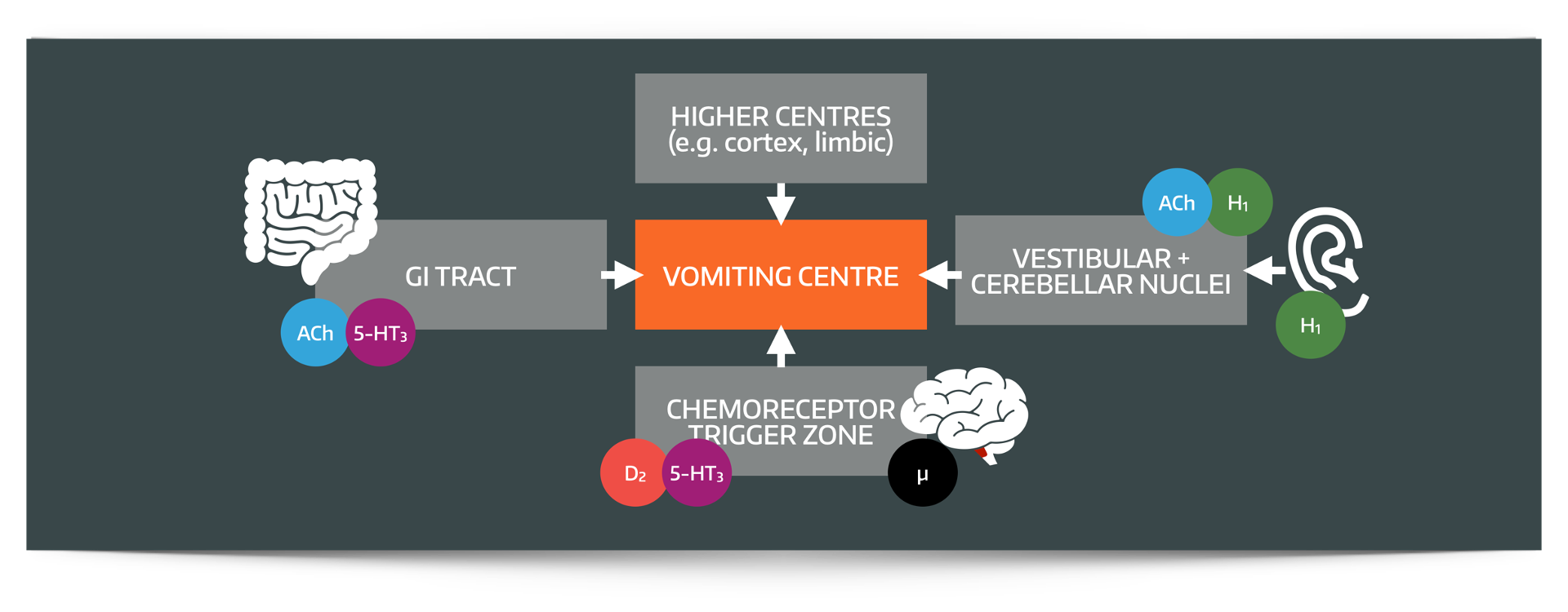
What is the chemoreceptor trigger zone?
No post on antiemetics and vomiting would be complete without at least mentioning the CTZ
- The chemoreceptor trigger zone (CTZ) also known as the area postrema, is a circumventricular organ found in the dorsal surface of the medulla oblongata, on the floor of the fourth ventricle
The crucial point is that it lies outside the blood brain barrier, meaning it is privy to the goings-on in the blood to which other areas of the brain remain blissfully naive.
It then relays that information to the vomiting centre, which can the do the dirty business of coordinating the vomiting response.
The chemoreceptor trigger zone has many receptors
- Mu (opioid)
- D2 (dopamine)
- 5HT-3 (serotonin)
- Kappa (opioid)
- NK1 (neurokinin-1)
- H1 and H2 (histamine)
Given evolutionarily speaking, vomiting is one of the single greatest life-saving reflexes - it makes sense to have a CTZ that can detect all sorts of different poisons.
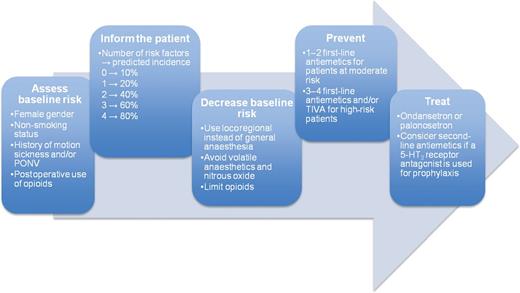
So how can we fix it?
There's a three step method to preventing and treating post operative nausea and vomiting:
- Identify your at risk patients (history and Apfel score)
- Reduce anaesthetic triggers (volatiles, nitrous, opioids)
- Treat early with effective antiemetics
What are the different types of anti-emetic that you know?
Anti-emetics can be classified by the predominant receptor that they target
- 5HT3 receptor antagonists - ondansetron
- Anti-histamines - cyclizine
- Dopamine anatagonists - metoclopramide, domperidone, prochlorperazine
- Antimuscarinics - via the M3 receptor - Hyoscine
- Neurokinin-1 antagonists - aprepitant
- Other - dexamethasone, propofol
Ondansetron
The GOAT.
Originally licensed only for chemotherapy associated nausea and vomiting, now widely used for prevention and treatment of post-operative nausea and vomiting.
