Airway equipment library

It's rather frustrating, during an exam, being handed a piece of equipment you've never seen in your life and asked many invasive questions about what it is and how it works.
So here we're compiling a catalogue of examinable airway equipment that you might get handed to discuss in an OSCE or SOE scenario, so at least you've seen it before.
Underneath each piece of equipment we've included all the buzzwords and phrases you should mention in the exam.
Facemasks
Anaesthetic facemasks are different to ward masks as they form an airtight seal (when used properly) allowing the user to ventilate the patient, as well as provide supplemental oxygen.
Pretty much all masks used in the UK are disposable.
Adult anaesthetic facemask

Key Points
- Disposable, single use adult facemask
- Used for preoxygenation and facemask ventilation
- Forms airtight seal, but this can be difficult in patients with abnormal facial anatomy, beards or no teeth
- Connects to breathing system via 22mm standard connector, usually via an angle piece
- Can make patients claustrophobic, so it's often a good idea to let the patient hold it themselves during preoxygenation
Neonatal facemask

Key Points
- Soft circular silicone ring to fit small anatomy of newborn baby
- Also very useful for ventilating through a tracheostomy or laryngectomy stoma in an emergency
Airway Adjuncts
These nifty bits of kit simply hold the upper airways open to facilitate ventilation - spontaneous or mechanical - and can be very helpful in a tricky airway.
Nasopharyngeal Airway
Key Points
- Holds nasopharynx open to facilitate air entry to hypopharynx
- Can also be used to allow passage of suction catheter to suction pharyngeal secretions
- Passed through the nostril into the posterior pharynx
- Slide the tube postero-caudally along the nasal floor (not cephalad)
- Does not stimulate gag reflex so helpful for semi-conscious patients who will not tolerate an oropharyngeal airway
- Consists of a soft plastic tubing with a flange at the proximal end to prevent inadvertent loss of device into patient’s airway
- There are various ways to size the nasopharyngeal airway: some advocate sizing the width of the tube to the width of the patient’s 5th finger
- Absolutely contraindicated in: (suspected) base of skull fractures and naso/oro-pharyngeal & facial trauma
Oropharyngeal Airway (‘Guedel’)
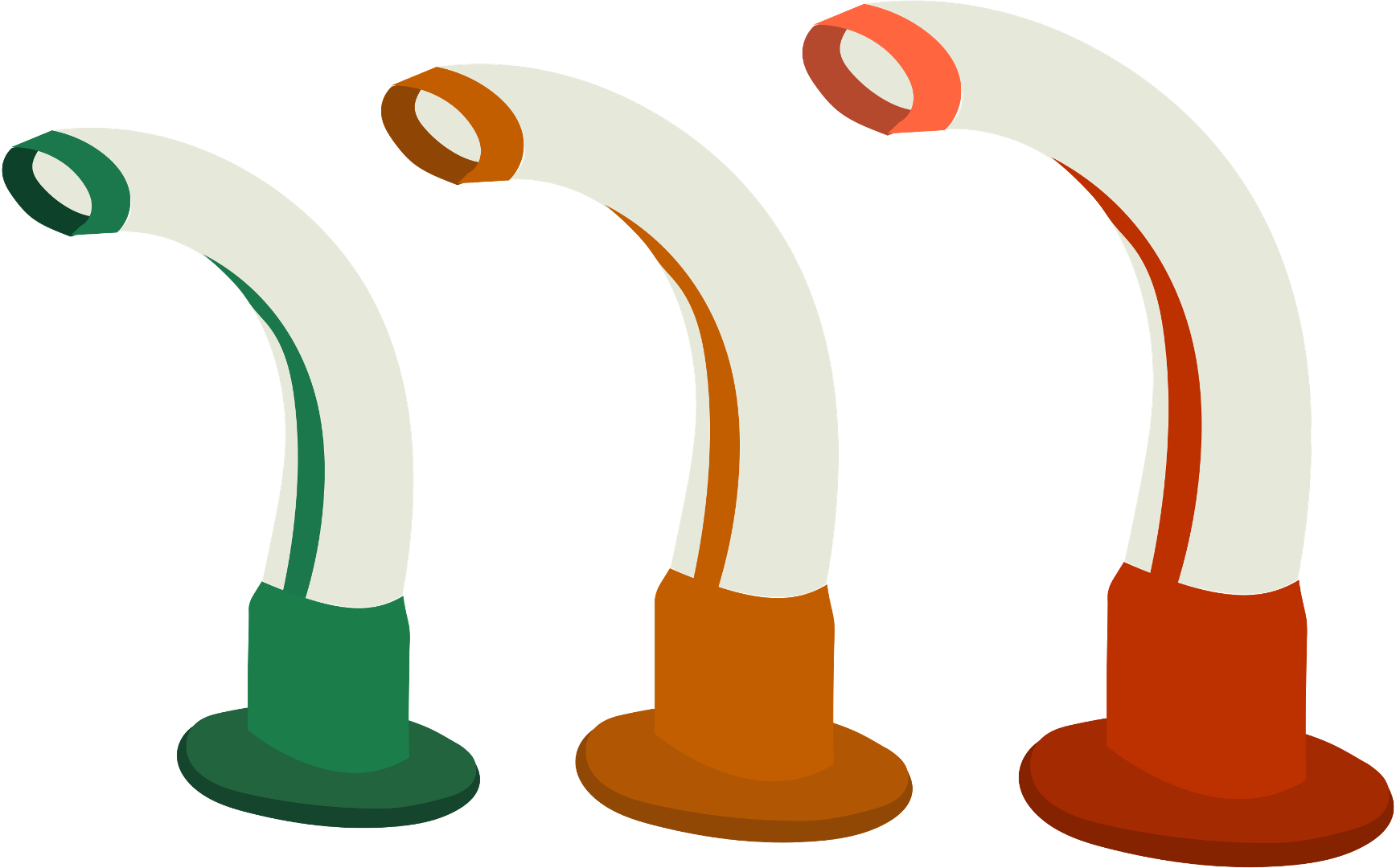

