Adrenal cortex disease in anaesthesia

Take home messages
- Adrenal disease produces disturbances in electrolytes and water distribution, which need correcting and monitoring perioperatively
- The main knock-on effect from this is cardiovascular instability
- Patients may require steroid replacement
- The Association of Anaesthetists' guidance on steroid replacement is found here
- If in doubt - give some glucocorticoids
- Don't forget to monitor blood sugar!
In terms of 'importance per gram of organ' the adrenals are way up there with the parathyroids.
They can mess up an anaesthetic very quickly indeed unless you pay attention.
Rapid Review of anatomy
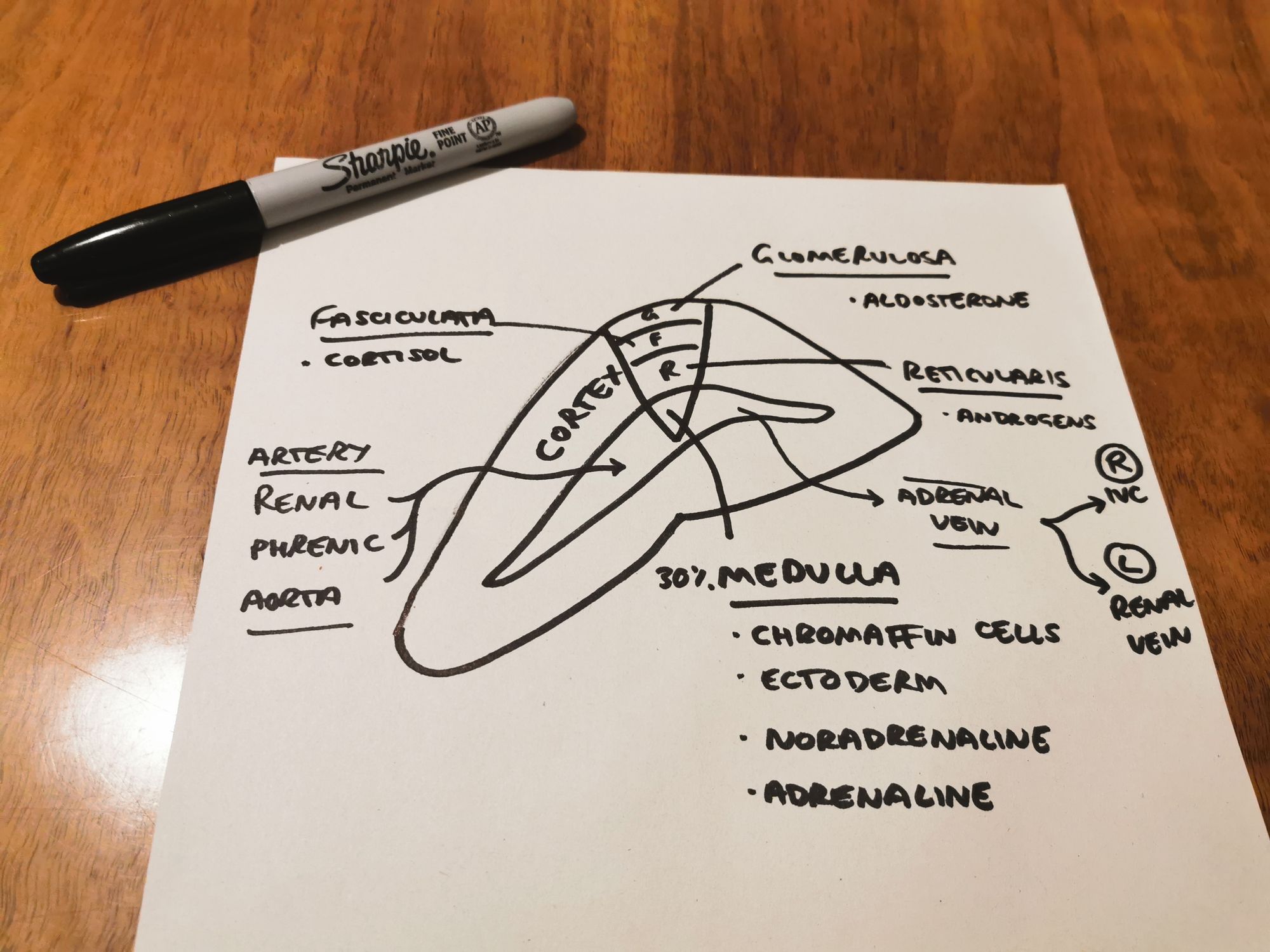
For the purposes of this article, we'll focus on the cortex. Phaeochromocytoma deserves it's own post, which will follow in due course.