As always, structure your response in a consistent manner when describing drugs:
Structure and class
- The molecule is a synthetic carbazole
Dose
- 4-8mg in adults up to TDS or 0.1 - 0.15mg/kg in children
Mechanism of action
- It has peripheral effects via serotonin receptors in the GI tract and central effects in the CTZ
Pharmacokinetics
Absorption
- 60% oral bioavailability
Distribution
- 75% protein bound
Metabolism
- Hepatic
- Inactive metabolites
- Reduced dose if hepatic impairment
Excretion
- Renal excretion
Side effects
- Constipation
- Bradycardia
- Headache and flushing particularly if given quickly IV
- Has been reported to cause extrapyramidal side effects
- Often avoided in long QT syndrome, but unlikely to have any significant effect at clinical dosese
Cyclizine
I tend to hold off on the cyclizine unless I need it, because it can give a bit of a tachycardia and make people feel woozy and strange, but it does work very well.
On more than one occasion, cyclizine's tachycardia has been helpful in bradycardic patients undergoing gynae surgery, offsetting the vagal stimulation rather nicely.
Structure
- Piperazine derivative
Dose
- 25-50mg every eight hours in adults, and 0.1mg/kg in children
Mechanism of action
- H1 antagonism
- Mainly vestibular and cerebellar in action but also some antimuscarinic activity
Pharmacokinetics
- Hepatic metabolism and renal excretion
Side effects
- Tachycardia
- Dry mouth
- Drowsiness
- Blurred vision
- Increased lower oesophageal sphincter tone
Others you might get asked about
Prochlorperazine
Structure
- Phenothiazine neuroleptic (antipsychotic)
Mechanism of action
- D2 antagonist, mainly on chemoreceptor trigger zone
- Dose
- 12.5mg IM (adults)
Side effects
- Increased QTc interval
- Venous thromboembolism
- Neuroleptic malignant syndrome
- Lower seizure threshold
- Parkinsonism
- Oculogyric crisis
- Dry mouth
- Pharmacokinetics
- Hepatic metabolism and renal excretion
Hyoscine
Structure
- Only L-hyoscine is pharmacologically active
Mechanism of action
- Antimuscuranic effects in vomiting centre and vestibular system
Side effects
- Sedation
- Central anticholinergic syndrome
- Agitation
- Drowsiness
- Hallucinations
- Ataxia
- Very dry mouth
Aprepitant
Mechanism of action
- Central action in the vomiting centre on neurokinin-1 receptors, inhibiting the emetogenic effects of substance P
Side effects
- Fatigue
- Hiccups
- Loss of appetitie
- Alopecia
Metoclopramide
Mechanism of action
- D2 receptor antagonism at CTZ
- 5HT3 receptor antagonism
Effects and side effects
- Prokinetic effect on stomach
- Crosses the blood brain barrier
- Extrapyramidal side effects
- Oculogyric crisis
- Dystonia
- More common in young women and elderly
Dexamethasone
Structure
- Synthetic glucocorticoid
Mechanism of action
- Acts on nuclear glucocorticoid receptors but unclear exact pathway, possibly via stimulation of appetite
- This may reduce release of serotonin from the GI tract
- Potentially reduced permeability of blood brain barrier
- Possibly reduced production of arachidonic acid
Dose
- 4-8mg (adults)
- 0.1mg/kg in children
Side effects
- Deranged blood glucose in poorly controlled diabetic patients
Key Pharmacokinetics
- Renal excretion
Other options
Acupuncture
So according to a Cochrane review, acupuncture genuinely works in preventing PONV.
The needling point is called Pericardium 6.
It is approximately 3-4cm proximal to the distal wrist skin crease (i.e. nowhere near the pericardium) between the tendons of FCR and PL.
The patient needs to be awake for it to work, and it has zero side effects, assuming you know what you're doing with the needles.
Cannabinoids
- Nabilone and abalone are a synthetic cannabinoid agent used to treat nausea and vomiting associated with chemotherapy
- Targets CB1 and CB2 cannabinoid receptors
Side-effects
- Dizziness
- Drowsiness
- Dry mouth
- Psychotic reactions
- Hypotension
- Tachycardia.
Don't forget Propofol
Our favourite hypnotic comes to the rescue once again, with its rather impressive antiemetic properties.
It's very useful in the form of TIVA when a patient is known to suffer from post-operative nausea and vomiting. This is especially true if you combine it with regional anaesthesia and use TCI sedation rather than full blown general anaesthesia.
You can use it in subhypnotic doses if you're really struggling to get on top of a patient's vomiting and you're all out of other options.
So what should I give?
A general recipe for a standard operation in an adult patient may look something like this:
- Ondansetron 4-8mg and dexamethasone 6.6mg at induction, unless no risk factors or poorly controlled diabetes
- Cyclizine 25-50mg if more than 2 Apfel points, or already bradycardic and emetogenic surgery
Then for post operative prescription:
- Regular ondansetron for 24 - 48 hours
- PRN cyclizine
- PRN metoclopramide if high risk
Here's our free antiemetic drug summary
Here's our video on the vomiting reflex
Here's a 38 second recap on anti emetics
Syllabus
- PB_BK_77 Nausea and vomiting
Useful Tweets and Resources
FREE TO VIEW
— British Journal of Anaesthesia (@BJAJournals) June 25, 2023
Do longer-acting anti-emetics prevent post-discharge PONV in #DayCase patients? Moraitis et al present a new #openaccess placebo-controlled trial. #Anaesthesia #PONV #Perioperative #AmbulatorySurgeryhttps://t.co/4BHjJyxABM pic.twitter.com/SC6UCsV2qP
A UK hospital has safely treated more than 30,000 patients allowing unrestricted clear fluid until the time of operation. Improved patient satisfaction, reduction in post op nausea and vomiting.
— Dr Helgi (@doctorhelgi) March 7, 2019
Let’s top saying “nil by mouth from midnight”, and allow our patients to drink. https://t.co/LeXPZhu3HI
Dr Chris Hellyar over at gasnovice.com has kindly given us permission to share his wonderful infographic and video below:
References and Further Reading
Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.