Key Points
- Passed through the mouth into the posterior pharynx to hold the mouth open and pull the tongue forward to prevent it covering the epiglottis
- Sized by measuring from the angle of the mandible to the incisors (usually green for women, orange for men, red for large men)
- Stimulates a gag reflex and so may not be tolerated well by semi-conscious patients
- Very easy to use but needs to be correctly sized - too long and it'll push the epiglottis down over the glottis, too short and it won't reach the base of the tongue
Supraglottic Airway Devices
As you might suspect from the name, these bits of kit sit above the glottis, forming a seal in the hypopharynx to allow ventilation of the patient as well as preventing upper airway obstruction.
They provide some airway protection but they are by no means a 'definitive' airway.
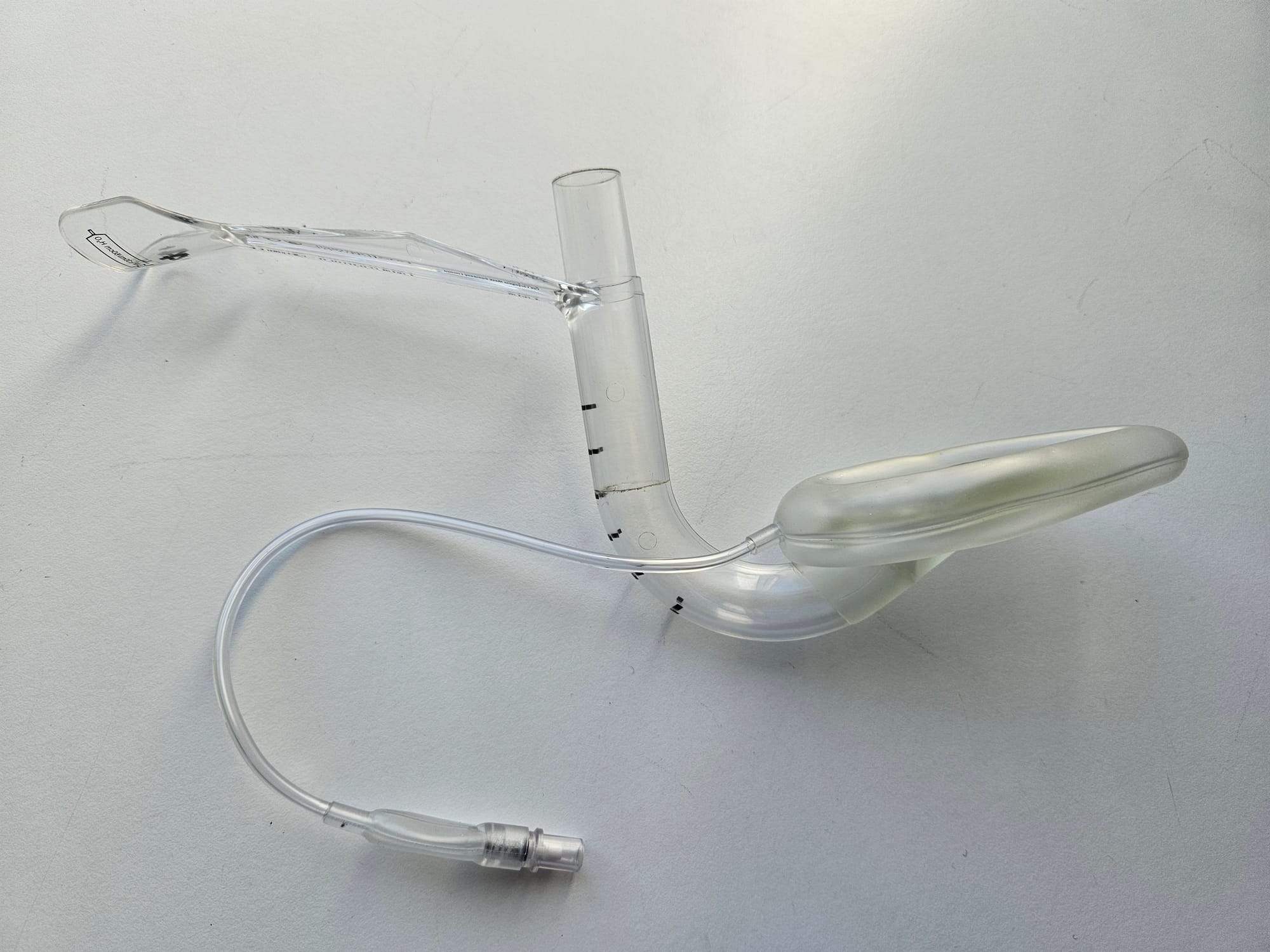
Laryngeal Mask Airway
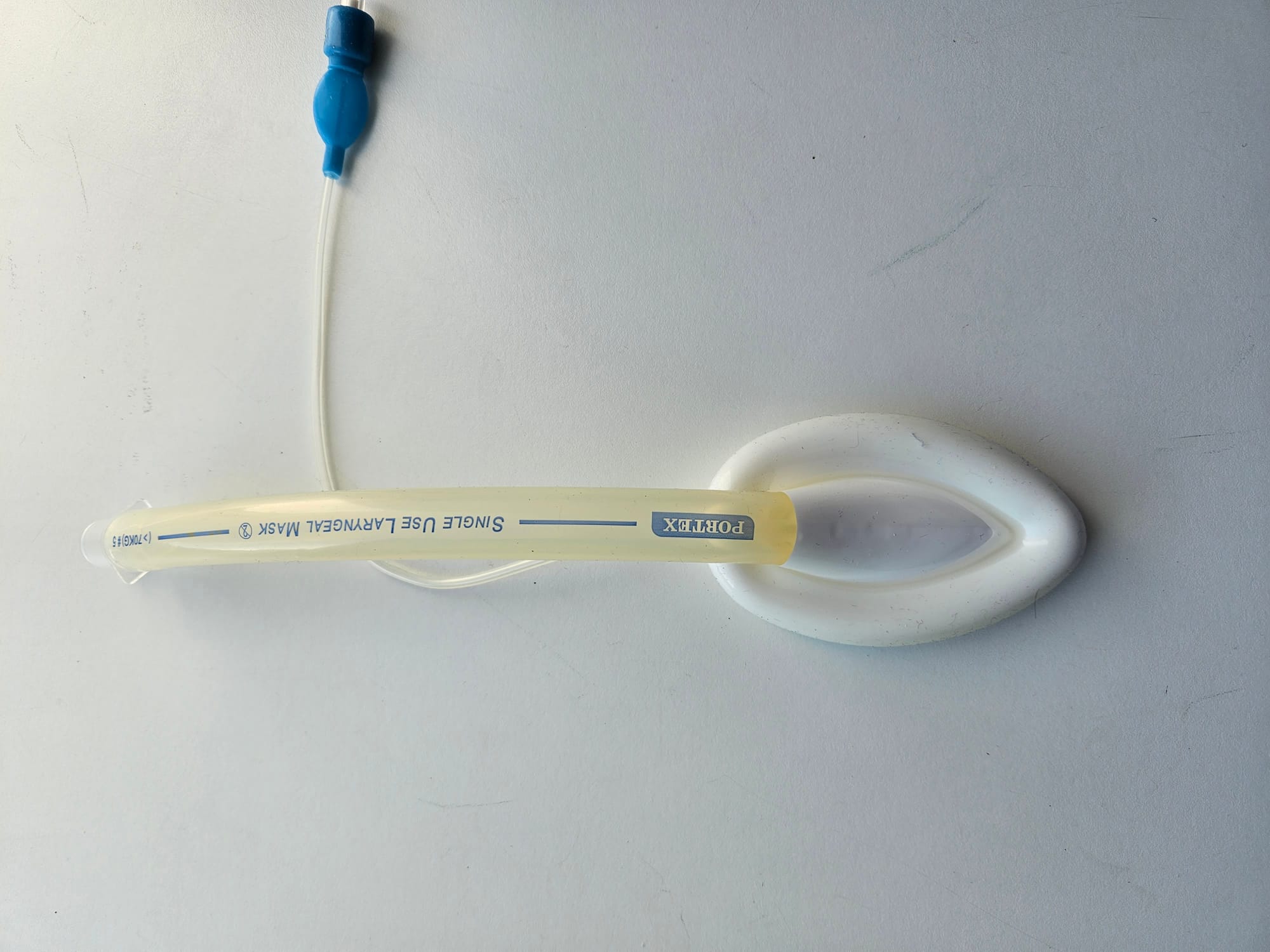
Key Points
- First generation supraglottic airway device invented by Dr Archie Brain in 1988
- Can be single use or reusable (vast majority are single use now as sterilisation doesn't inactivate prions)
- Used for ventilation in low risk elective anaesthesia in fasted patients with no significant reflux
- Also used as a rescue airway device in the unanticipated difficult airway
- Can be used to facilitate intubation, either blind or under bronchoscopy, depending on whether the airway tube has bars at the patient end
Components
- Flexible airway tube
- 15 mm connector
- Inflatable pharyngeal cuff designed to create a seal to faciliate ventilation and provide a degree of airway protection from secretions
- Pilot balloon to inflate cuff with 20-40mL of air
How to insert
- Deflate the cuff and lubricate the back of the mask
- Push the mask posteriorly along the contour of the hard palate
- Use index finger to guide the mask down posterior pharynx
- Continue inserting until resistance met
- Remove finger and inflate cuff - the solid line on the tube should be in the centre
The good and the bad
- Easy to insert
- No need for muscle relaxation
- Much less stimulating than intubation
- Can transfer to recovery before extubation (hospital policy dependent)
- Generally works very well
However
- Doesn't properly protect the airway
- Can cause laryngospasm
- No bite block
- Doesn't always form a reliable seal
- Low ventilatory pressure limit of around 20cmH2O
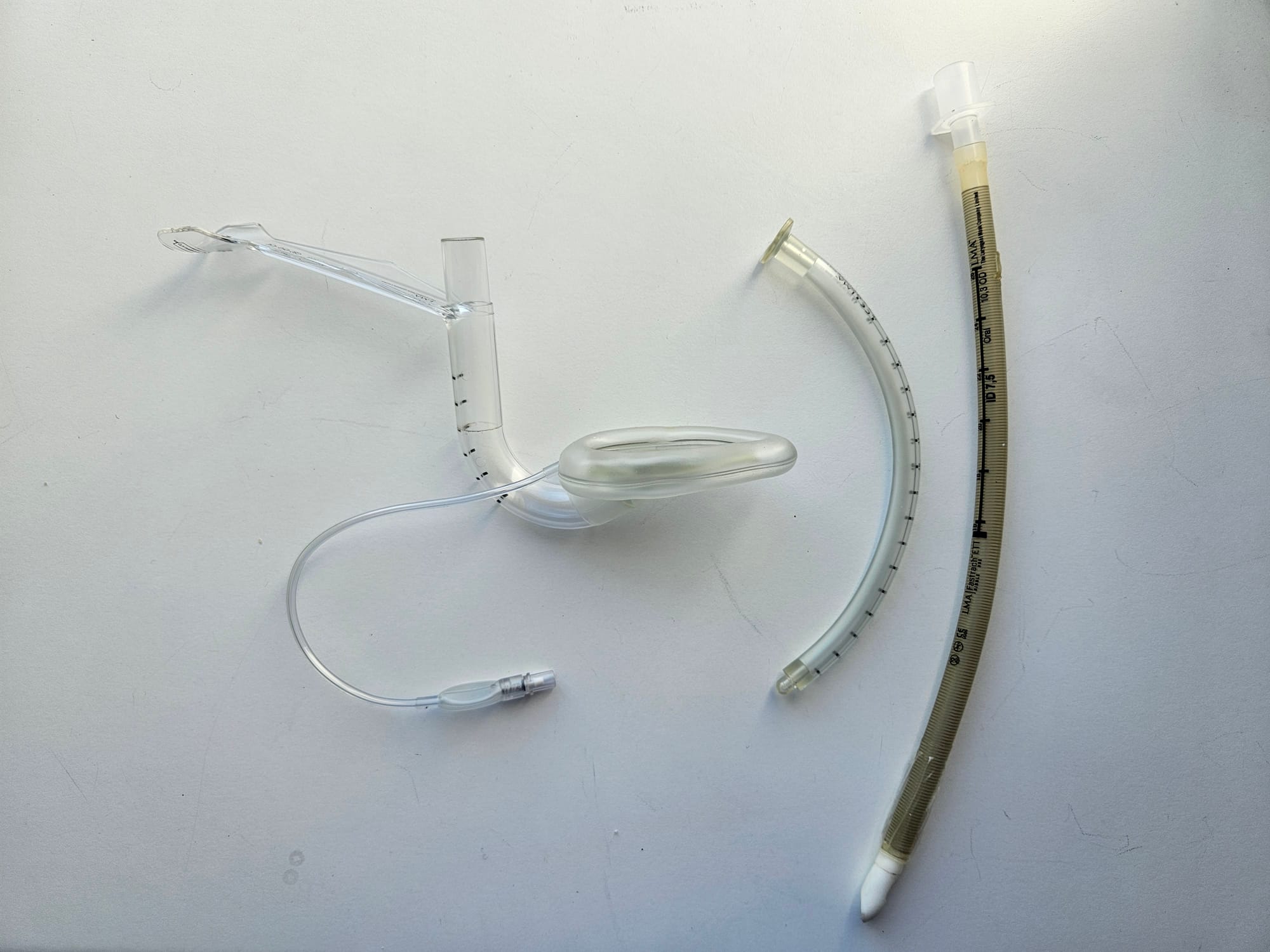
Reinforced LMA
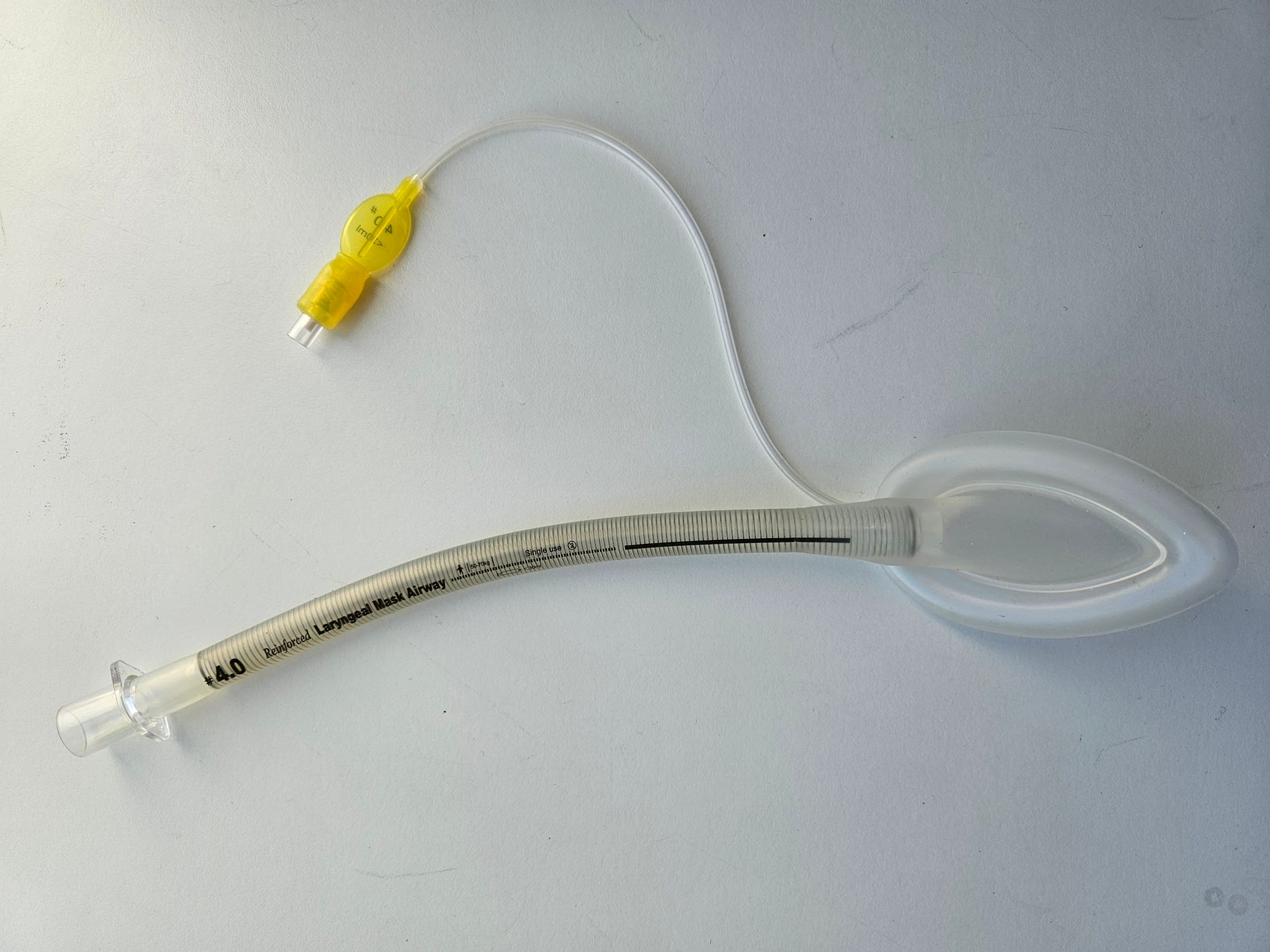
Key Points
- Often referred to as a 'flexi' LMA
- All the features of a standard first generation LMA but with the added zing of a metal spiral to provide structural integrity to the airway tube
- This prevents kinking when the tube is bent to more sporting angles, making it ideal for oral and pharyngeal surgery
- Larger cuff than endotracheal tube can catch blood and secretions, reducing the likelihood of laryngospasm
- However if the patient bites it, it will deform and remain pinched, potentially causing ventilatory compromise
2nd Generation Supraglottic Airway Devices
iGel


Key Points
- Laryngeal mask is not an inflatable cuff but is a thermoplastic elastomer that moulds to the patient’s warm airway to generate a seal
- Integrated bite block
- Gastric port opens at the oesophageal inlet to allow stomach contents to pass (+/- aspiration with gastric tube)
- Seal pressure is usually greater than first Generation devices, allowing for use of higher peak airway pressures
- Generally sits better in patients with abnormal facial anatomy or missing teeth than other LMAs
LMA Supreme

