A-a gradient

Key take home points
- A-a gradient gives you a clue as to the cause of hypoxia
- A normal gradient essentially rules out V/Q mismatch, diffusion defects and increased oxygen extraction as the cause
- a/A ratio may be more useful in patients with high, or changing, FiO2
- Don't confuse it with PaO2/FIO2, which is used to calculate disease severity in ARDS
The brain likes oxygen
In fact, most of the body does, so it's nice to know that the patient is getting enough. But we can't reliably, safely or easily measure oxygen within the vital organs themselves, so we have to rely on surrogate measures to reassure ourselves that they're sufficiently oxygenated.
We can measure oxygen 'levels' in the following ways:
- The FiO2 or percentage concentration of oxgyen that the patient is being given to breathe in
- The partial pressure in kilopascals (kPa) of the oxygen in the patient's blood
- The percentage saturation of haemoglobin in the peripheral circulation
It's really hard to measure the partial pressure of oxygen in the patient's alveolus, so we have to extimate it using the alveolar gas equation.
Concentration vs Partial pressure
This often gets confused and it's important to understand the difference.
What matters is the partial pressure of oxygen, which is the pressure exerted on the walls of the container or blood vessel by the oxygen molecules, because that generates the pressure gradient that ensures the molecules will diffuse into the mitochondria where they're needed.
We often measure concentration of oxygen when we talk about the gas mixture that the patient is breathing in and out, because it's often easier to measure that way, but it can be misleading:
- If the atmospheric pressure is 100 kPa, then 21% oxygen is 21 kPa
- If the atmospheric pressure is 50 kPa, then 21% oxygen is 10.5 kPa
- At 8,000 metres altitude, atmospheric pressure is 35.6 kPa, giving an unsurvivable oxygen level of 7.5 kPa, hence this altitude is referred to as the 'death zone'
In each of these scenarios, you're breathing '21%' oxygen, but the amount of oxygen is vastly different.
Enter the oxygen cascade
If you want fluid to move, you need to generate a pressure gradient, and the same applies to oxygen.
The oxygen cascade is the stepwise drop in partial pressure of oxygen as it waterfalls through the respiratory system and into the blood, where it is gradually absorbed into the tissues, leaving a relatively paltry quantity for the overworked mitochondria to use.
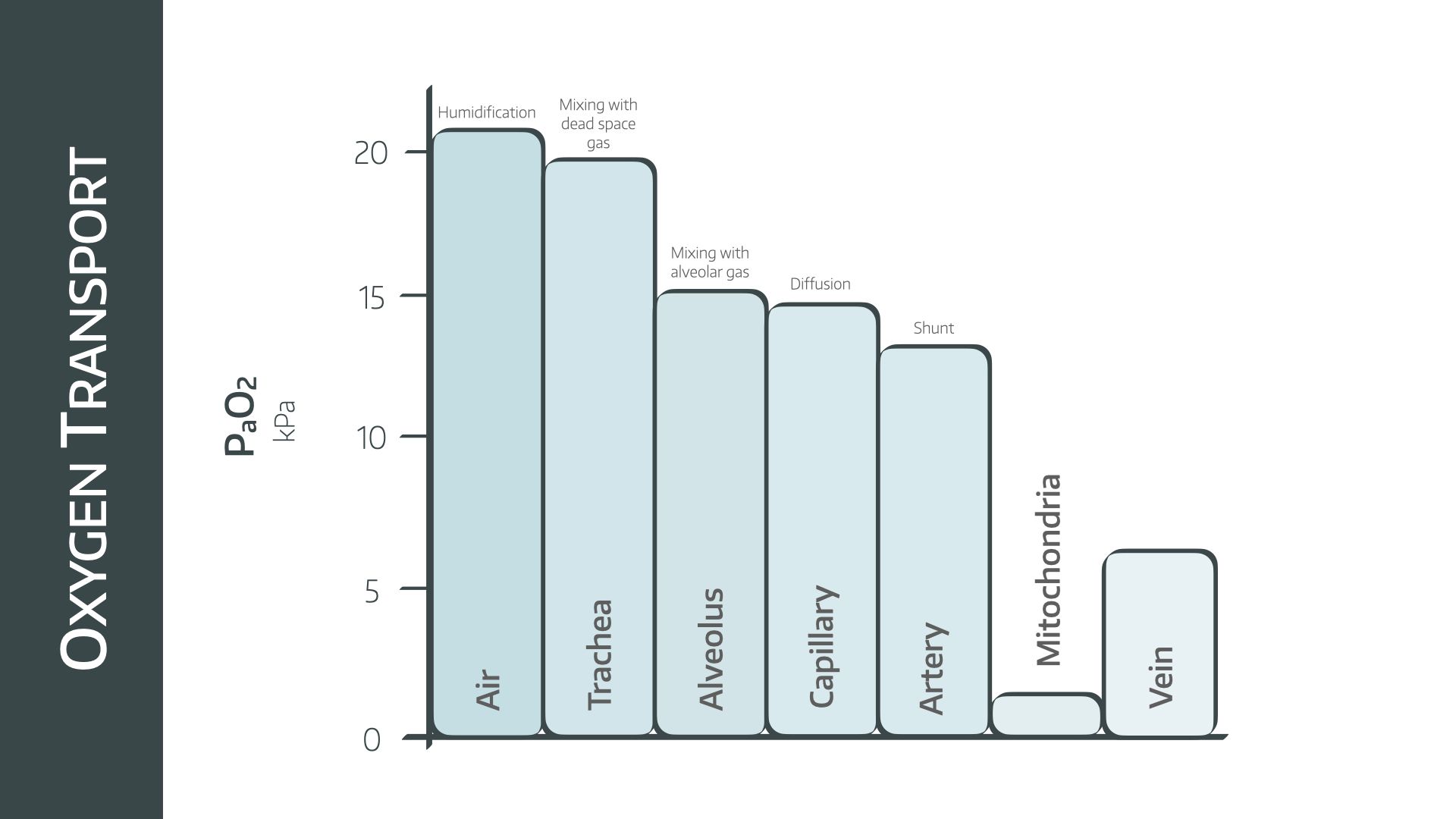
At each step along the way, inefficiencies of transfer, consumption by tissues and displacement by other gases cause the partial pressure of oxygen to drop steadily.