If you can't wait, read this
What do glucocorticoids do?
- Metabolism of carbohydrates, proteins and fats
- Stress response - important for cardiovascular stress response!
- Fasting response
What do mineralocorticoids do?
- Fluid and electrolyte balance
- Note cortisol has mineralocorticoid activity, especially if it is produced in excess, which is why Cushing's and Conn's syndrome both have hypernatraemia, hypokalaemia and metabolic alkalosis
We made a 30 second TikTok explanation of the electrolyte abnormalities seen in Conn's syndrome
View in browser to watch the video
@anaestheasier Conn's syndrome is a condition characterised by excess aldosterone. This causes a hypernatraemic, hypokalaemic, metabolic alkalosis #FRCA #novice #odp ♬ original sound - Anaestheasier
Who's driving this thing?
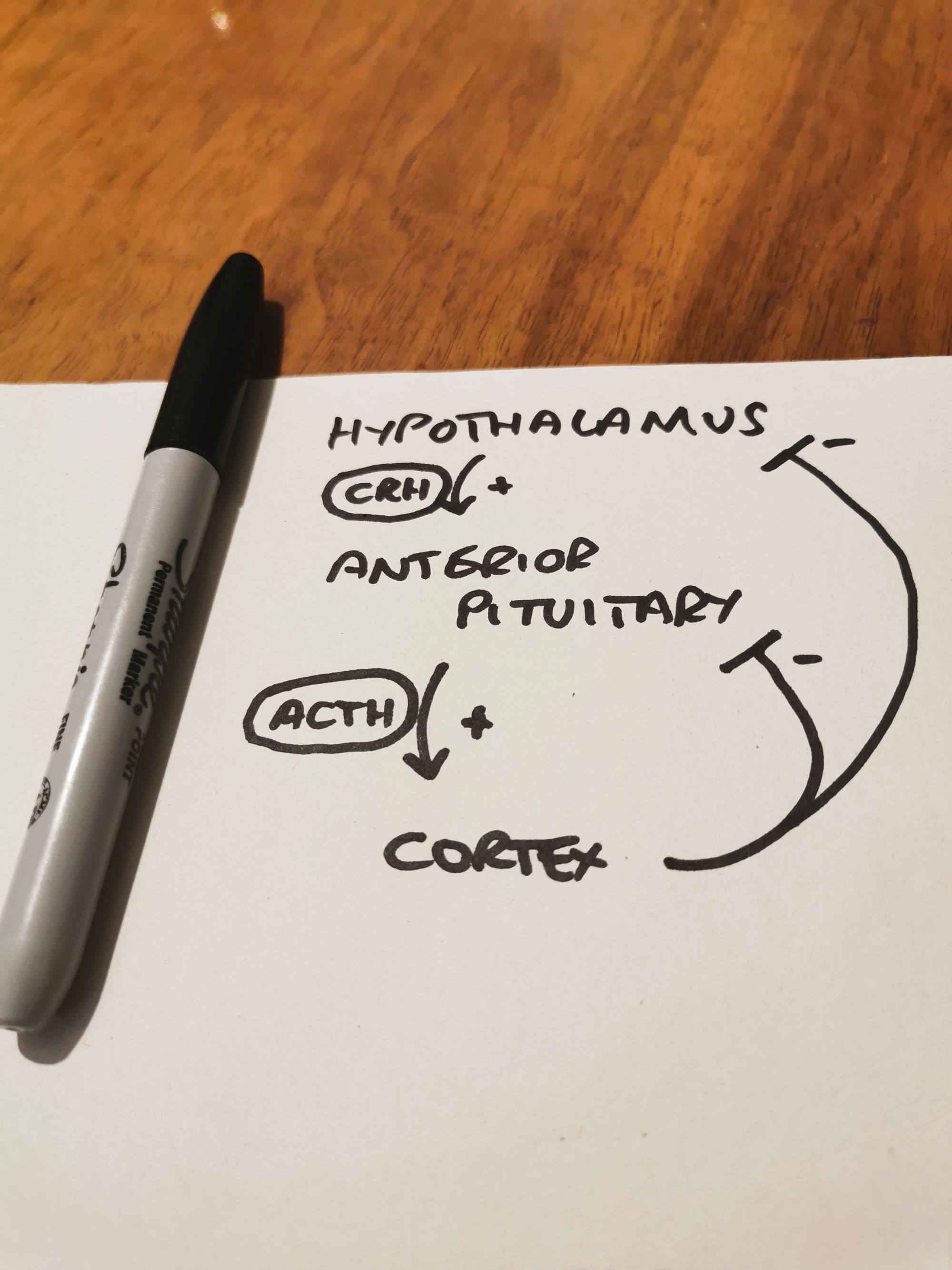
- The HPA axis runs on diurnal rhythms and negative feedback
- Cortisol is highest around 8am
The Renin-Angiotensin-Aldosterone System
This system mainly helps the body retain blood volume
- It does this by retaining salt, and dragging water with it via osmosis
- Low blood pressure to the kidney and sympathetic stimulation trigger renin release from the epithelioid juxtaglomerular cells
- Renin cleaves angiotensinogen to produce angiotensin 1 (AT-1)
- This travels to the lungs, and is converted to AT-2
- AT-2 acts on receptors in the zona glomerulosa to trigger production and release of aldosterone
- Aldosterone then acts mainly on the distal convoluted tubule to retain sodium in exchange for potassium and hydrogen ions
Note that renin release is also triggered if the macula densa detects low salt load in the distal tubule. Usually the low salt load is because there's reduced filtration, due to low blood pressure.
When it goes wrong
If you know about Conn's, Cushing's and Addison's then you're doing alright, because that's about it.
Conn's syndrome
- Primary hyperaldosteronism