Key Points
- Single use, second generation supraglottic airway device with two seals (Oropharyngeal Seal + Oesophageal Seal)
- Integrated bite block
- Gastric port to allow passage of orogastric tube and to reduce insufflation of the stomach
- Inflatable cuff
- Larger gastric port and inflatable cuff potentially offer more airway protection and allow greater ventilatory pressures than a first generation LMA (up to 25-30 cmH2O)
Intubating LMA
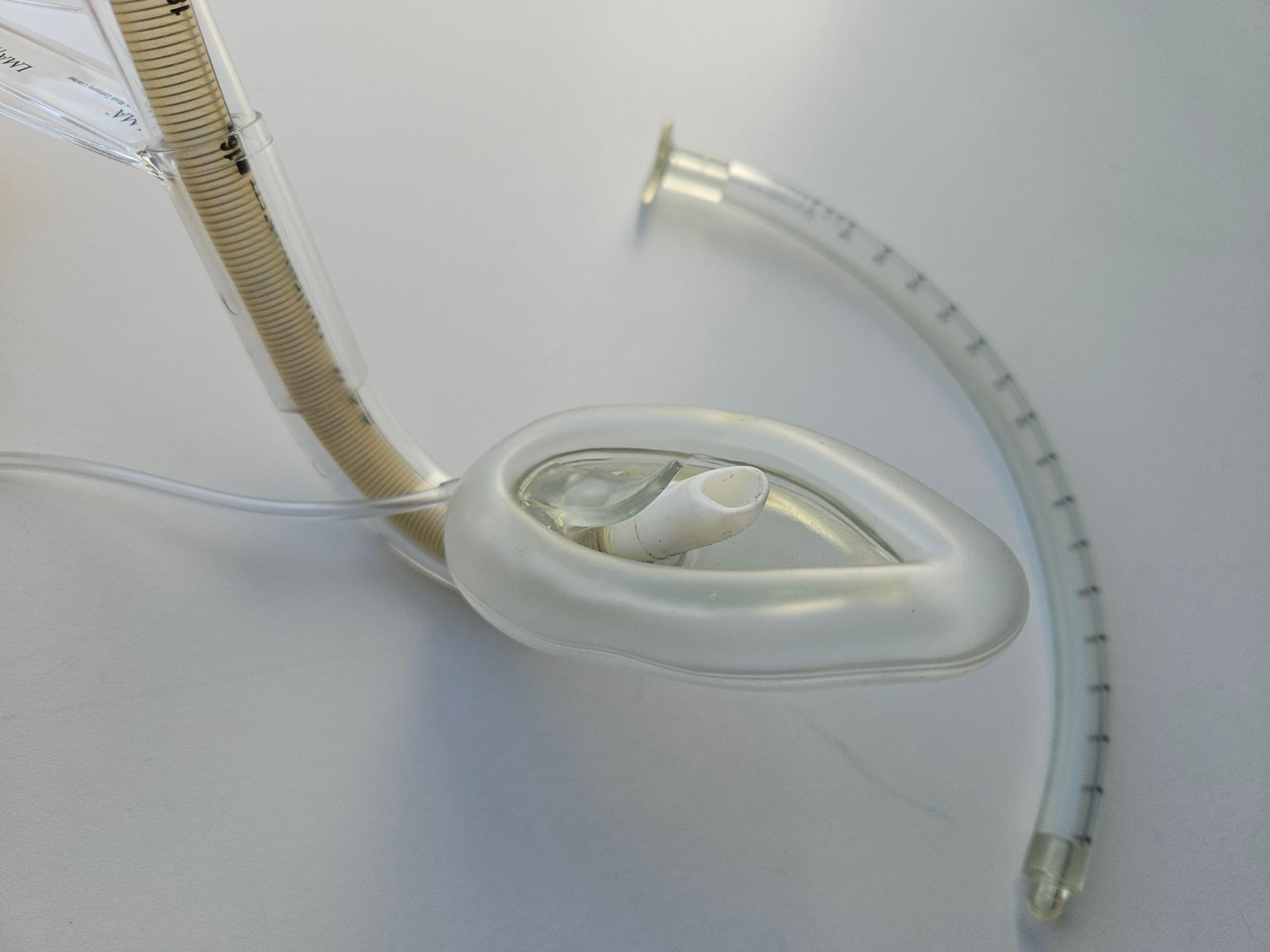
Key Points
- Single use, second generation supraglottic airway device
- Designed to facilitate endotracheal intubation either in known difficult airways, or as a rescue device in an unanticipated difficult intubation
- It has a curved airway tube with a unique rigid handle to facilitate one-handed insertion
- It has a cuff much like other LMAs however it also has an epiglottic elevator bar at the patient end of the airway tube
- It will take an 8mm endotracheal tube, whereas other LMAs will only allows 6.5mm or smaller
It comes as a package with a specific reinforced endotracheal tube and a stabilising rod.
- Once the LMA is inserted and the cuff inflated, the patient can be ventilated with the supraglottic component, or the operator can procede to intubation
- The reinforced endotracheal tube is lubricated and inserted through the iLMA
- The ETT cuff is inflated and ventilation confirmed with capnography
The iLMA can then be removed or left in place
- To remove the iLMA, the connector at the end of the endotracheal tube needs to be removed first
- The iLMA is then removed, leaving the ETT in place
- Insert the stabilising rod into the top of the airway tube, to push the end of the ETT through the airway tube and ensure it stays in place
- Take hold of the ETT once the iLMA is clear of the mouth, reconnect the connector and ventilate normally
Removal of the ILMA, leaving the endotracheal tube in position.
I'd probably avoid this piece of kit.
The Combi Tube

Key Points
- The idea here is that you can plonk it blindly into the patient's mouth and it doesn't particularly matter where the tip ends up
- If the tip is in the trachea, then inflating the distal cuff turns it into an endotracheal tube and you can ventilate the patient conventionally
- If the tip is in the oesophagus then you inflate both cuffs
- The smaller distal cuff occludes the oesophagus, while the larger, proximal cuff occludes the pharynx above the larynx
- Theoretically you can then ventilate the patient through the fenestrations on the side of the tube, using the alternative lumen
- It's critically important that you correctly identify which lumen you're supposed to be ventilating through
It's a horrendous piece of equipment, please don't use it
Laryngoscopes
Laryngoscopes are (mostly*) left-handed intruments used to facilitate visualisation of the vocal cords, usually to then allow the operator to intubate the trachea.
There are three broad categories of laryngoscopes - Direct, indirect and video.
Direct laryngoscopes aim to align the oral and pharyngeal axes, enabling the operator to see the vocal cords in a straight line through the mouth from behind the patient's head.
Indirect laryngoscopes use mirrors or fibreoptics to allow the operator to look around the corner into the pharynx.
Video laryngoscopes are technically a subset of indirect laryngoscopes, and do not necessarily require the oral and pharyngeal axes to align, as the camera is on the blade itself, allowing tube passage in more difficult airways.
*There are blades designed to be used in the right hand, which logically are called 'left handed laryngoscopes'.
Macintosh Blade


Key Points
- The OG (don't say this in the exam)
- Left handed instrument for airway manipulation to facilitate endotracheal intubation under direct vision by aligning the oral and pharyngeal axes
- Curved blade with groove to displace tongue to the left
- Tip is placed in the vallecula, and pressure on the hyoepiglottic ligament lifts the epiglottis away from the laryngeal inlet
- Fibre-optic light source
- Handle contains battery
Disadvantages
- Skilled technique requiring experience to use reliably
- Difficult to teach as only operator can see the glottis
- Doesn't always work
Other variants
- The Polio blade has a 135° angle rather than 90°
- This makes it easier to insert the blade into the mouth when there is anything in the way above the sternum, such as an iron lung, (or large breasts in obstetric patients)
- The stubby handle is a standard right angle but much shorter for the same reason
Miller Blade


Key Points
- Straight blade direct laryngoscope blade
- Long curved tip
- Designed to lift epiglottis directly, rather than via the hyoepiglottic ligament
- Frequently used in paediatric airways because they have a comparatively larger and more floppy epiglottis that doesn't lift as easily by lifting the vallecula
Kids often go bradycardic at intubation because the Miller blade stimulates the underside of the epiglottis, which is innervated by the vagus nerve, rather than the glossopharyngeal nerve, which innervates the vallecula.
McCoy Blade

Key Points
- Direct laryngoscope with curved blade very similar to mac
- Added feature of hinged tip
- Lever mechanism flexes the tip of the blade in order to improve visualisation of the larynx by moving the larynx more anteriorly
- Useful for more difficult intubations (e.g. patients with anterior larynx) – but has largely been made obsolete by videolaryngoscopy
Videolaryngoscope blades

Key Points
- Macintosh and Hyperangulated videolaryngoscope blades
- The Mac blade can be used with the direct or indirect technique, which makes it useful for training, as the trainee can perform direct laryngoscopy and the trainer can watch the screen to assess their technique
- The hyperangulated blade does not require the oral and pharyngeal axes to align and can be very helpful in more difficult airways
- Theoretically there is reduced force required, producing less of a haemodynamic response to laryngoscopy
- The hyperangulated blade usually requires a stylet to angulate the endotracheal tube
Airtraq Optical Laryngoscope

Key Points
- Single use optical indirect laryngoscope
- Offers a magnified angular view of the larynx to facilitate intubation
- It has an optical channel and a guiding channel, into which the ET tube is clipped prior to insertion
- After insertion into the mouth, the operator looks down the guiding channel like a periscope
- The tube is then slid forward through the guiding channel and once intubation has occured, it can be clicked sideways out of the channel to allow the scope to be removed from the mouth
- There are now videolaryngoscope versions available
Endotracheal tubes
The 'definitive' airway, these devices isolate the trachea from the oesophagus and pharynx, to protect it from aspiration and facilitate ventilation.
Features generally common to all tubes
- Standard 15mm connection
- Radio-opaque line along tube allows localisation under xray
- Cuff to generate a seal within the trachea, both to protect against aspiration and to allow positive pressure ventilation with pressures up to 30 cmH2O
- The distal end features a left-facing bevel designed to improve visualisation of the cords during intubation (as the tube is inserted from the right side of the mouth)
- Most tubes have a Murphy eye, which is a second hole on the side of the tube near the distal end, which reduces the liklihood of the tube getting blocked, and by virtue of the fact that it is situated on the right side of the tube, if the patient's right upper lobe happens to originate from the trachea slightly proximal to the right main bronchus (see aberrant right upper lobe), then it at least has a chance at ventilating that too
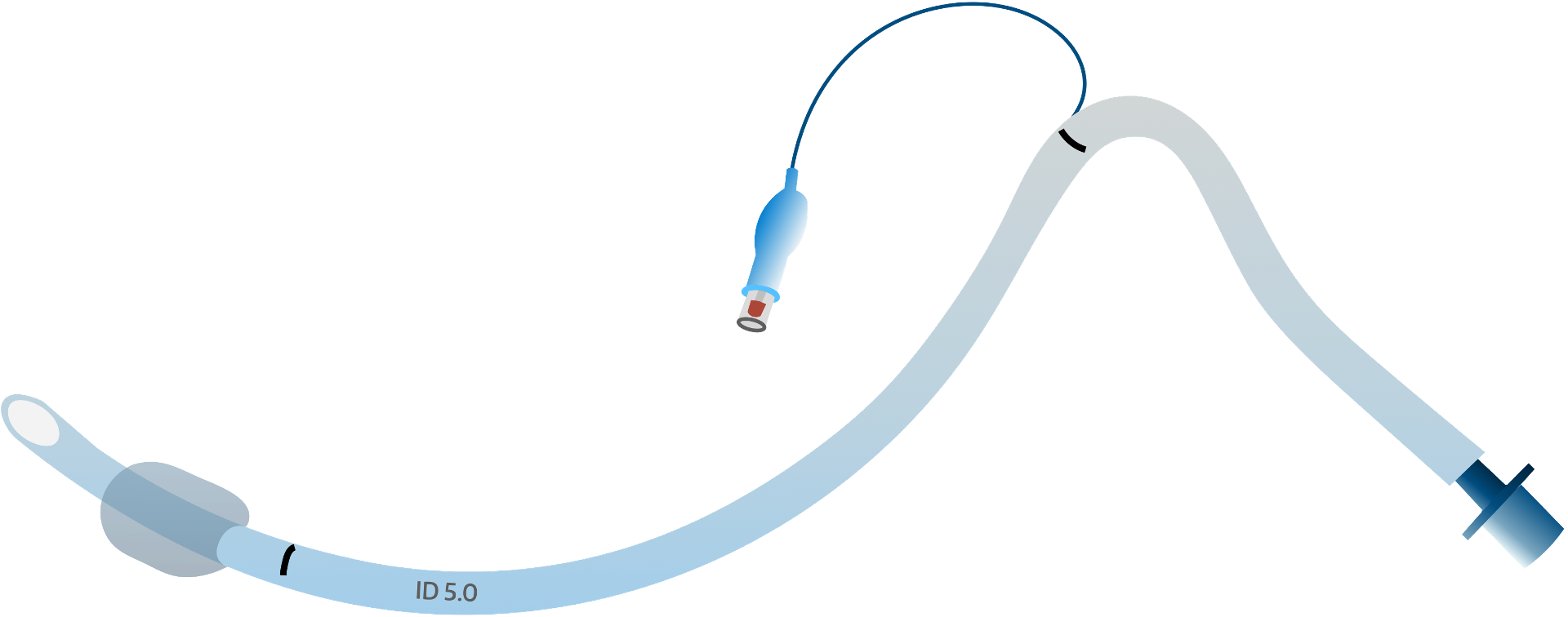
Standard Endotracheal Tube