Enter the A-a gradient
It's a simple enough idea - you minus the arterial oxygen tension (in kPa or mmHg) from the alveolar oxygen tension and it tells you essentially how efficiently oxygen is moving across the alveolar membrane to the capillaries, as well as how much shunt you're likely to be dealing with.
Now you may quickly realise that while we can measure PaO2 relatively easily with an arterial blood gas machine, it is vastly more difficult to measure the oxygen tension in the alveolus.
We therefore estimate it using the alveolar gas equation
PAO2 is estimated as PiO2 - PaCO2/0.8
- PiO2 = partial pressure of inspired oxygen
- PaCO2 = arterial carbon dioxide tension
- 0.8 = estimated respiratory quotient
You've probably worked out that if the lungs aren't working well, this number is going to increase, as there is less oxygen on the arterial side, and more remaining trapped in the alveolus.
Thus if a patient is hypoxic, they will either have a raised A-a gradient because the lungs aren't working all that well, or a normal A-a gradient, because the hypoxia is caused by another problem not involving the alveolar membrane or shunt.
Normal A-a gradient
- Lungs giving oxygen to the blood well, but lungs not receiving enough oxygen in the first place
- Either due to alveolar hypoventilation, which will usually have a raised CO2
- Or due to low PiO2 (hypoxic gas mixture, high altitude) which will have a normal CO2
Raised A-a gradient
- Ventilation perfusion mismatch (either shunt or deadspace caused by a respiratory or cardiovascular pathology)
- Severe right to left shunt (congenital cardiac)
- Increased oxygen consumption and extraction (sepsis, hypermetabolic state)
Other factors affecting A-a gradient
- Age - for each ten years of life, A-a gradient increases by around 1 mmHg or 0.13 kPa
- If you're measuring in mmHg then a normal A-a gradient can reasonably be estimated by Age/4 + 4 (which may feel weirdly familiar)
The main issue
The main drawback of the A-a gradient as a measuring tool is that it is extremely sensitive to changes in FiO2.
- If you have a patient on room air with a PAO2 of 13 kPa and a PaO2 of 9 kPa, then their A-a gradient is 4 kPa - raised but not enormous
- If you then stick them on 100% oxygen, and give them a PAO2 of 85 kPa, their PaO2 will probably rise to around 60 kPa, giving an A-a gradient of 25 kPa - enormous
Their gradient has gone from slightly abnormal to very abnormal but their pathophysiology hasn't necessarily changed - it's just because the FiO2 is much higher.
What about a/A ratio?
This is a different way of expressing essentially the same information, but it has the benefit of being less affected by changes in FiO2.
Instead of subtracting the arterial from the alveolar oxygen tensions, you simply divide the arterial by the alveolar tension instead.
- PaO2/PAO2
This gives you a fraction, and over 0.75 is normal.
(While an abnormal A-a gradient will be high, an abnormal a/A ratio will be low, because it is a fraction with PaO2 as the numerator, rather than a difference between the two terms)
If we take the same patient as before:
- Patient on room air with a PAO2 of 13 kPa and a PaO2 of 9 kPa, then their a/A ratio is 9/13 = 0.7
- If you then stick them on 100% oxygen, and give them a PAO2 of 85 kPa, their PaO2 will probably rise to around 60 kPa, giving an a/A ratio of 60/85 = 0.7
Seems to us that this is probably a more sensible tool to use, as it remains consistent with the patient's pathology, rather than fluctuating wildly depending on what FiO2 you're giving.
Useful resources and further reading