NAP 5

Take home messages
- Overall incidence is 1:19 000
- Awareness is significantly more likely in patients who are given neuromuscular blockade (1:8 000)
- Awareness is much lower in non-paralysed patients (1:136 000)
- Patients that experience awareness under general anaesthesia are prone to developing PTSD and depression
Anaesthesia.
- An - without
- Aesthesia - sensation or perception
Kind of in the name really.
We don't want our patients to be aware of the unpleasant things surgeons do when they're not looking. They might be awake if we're electing to use regional anaesthesia, but we generally don't want them to be able to perceive the experience in any meaningful manner.
When it comes to good old general anaesthesia - we concern ourselves with whether there is any chance the patient is actually aware of what's going on.
What is awareness?
- Awareness can be explicit or implicit
- Explicit awareness involves the ability to recall the situation
- Implicit awareness means there is no conscious recollection of the event, however the patient's behaviour and feelings may be affected at a subconscious level
- Frequency is approximately 1 in 500 to 1 in 1000 according to patients, but as low as 1 in 15000 according to anaesthetic practitioners
According to the fifth national audit project (NAP5), nearly half (47%) of cases of awareness involved vague memories of hearing noises or feeling sensations that weren't overtly distressing.
However the remaining 53% reported significant distress, including pain and paralysis, and these were associated with long term psychological impact including:
- PTSD and flashbacks
- Fear of surgery
- Insomnia
Who is at risk?
There are two types of list in anaesthesia:
- Those that can be cancelled
- Those that can be categorised
This is one of the latter.
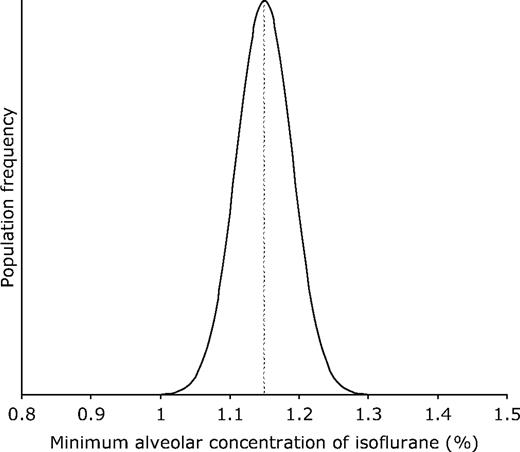
Patient factors
- Previous awareness
- Chronic sedative use (alcohol, benzodiazepines)
- Sepsis
- Hyperthyroid
- Hypermetabolic state (including anxiety)
- Smoker
- Beta-blockers
- Diabetes with autonomic neuropathy
- Chronic pain syndrome
- Female
- Middle aged
Anaesthetic factors
- Unexpected difficult airway with multiple intubation attempts
- TIVA
- Emergency intubation with rapid sequence induction
- Use of thiopental
- Use of paralysis
- Inadequate use of reversal and muscle stimulator
- Junior anaesthetist
- Lack of depth of anaesthesia monitoring
- Transfer of patient from anaesthetic room to theatre
Surgical factors
- Emergency surgery
- Substantial blood loss
- Cardiac surgery
- Obstetric surgery (particularly c-section)
- Paediatric surgery
- Bronchoscopy
What the National Audit Project found
- The estimated incidence of patient reports of AAGA was ~1:20,000 anaesthetics. However, there was considerable variation in this incidence when subtypes of anaesthetic techniques or subspecialties were taken into account.
- The incidence of reports of AAGA when neuromuscular blockade was used was ~1:8,000
- When no paralysis was involved this was ~1:136,000
- The incidence of reports from cardiothoracic anaesthesia (~1:8,600) closely resembled that for neuromuscular blockade.
- The incidence of reports of AAGA after general anaesthetic
- Caesarean section was much higher, ~1:670
- Almost two-thirds of AAGA experiences arose at induction and emergence
- One third of AAGA events arose during the maintenance phase of anaesthesia
Useful Tweets and Resources

References and Further Reading

Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.