Key Points
- Standard 15mm universal connector for breathing circuit
- Transparent PVC Tubing
- Pilot Balloon with spring-loaded one-way valve
- High volume low pressure cuff is less damaging to the trachea
- Low volume high pressure cuff provides better protection against aspiration
- Glottis Line
- Murphy Eye
- Bevelled tip
Uncuffed tubes are frequently used in paediatrics as the narrowest point of the airway is the cricoid cartilage rather than the glottis, and there is increased risk of pressure necrosis from a cuff (lower risk with newer, lower pressure cuffs).
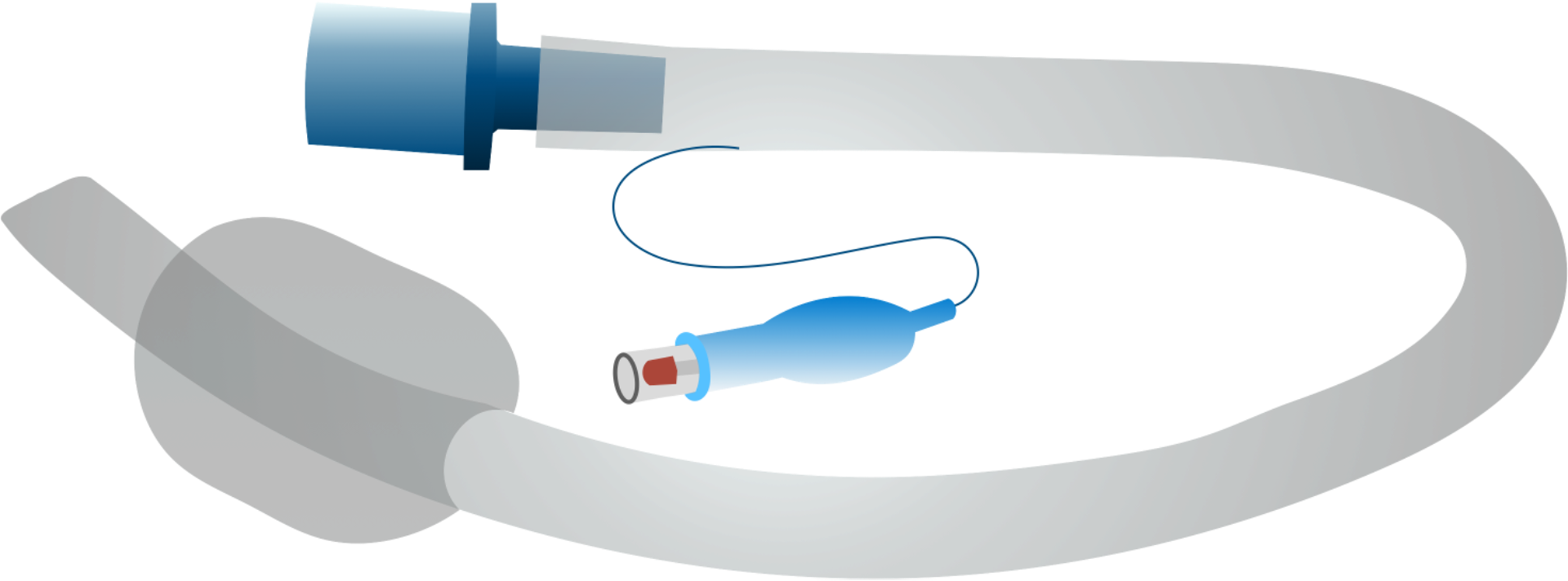
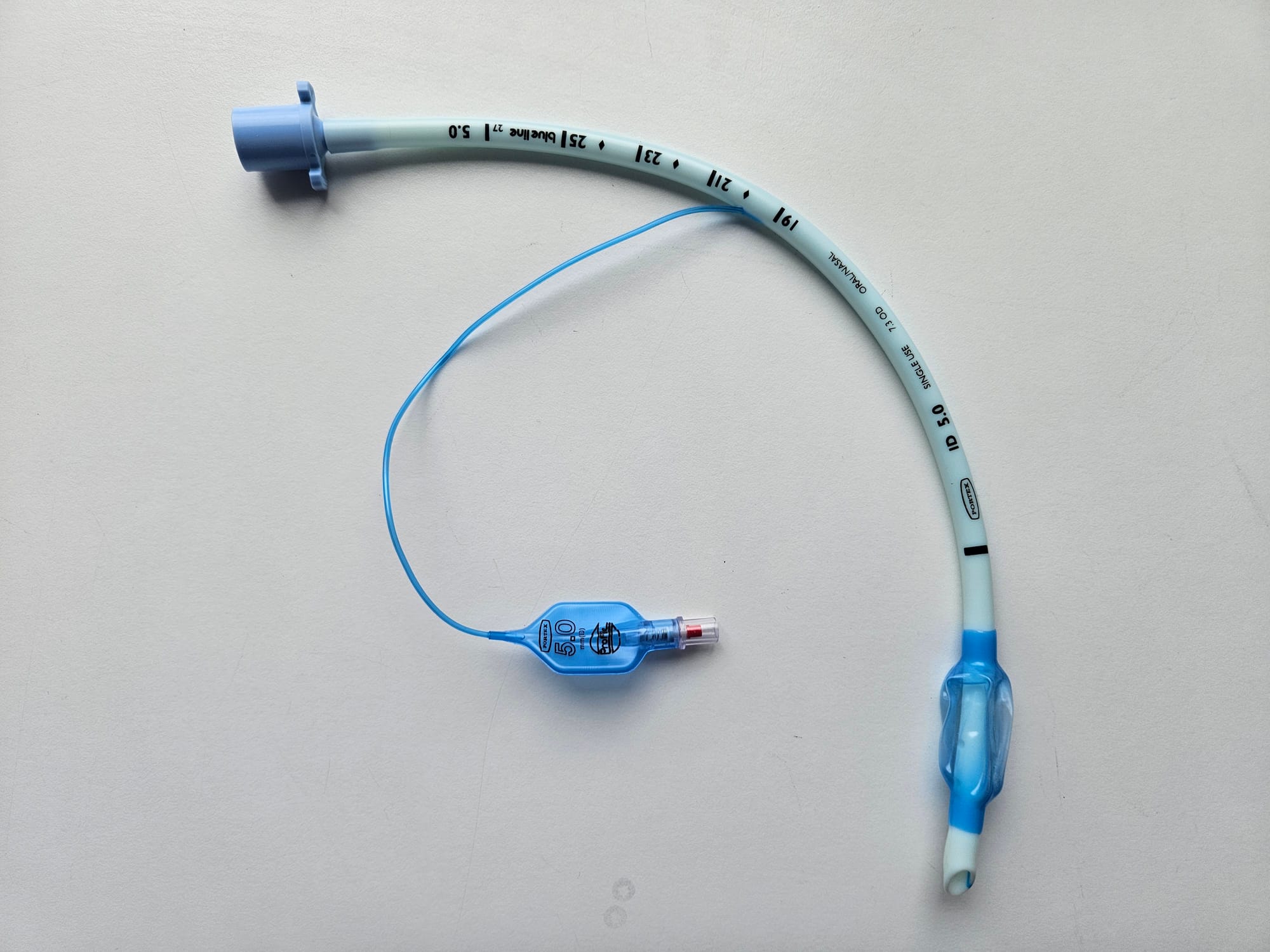
Reinforced Endotracheal tube

Key Points
- Single use endotracheal tube
- Left-facing bevel tip
- Murphy eye
- Reinforcing metal spiral prevents kinking of the tube when bending
- Useful for cases involving extreme positioning such as prone surgery
- Not good if a patient bites it, as it can deform and remain deformed, causing airway obstruction
North-Facing Nasal RAE Tube

Key Points
- Nasal tubes also facilitate oral and facial surgery by bypassing the oral cavity to maximise surgical access
- Patient cannot bite tube, and tube is more stable as held in place by nasopharyngeal anatomy
- The smaller diameter of the tube (to facilitate passing through a nostril) can lead to high peak airway pressures and produce an obstructed ventilatory pattern
- Special care should also be taken to protect the nostril from pressure sores (and subsequent necrosis) from the tube
South-facing RAE Tube

Key Points
- ‘Ring, Adair & Elwyn’ Tube facilitates oral/facial surgery with a south-facing bend in the tube to facilitate surgical access
- Depth of tube insertion is largely determined by the pre-formed bend in the tube, so it can end up sitting too deep or too short if not sized correctly
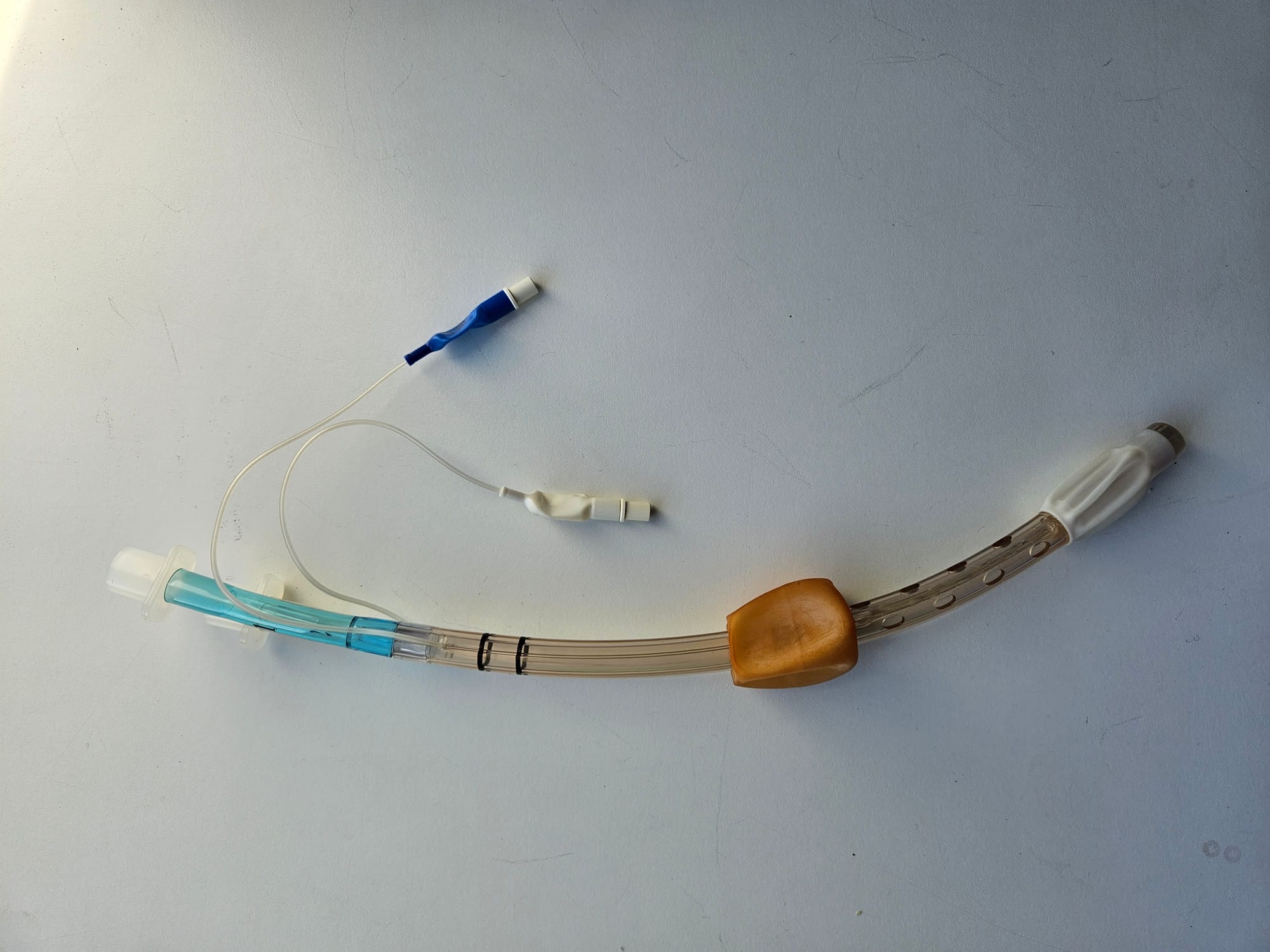
Neural Integrity Monitor (NIM) Electromyogram Tube
Key Points
- Used for Head & Neck procedures where the recurrent laryngeal nerve is at risk of injury
- Colour-coded contact band must be positioned between the vocal cords – these detect vocal cord movement if recurrent laryngeal nerve is stimulated
- Surgeons use a sterile contact probe (passing 0.5-2.0 mA current) to test anatomical sites in question
- Return electrodes are placed over the patient's sternum
- If the surgeon stimulates a nerve, the motion of the vocal cords is detected by the contact band on the ETT and the electrical signal is detected ad displaced on the monitor (with an audible ‘click’)
- Clearly you don't want the patient to have neuromuscular blockade on board during the procedure
Microlaryngoscopy Tube (MLT)
Key Points
- Essentially just a smaller diameter standard tube, but longer as designed for use in adults that would usually take a larger diameter tube
- Size 4-6 mm
- High volume cuff to compensate for reduced tube diameter
- Used in airway surgery, particularly vocal cord surgery, to facilitate easier surgical access to the larynx
- Also used for patients with very narrow larynx
- Generally work very well but can require higher ventilatory pressures and become blocked more easily
Laser safe tube