- Hypertension (due to hypernatraemia and fluid retention, and also a bit of vasoconstriction directly caused by aldosterone)
- Hypokalaemia
- Alkalosis
- (Note that secondary hyperaldosteronism is the same but is due to high renin, rather than an intrinsic adrenal pathology)
Cushing's syndrome
- High cortisol (Cushing's disease is specifically due to ACTH-secreting pituitary tumour)
- Hypertension
- Diabetes
- Bruising
- Characteristic appearance (moon facies, buffalo hump)
- Hypokalaemia (mineralocorticoid activity)
Addison's disease
- Hypoadrenalism
- Low cortisol and often low aldosterone
- Hypoglycaemia
- Hyponatraemia
- Hyperkalaemia
- Uraemia
- Dehydration
- Hypotension
Useful Tweets
Anaesthesia, analgesia and the surgical stress response
— British Journal of Anaesthesia (@BJAJournals) September 11, 2020
Plasma cortisol levels can remain elevated for 7 days after major surgery; Explore the hypothalamic-pituitary -adrenal (HPA) axis@barbaracusack89 @Mater_ICU#BJAEducationhttps://t.co/H5lS2HKlLp pic.twitter.com/MIzU2oFTUV
💊➡️Along with sedation/anesthesia, etomidate is also used as a steroidogenesis inhibitor - making it useful for hypercortisolism when oral administration is not possible. It suppresses corticosteroid synthesis in the adrenal cortex by reversibly inhibiting 11β-hydroxylase.
— PharmaFactz (@PharmaFactz) April 22, 2020
Replacing steroids
- You can't use dexamethasone in patients with primary adrenal insufficiency as it doesn't have any mineralocorticoid activity - use hydrocortisone
- The safest regime for anyone who usually take 5mg prednisolone per day equivalent or more is 100mg hydrocortisone at induction followed immediately by 200mg over 24 hours, continued until the patient can take double their usual oral dose
References and Further Reading:
- Melanie Davies, FRCA, Jonathan Hardman, DM FRCA, Anaesthesia and adrenocortical disease, Continuing Education in Anaesthesia Critical Care & Pain, Volume 5, Issue 4, August 2005, Pages 122–126, https://doi.org/10.1093/bjaceaccp/mki033