Key Points
- Used for airway laser surgery as increased risk of airway fire and burns to tissue and equipment
- Matt metal coil deflects laser light and protects tube and pharyngeal tissues from damage
- Cuff filled with saline or dye to allow early identification of cuff damage
- Some tubes have a double cuff for extra protection
Double Lumen Tubes
Here's a classic Final FRCA CRQ Question:
What are the absolute and relative indications for using a double lumen tube?
Absolute
- Unilateral lung abscess or empyema
- Massive pulmonary haemorrhage
- Bronchopleural fistula
- Tracheobronchial trauma
- Pulmonary toilet/lavage
- Bronchial sleeve resection
Relative
- VATS
- Pneumonectomy
- Lobectomy
- Oesophagectomy
- Thoracic aortic aneurysm repair
- Split lung ventilation on ITU
The two names you need to know for the exam are Carlens and Robertshaw.
The Carlens tube has a carinal hook, which theoretically makes it easier to sit the bronchial lumen in the right place, however most modern tubes are now based on the Robertshaw design.
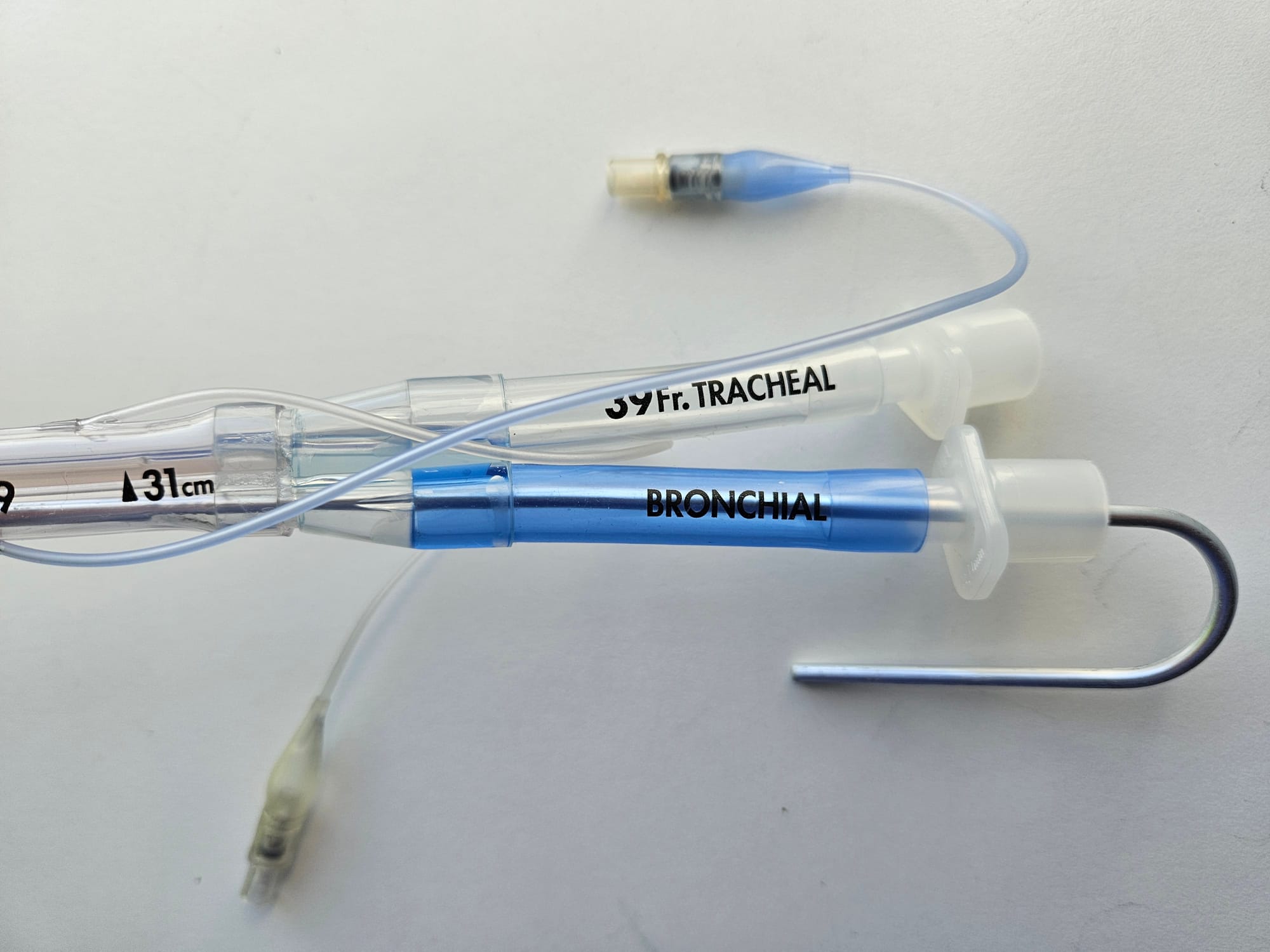
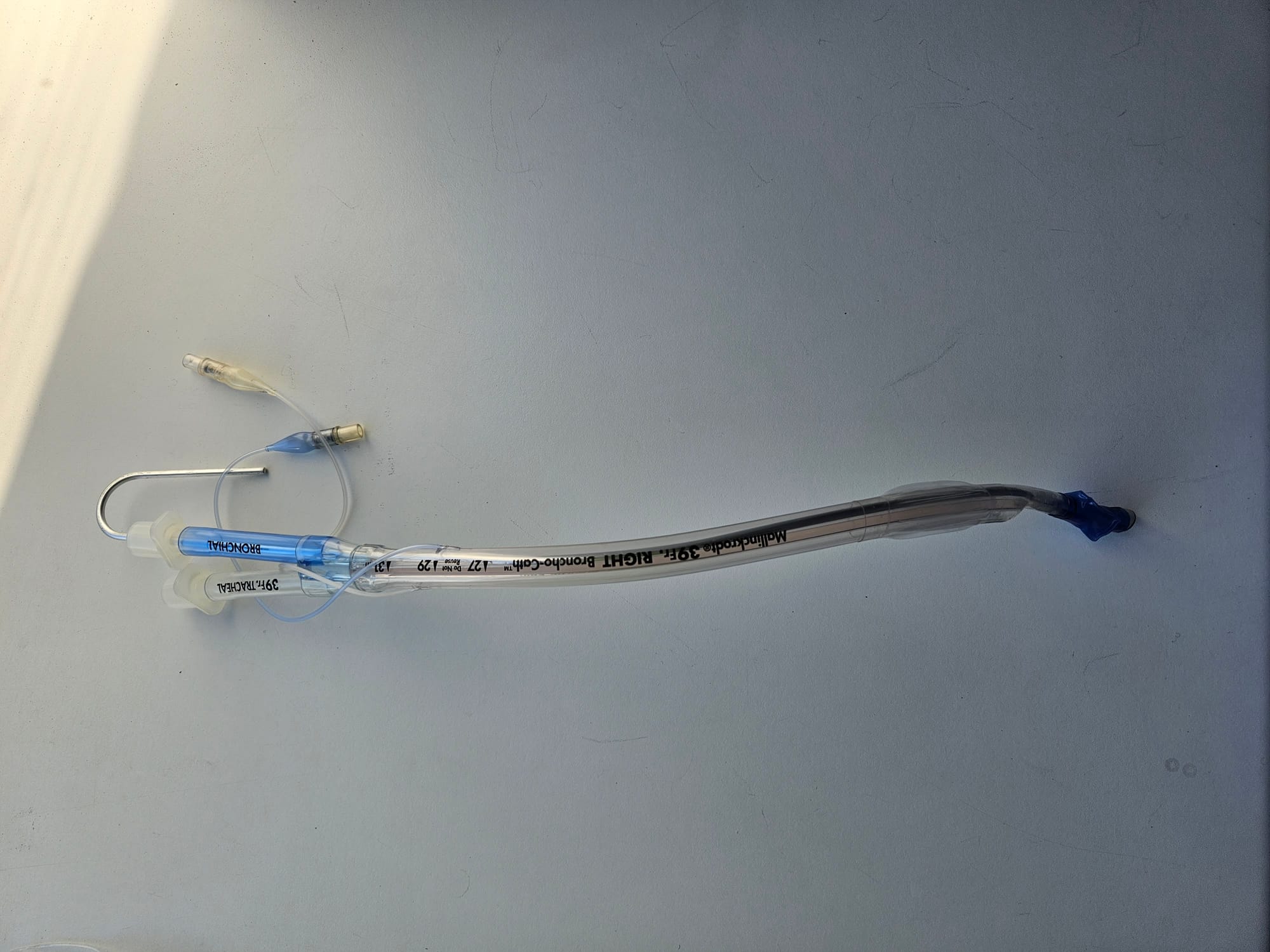

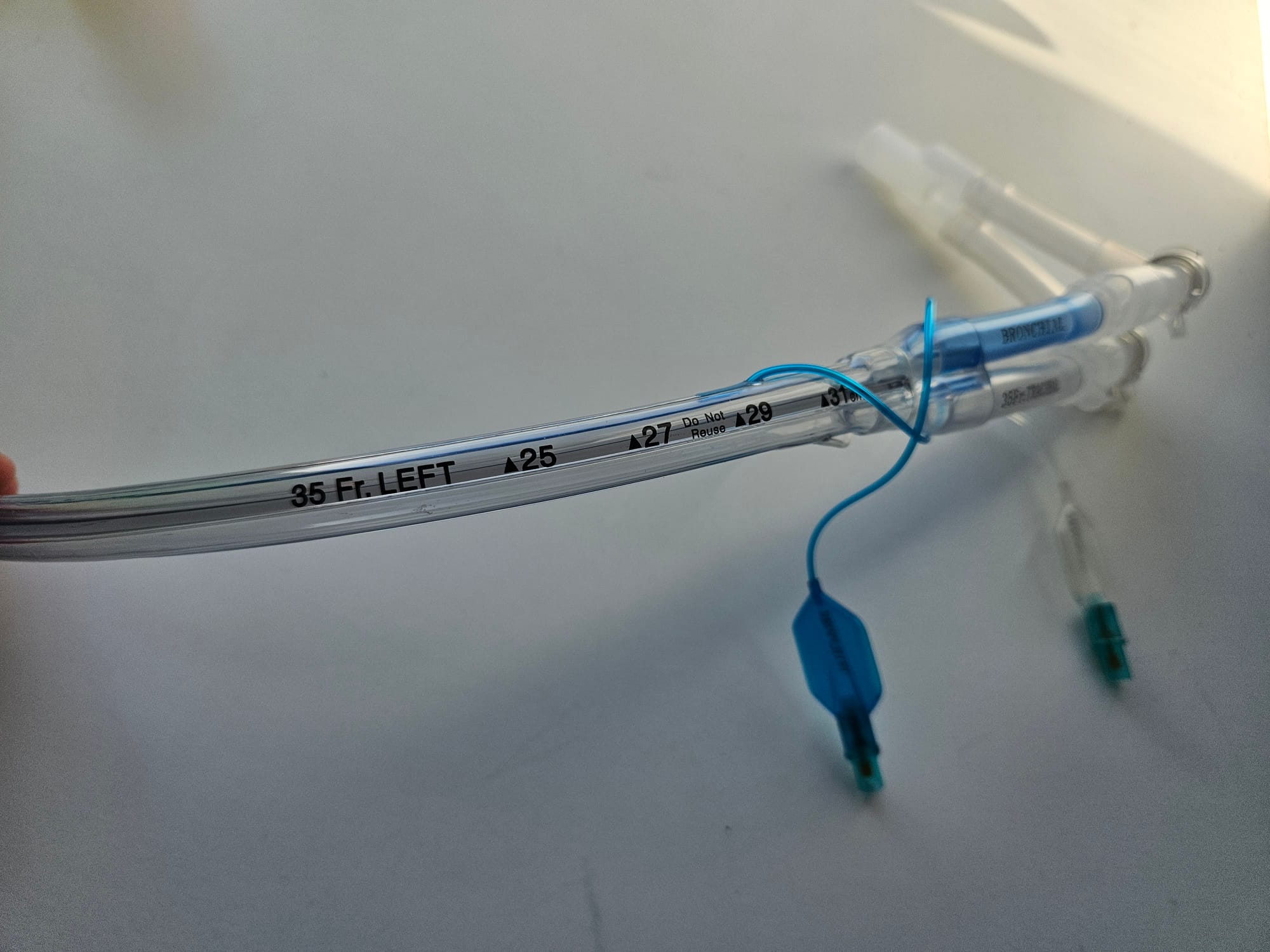
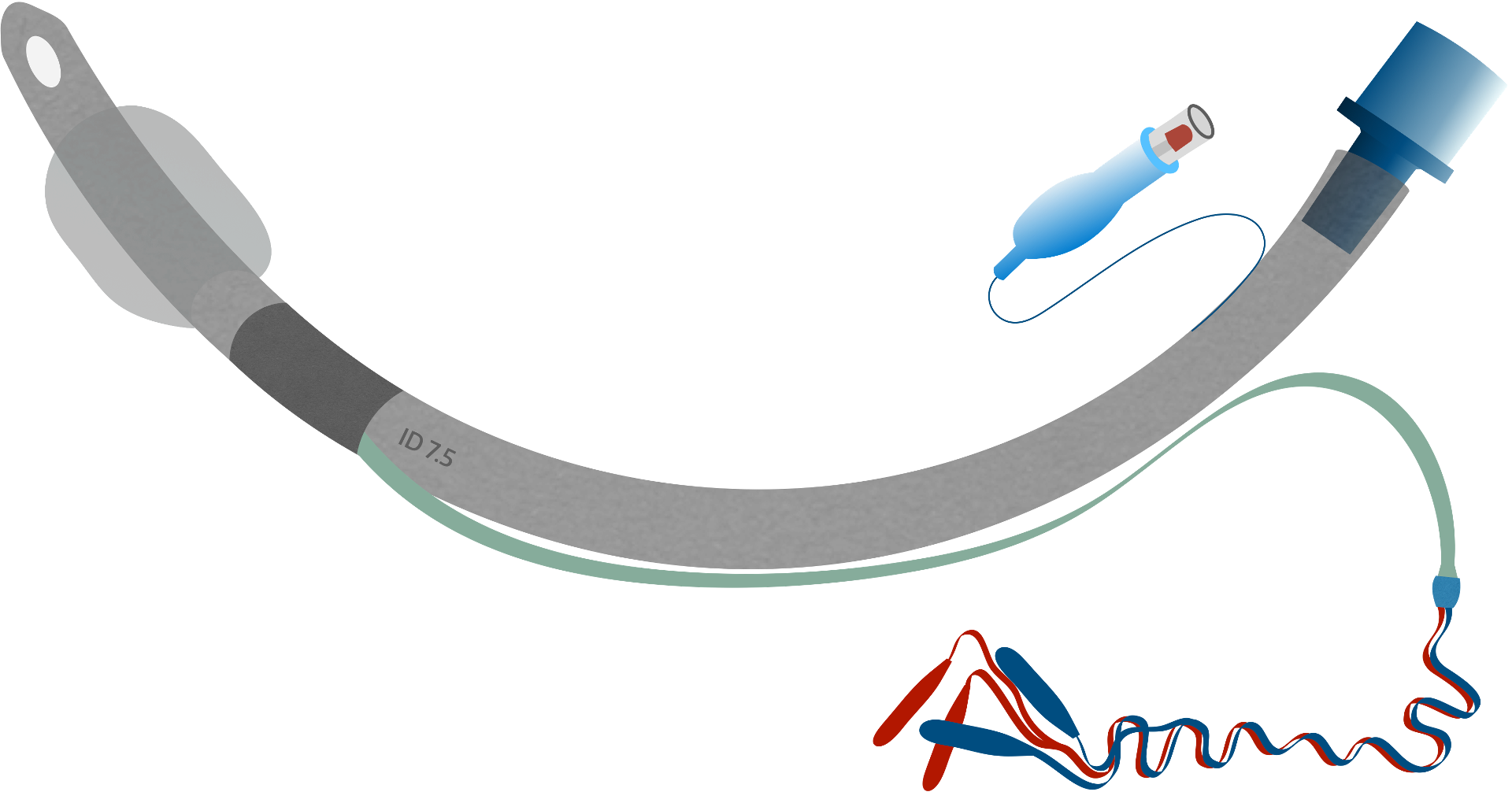
Key Points
- Tracheal and bronchial lumens
- Left and Right sided versions available
- The cuffed end is inserted into once of the main bronchi and the cuff inflated
- One lumen ventilates the isolated lung, and the other lumen ventilates the trachea and therefore the other lung
- The tubes have a combined connection at the top to facilitate bilateral ventilation
- The tubing can be clamped proximal (machine side) to the right angled catheter mount, and the catheter mount can then be opened to allow the air to drain out of the isolated lung and the lung to collapse to facilitate surgical access

Key Points
- The cuffs are different on right and left double lumen tubes
- The cuff on the right sided double lumen tube has an obliquely angled cuff, and an eyelet to optimise ventilation of the right upper lobe, which can branch off from the right main bronchus very proximally
- The left sided tube does not have an eyelet and has a smaller, more spherical cuff
Bendy sticks
Bougie
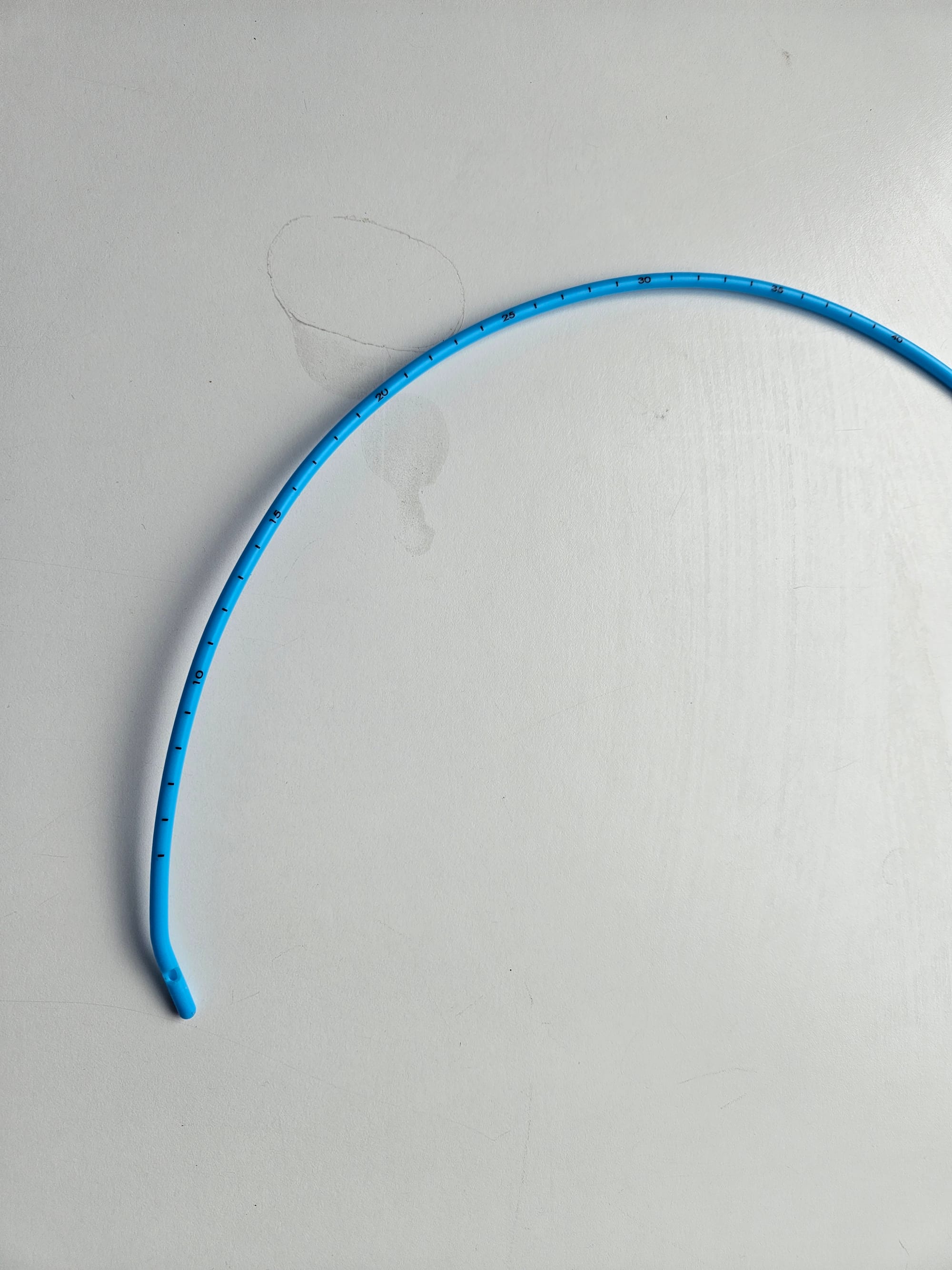
Key Points
- Semi-rigid 15 Fr rod, usually 60cm in length
- Used as a guidewire over which to railroad endotracheal tubes
- Its stiff, narrow profile makes it easier to pass into the trachea, and the tracheal rings can be felt as the bougie advances, serving as further reassurance of correct placement
- Can also be used to facilitate safer tube exchange, and for emergency front of neck access
- Paediatric bougies (10 Fr) are also available
Alternative versions

Key Points
- All the benefits of a standard bougie, with the added fun of a flexible wiggly tip that can be controlled with the operatiors thumb half way along the bougie
We highly doubt this will be examined, however please do let us know if it is...
Stylet

Key Points
- It's a bendy metal stick, there's not much else to it really
- Used to provide angulation to endotracheal tube to facilitate intubation with hyperangulated laryngoscope blade
- Curved top prevents it disappearing down the airway
- Risk of airway trauma, thanks to its being a bendy metal stick and all that
Airway Exchange Catheter
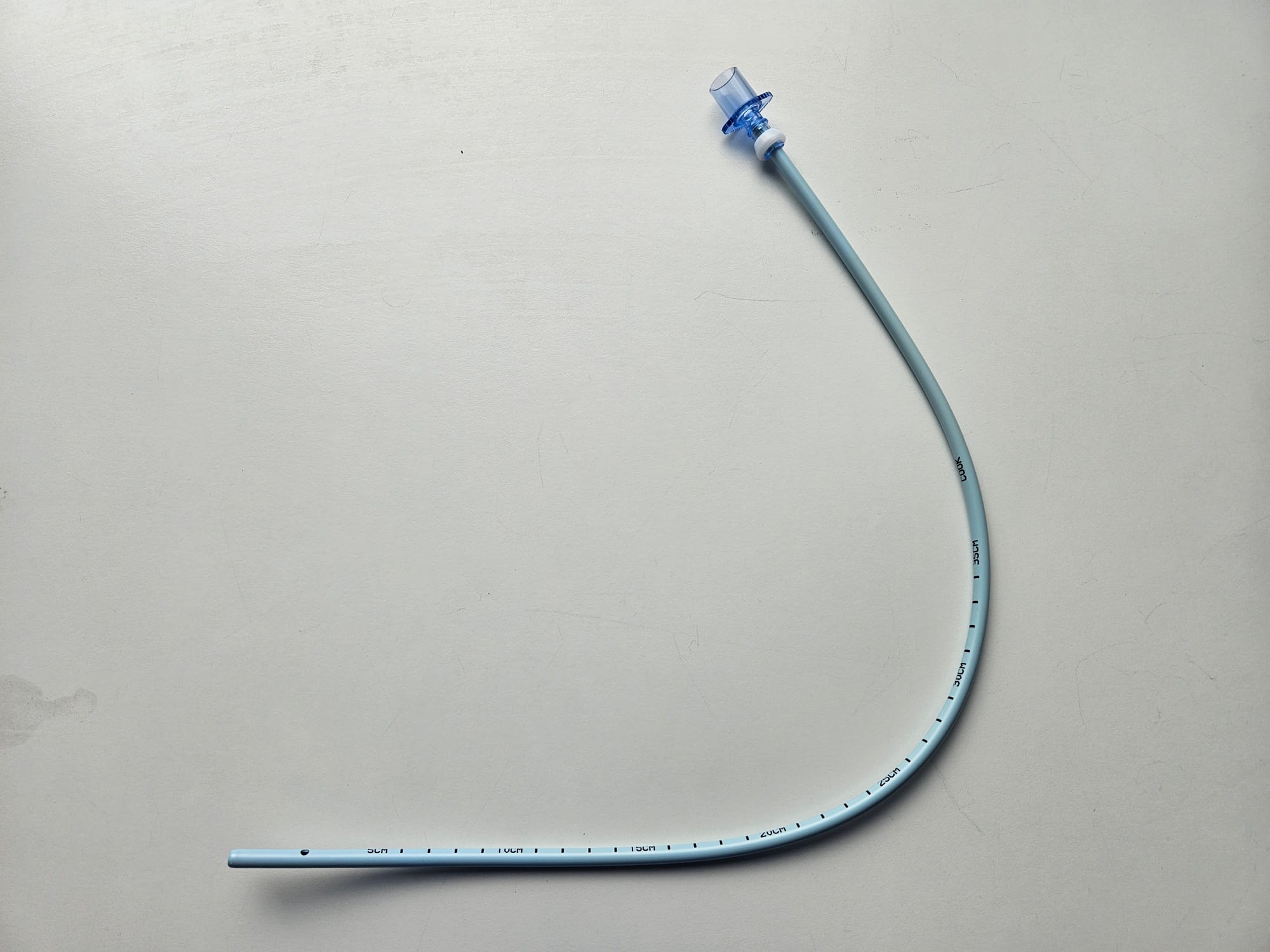
Key Points
- Larger diameter catheter with adaptor to allow connection to 15 mm connector
- This allows jet ventilation or oxygenation down the catheter during airway exchange
- The hole on the side at the distal end reduces chances of catheter becoming blocked
- Doesn't retain its shape like a bougie, so needs an airway in place first
The classic use for this piece of kit is either a tube change or switching from a supraglottic airway device to an endotracheal tube. The catheter is inserted into the SGA, either blindly or loaded onto a bronchoscope.
Once the catheter is in the trachea, the SGA is removed and the ETT railroaded over the catheter like a bougie.
Jet ventilation catheter
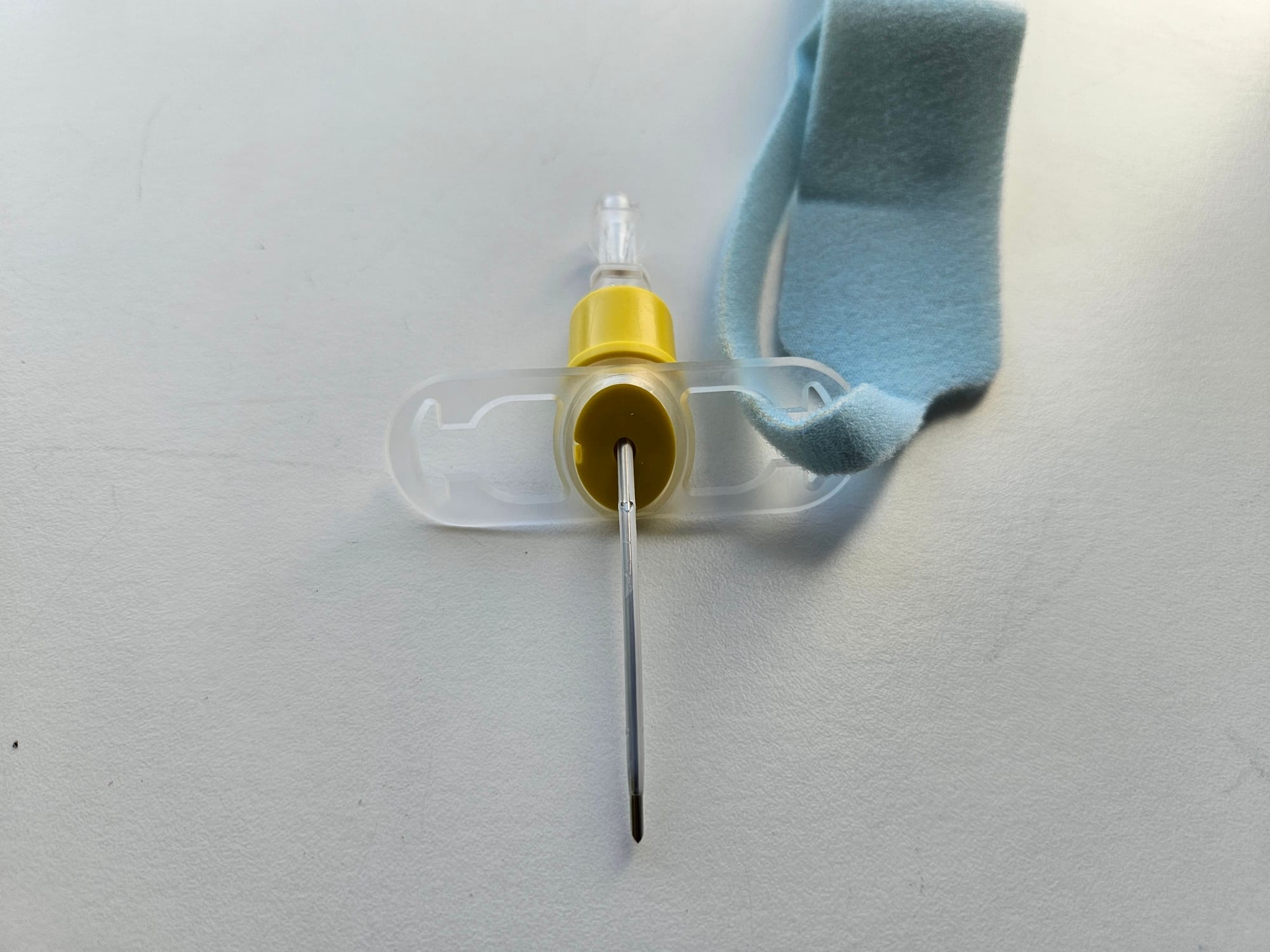
Key Points
- Inserted into the trachea through the cricothyroid membrane to facilitate jet ventilation
- Can be used electively or as a rescue technique
- Risk of false passage and airway trauma as sharp needle and blind technique
Clamps and grabbers
Magill Forceps
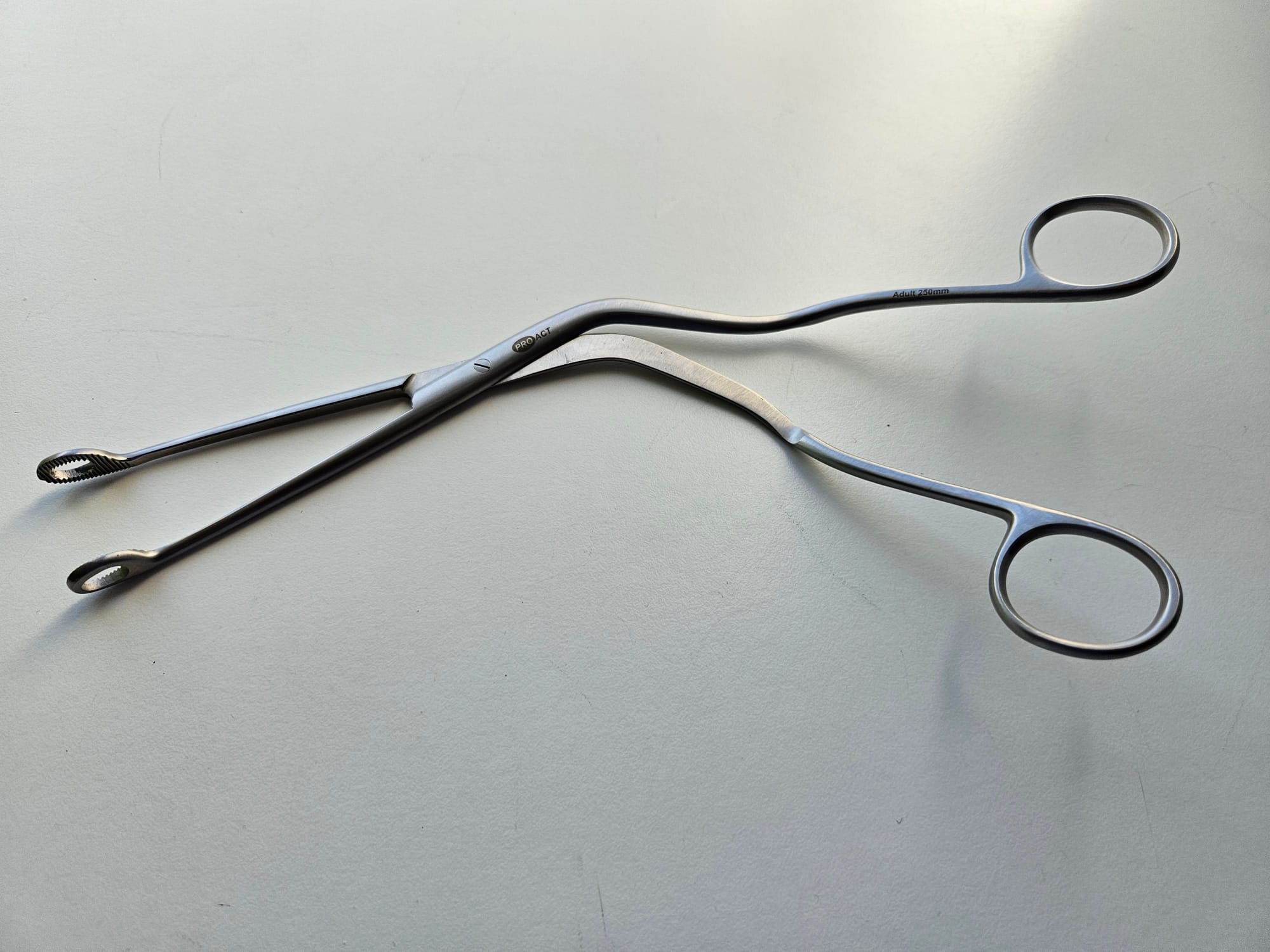
Key Points
- Twin bladed forceps with round grasping ends
- Oblique angle of handles to allow direct visualisation of airway during use
- Can be single use or reusable
- Used to insert nasogastric and endotracheal tubes, pharyngeal packs, or to retrieve foreign objects from the airway
- Risk of airway trauma and bleeding
Tube Clamp

Key Points
- Endotracheal tube clamp
- Used to maintain PEEP when disconnecting breathing circuit
- Also used to reduce aerosol generation in viral respiratory infections
- Flat blades to reduce trauma to endotracheal tube
- Right angled limbs facilitate clamping from in front or behind the patient
Never clamp a reinforced tube, as it will deform the metal spring and the tube will remain pinched after removing the clamp.
Tracheal dilator

Key Points
- The reverse mechanism to a clamp - squeezing the handles opens the limbs
- Allows the user to dilate small tracheal holes to facilitate front of neck access
Tracheal Hook

Key Points
- Used to hold onto trachea during front of neck access
You don't really need to know any more than that.
Humphrey ADE breathing system
This is the only breathing system we're going to mention here. We've done a post here on all the other breathing systems you need to know about.
We're mentioning it here because this is the sort of kit they like to whip out in the exam to see if you've been doing your reading, even though you've literally never used it.


Key Points
- A mechanical valve system that allows the operator to convert the breathing system between a Mapleson A, D or E just by moving a lever
- Mapleson A is most efficient for spontaneous breathing
- Mapleson D is most efficient for IPPV
- Mapleson E facilitates low-pressure ventilation of the spontaneously breathing patient
- The circuit consists of a metal block with a fresh gas inlet, two reservoir bag connectors, an APL valve, tubing connectors and rotary valves connected to the selector lever
- The selector lever moves the rotary valves which in turn alter the dynamics of the circuit to be either a Mapleson A, D or E system
- It is either a semi-open or a semi-closed system, depending on whether it is set up as a circle system with soda lime
Tracheostomy tubes
What are the indications for a tracheostomy?
Airway protection
- Particularly when the upper airway is obstructed
- As a rescue in difficult airway
Respiratory weaning on ITU
- Well tolerated by awake patients, allowing respiratory support to continue in an awake patient who can start mobilising and communicating
- Allows for airway suctioning
Sleep apnoea
- In severe cases where CPAP doesn't work
Swedish Nose

Key Points
- Essentially a posh wet sponge to humidify and warm the inspired air
- Used to facilitate tracheostomy weaning as last step before decannulation
- Supplemental oxygen can be given through standard facemask tubing
- Frequently clogs with secretions and needs changing
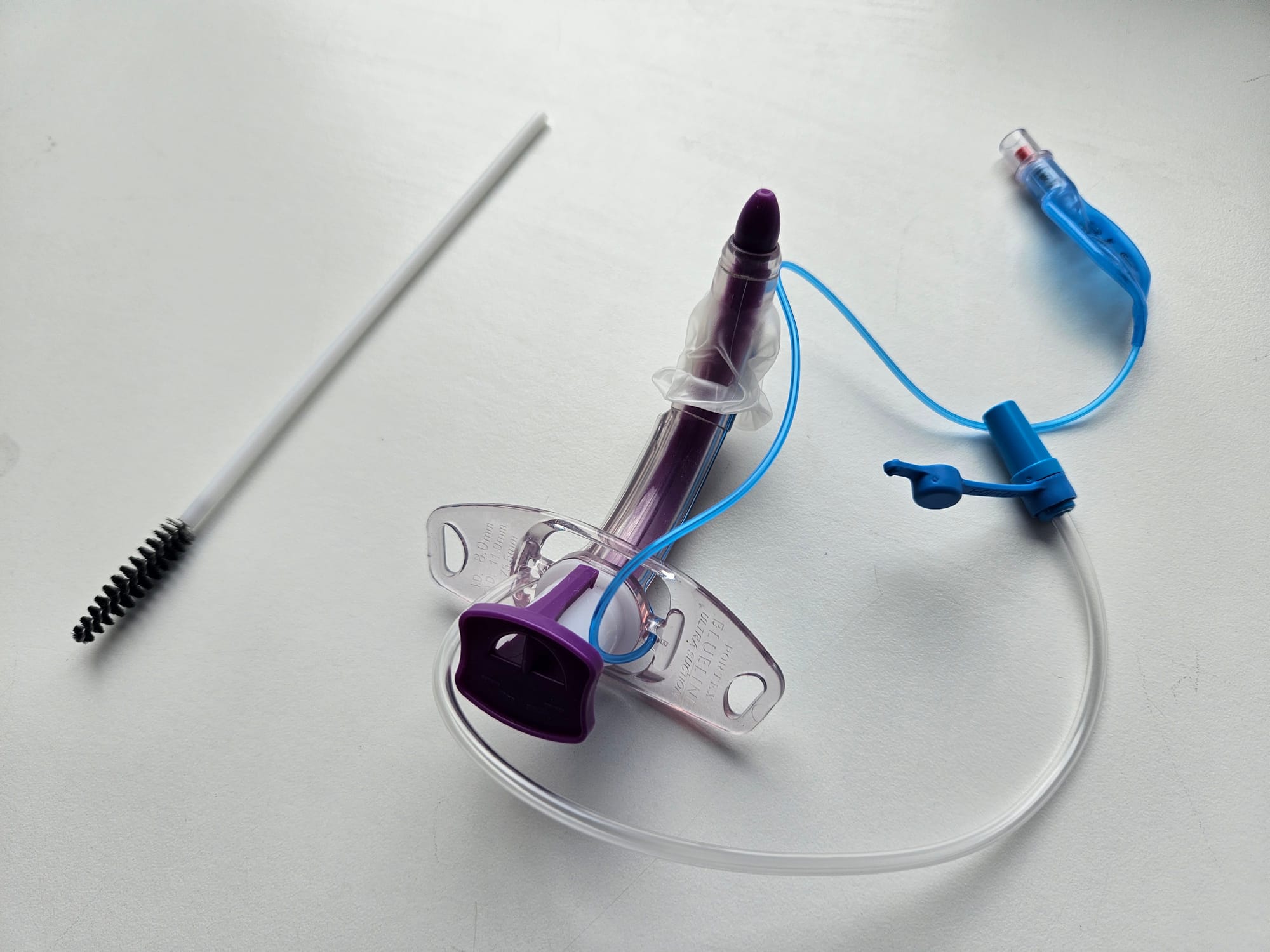
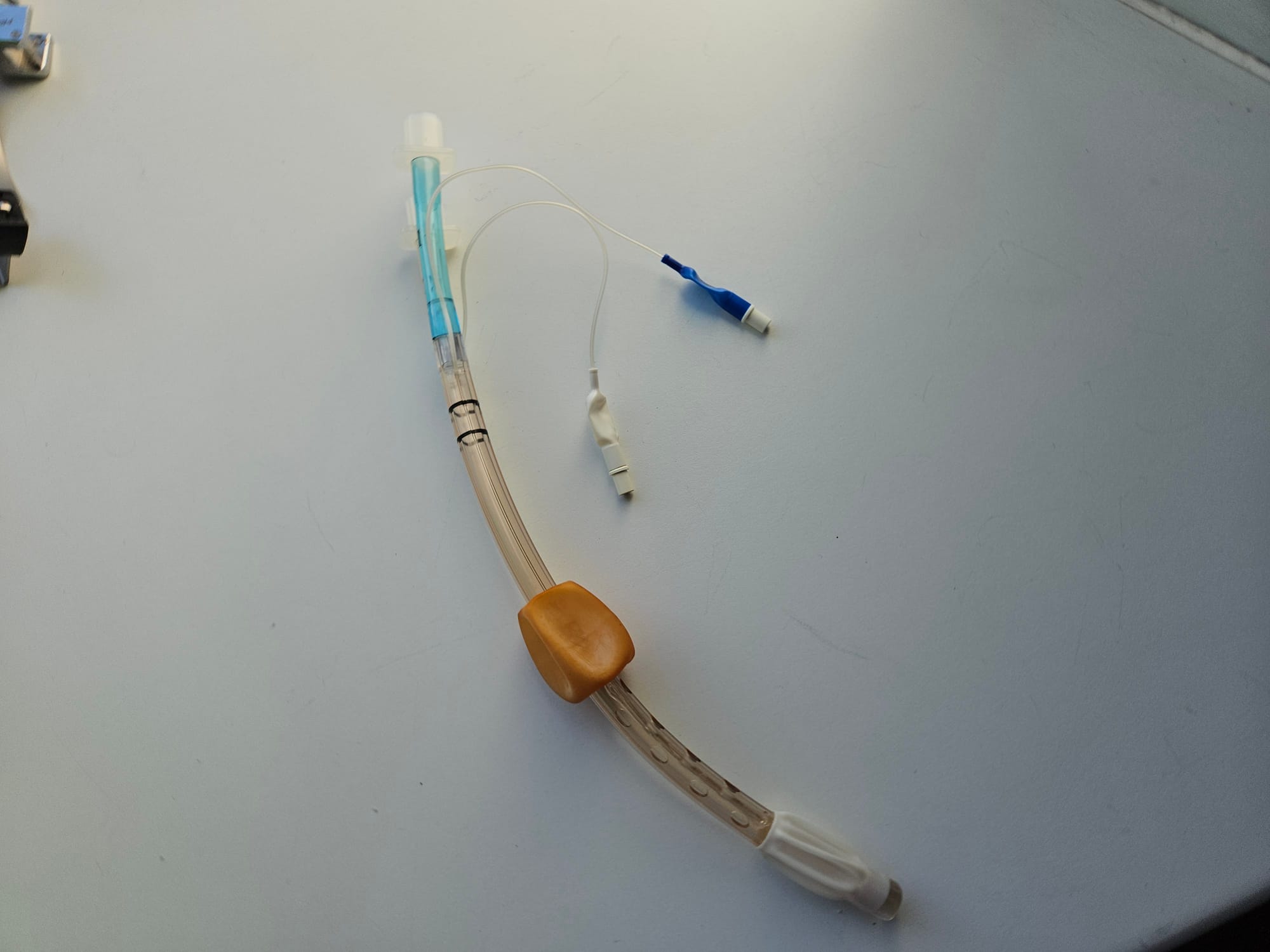
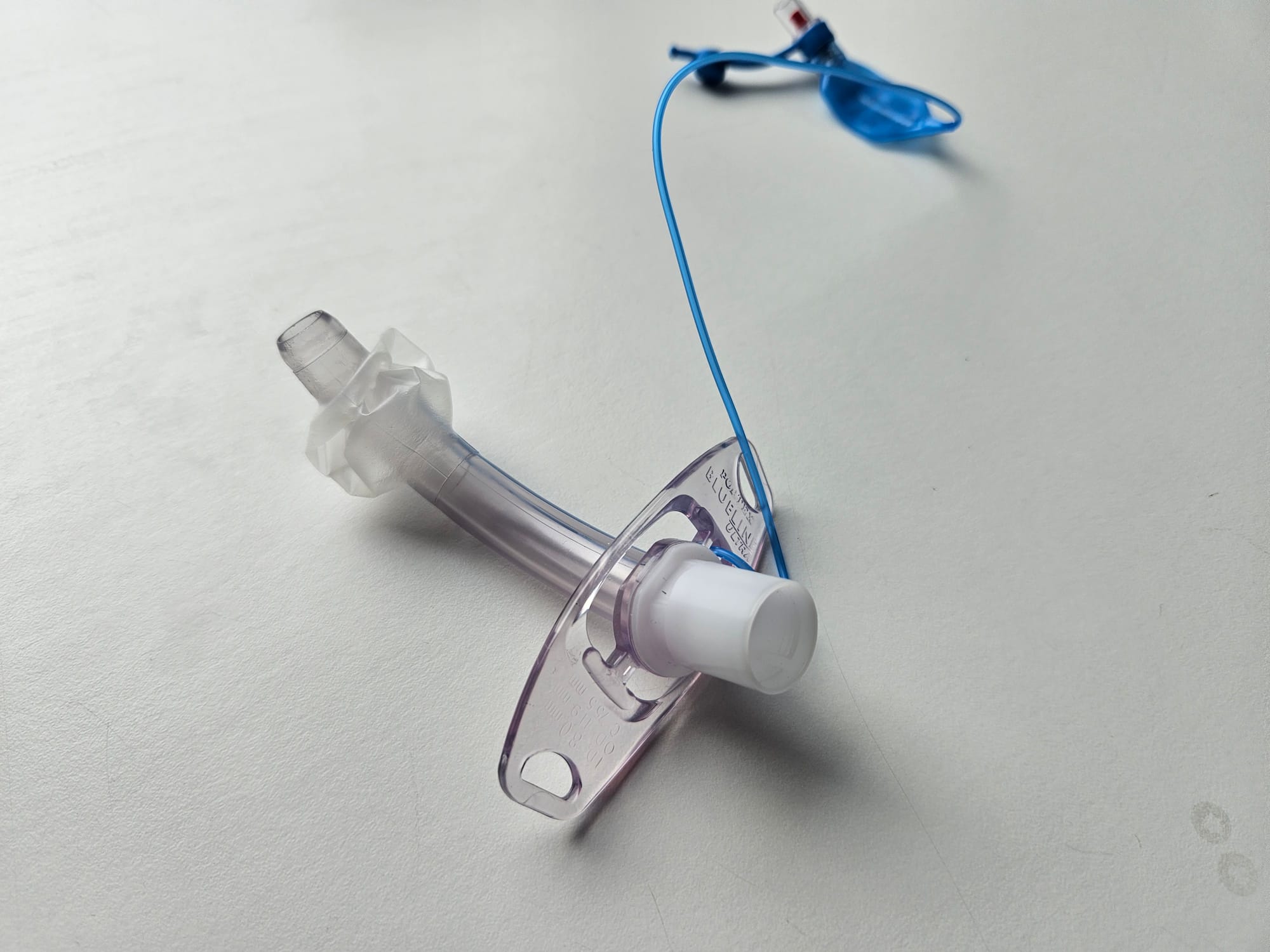
Key Points
- Tracheostomy tube loaded onto introducer
- Pilot baloon (blue) for cuff inflation
- Supraglottic suction port
- Separate inner tube cleaner
Inner tube

Key Points
- Designed to be easily removed and cleaned or replaced if blocked
- Looks similar to nasopharyngeal airway, so don't get confused - note the square end here whereas a NPA has a bevel
Our quick recap video
Our Laryngoscope TikTok video
@anaestheasier What is a Laryngoscope?
♬ Breathe - Mackenzie Ziegler
Non rebreathe facemask
Useful Tweets and Accounts
These are two of the most useful Twitter accounts to follow for anaesthetics - we'd highly recommend them!
Happy New Year Everyone! Welcome to #JanuAIRWAY best bites 2023. Starting with oxygenation. The meaningful delivery of oxygen is the fundamental aim of all airway management. Think ABO – Always, Be, Oxygenating. Here’s some #OnePagers covering the basics of oxygen physiology. 1/2 pic.twitter.com/GFUqJnE1bz
— Difficult Airway Society (DAS) Trainees (@dastrainees) January 1, 2023
In honor of #JanuAIRWAY - here are a 2 #ICUOnePagers relevant to safely monitoring patients during airway management: #Capnography & #PulseOximetry.
— Nick Mark MD (@nickmmark) January 9, 2022
Learn the physiology & how these devices work, what clues are hidden in the waveforms, & what can make them less accurate #FOAMed pic.twitter.com/Mo1yXtoYoS
A useful subreddit

